
Immunotherapy in head and neck cancer
Introduction
Head and neck cancers comprise a diverse set of malignancies that originate from nasopharynx, oral cavity, oropharynx, hypopharynx, larynx, and salivary gland. It is estimated that they will account for 61,760 new cancer cases and 13,190 cancer deaths in the United States in 2016 (1). Besides tumors of salivary glands, the majority of head and neck cancers are squamous cell carcinomas and is the focus of this article.
Tobacco (including smokeless tobacco) and alcohol use are the most predominant risk factors for head and neck squamous cell carcinoma (HNSCC) and they work synergistically. Human papillomavirus (HPV) infection is now widely accepted as another cause for HNSCC, particularly in the oropharynx, with an increasing incidence in developed countries (2,3). Epstein-Barr virus (EBV), another oncogenic virus, is associated with endemic nasopharyngeal cancer in the Mediterranean and Far East (4).
For localized disease without detectable lymph node involvement, surgery or radiotherapy are effective treatment options. Radiation therapy is preferred for laryngeal cancer to preserve vocal cord function whereas surgery is recommended for small lesions in the oral cavity to avoid long-term complications associated with radiation such as xerostomia and severe dental decay. However, two-third of patients with HNSCC present with stage III or IV disease. Despite optimal local therapy, 30–50% of patients will have local or regional recurrence (5). Patients with locally or regionally advanced disease, that is, disease with a large primary tumor and/or lymph node involvement, are treated with curative intent with combined-modality therapy including surgery, radiation, and/or chemotherapy. Nearly a third of all patients with HNSCC will eventually develop distant metastases. The cornerstone of recurrent or metastatic HNSCC treatment is palliation with a platinum-based therapy (6). Cetuximab, an epidermal growth factor receptor (EGFR) inhibitor, was approved by the U.S. Food and Drug Administration (FDA) in 2011 for recurrent or metastatic HNSCC as it demonstrated survival superiority when used with platinum plus 5-fluorouracil (5-FU) (7). Nonetheless, recurrent or metastatic HNSCC still has a poor prognosis with low response rate to current systemic treatment (methotrexate, 5-FU, cisplatin/carboplatin, docetaxel/paclitaxel, or cetuximab) and short duration of response with a median survival between 6 to 10 months (8).
Head and neck cancer treatment can cause significant side effects. Its close proximity to vital organs for speech, swallow, and breathing impacts patient’s quality of life after surgical resection or radiation. Radiation therapy can be limited by acute oral mucositis and has long-term complications including loss of taste, decreased tongue mobility, xerostomia, and neck fibrosis (9,10). Complications of chemotherapy vary with specific regimen but frequently include myelosuppression, nausea and vomiting, nephrotoxicity and ototoxicity (platinum-based), and neuropathy (taxanes). Adverse effects with cetuximab include dermatological toxicity (e.g., pruritus, rash, nail changes), diarrhea, and infusion reactions (11). Severe hypomagnesemia and cardiac arrest can also occur.
Despite significant advancements in treatment of HNSCC in recent decades such as transoral robotic surgery (TORS), more precise intensity-modulated radiation (IMRT), and cetuximab, morbidity and mortality for patients with HNSCC, especially recurrent or metastatic HNSCC, remains high. Agents with less toxicity and better efficacy are needed. The FDA recently granted accelerated approval to pembrolizumab, a checkpoint inhibitor with improved side effect profile, tolerability, and promising durable antitumor activity, for second-line recurrent or metastatic HNSCC treatment. In this article, we will review immune escape mechanism in HNSCC, FDA approval for pembrolizumab, and latest developments in immunotherapy in HNSCC with a focus on pembrolizumab and checkpoint inhibitors, therapeutic cancer vaccines, and adoptive cellular therapies.
Immune escape in HNSCC
HNSCC is known to be an immunosuppressive disease with spontaneous apoptosis and down-regulation of effector T cells (12-14), defective antigen-processing mechanism, and thus impaired recognition of cancer cells by T cells (15), lower absolute lymphocyte counts (16), and compromised natural killer cell function (17). Patients who are immunosuppressed either with HIV infection or post-solid organ transplant are at increased risk of developing HNSCC (18-20).
The lack of immune control has been recognized as an emerging hallmark of cancer (21). Allison and his colleagues found that simply occupying T-cell antigen receptor (TCR) is not sufficient to fully activate T-cells; a second signal such as binding of T-cell CD28 molecule is necessary (22). This led to the discovery of various co-stimulatory receptors and co-inhibitory receptors for the regulation of T-cell activation. Perhaps the need for two immunologic signals, co-stimulatory/co-inhibitory signals, in addition to binding of TCR, helps to prevent overacting inflammatory response to a stimuli or mistaking self as a dangerous invader while providing appropriate protection to the host. Besides CD28, multiple other co-stimulatory/activating receptors have also been identified, including CD137, CD40, OX40 (CD134), and lymphocyte activation gene-3 (LAG-3) (23,24). Co-inhibitory receptors are also known as immune checkpoints and are responsible for preventing chronic autoimmune or inflammatory state. Some cancer cells manage to present certain immune checkpoints and by doing so skip the immune surveillance. By inhibiting immune checkpoints, one can unblock the negative immune regulation and allows the immune system to fight cancer.
Two of the most studied checkpoint mechanisms are cytotoxic T-lymphocyte-associated protein-4 (CTLA-4) and programmed cell death-1 (PD-1) receptors. CTLA-4 binds to the same ligands (CD80 and CD86) as does CD28 do but with higher affinity; therefore, the presence of CTLA-4 overcomes effects of stimulatory CD28 and causing immune suppression (25). PD-1 receptors present on the surface of T lymphocytes and when activated, inhibit T-cell activation (26). PD ligand 1 (PD-L1) is the main ligand for PD-1 and can be found on antigen presenting cells as well as tumor cells. Binding of PD-L1 to PD-1 activates the latter and results in down regulation of immune function. PD-1 has another ligand called PD ligand 2 (PD-L2) and has similar effect as PD-L1. Both the CTLA-4 and PD-1:PD-L1 pathways have been shown to be commonly present in HNSCC (27,28).
Immunotherapy—checkpoint inhibitors
In August 2016, the FDA granted accelerated approval for pembrolizumab (Keytruda®, Merck & CO. Inc., Kenilworth, USA) in treatment of recurrent or metastatic HNSCC with progression on or after platinum-containing chemotherapy (29). This indication is based on tumor response rate and durability of response observed from a multicenter, nonrandomized, open-label phase 1b study, KEYNOTE-012 (NCT01848834). The recommended dose is 200 mg every 3 weeks administered as an intravenous infusion over 30 minutes.
Pembrolizumab is an IgG4 monoclonal antibody against PD-1 receptor therefore blocks tumor cell’s immune-suppressing ligands, PD-L1 and PD-L2, from interacting with PD-1 on T cell and helps to restore immune response. It has been approved previously by the FDA for patients with unresectable or metastatic melanoma and in patients with metastatic non-small cell lung cancer (NSCLC) who have positive PD-L1 expression. KEYNOTE-012 study explored the use of pembrolizumab in patients with other advanced solid tumors including triple-negative breast cancer, HNSCC, urothelial tract cancer, and gastric cancer (NCT01848834). A total of 192 patients aged 18 years or older with confirmed diagnosis of recurrent (not amenable to locally curative options) or metastatic HNSCC received pembrolizumab in this study (30). Exclusion criteria include active autoimmune disease that required immunosuppression, evidence of interstitial lung disease, ECOG ≥2, CNS metastases, HIV, hepatitis B or C, and additional progressing malignancies (31). The initial (I) cohort enrolled PD-L1-positive patients (n=60) whereas expansion (E) cohort enrolled patients regardless of PD-L1 status (n=132). Pembrolizumab 10 mg/kg every 2 weeks (I) or 200 mg every 3 weeks was given for up to 24 months until disease progression, or unacceptable toxicity. Accelerated approval by the FDA was granted as the clinical trial showed an objective response rate (ORR) of 16% (95% CI, 11–22%) in the 174 patients (I =53, E =121) who had progression after platinum-containing chemotherapy (32). Twenty-three (82%) of responding patients have responses of 6 months or longer, with several lasting for more than 2 years and a complete response rate of 5%. Similar ORR was demonstrated in both the initial cohort and expansion cohort when calculated separately regardless of PD-L1 status (31,33). The median response duration has not been reached. It was also noticed that ORR was 22% (95% CI, 12–34%) in HPV-positive patients and 16% (95% CI, 10–23%) in HPV-negative patients when counting all responding patients regardless of previous treatment status (30). However, caution should apply when reaching final conclusions on how HPV status affects response rate to PD-1 inhibitor given the small number of patients.
Pembrolizumab has a relatively tolerable side effect profile. Treatment-related adverse events occurred in 122 (64%) of the patients (30). Adverse events experienced by patients with HNSCC were similar to those occurring in patients with melanoma or NSCLC, with the addition of facial edema (10% all grade, 2% grades 3–4). Most common adverse reactions (reported in ≥20% of patients) were fatigue, decreased appetite, and dyspnea; 12% patients had grade 1–2 pruritus (31). Of the 192 patients receiving pembrolizumab for recurrent or metastatic HNSCC, 23 (12%) had a grade 3–4 adverse event including increased alanine aminotransferase, increased aspartate aminotransferase, hyponatremia, atrial fibrillation, congestive heart failure, diarrhea, lymphopenia, musculoskeletal pain, and neck abscess. Clinically significant immune-mediated adverse reactions such as endocrinopathies (hypophysitis, thyroid disorders, and type 1 diabetes mellitus), colitis, hepatitis, nephritis, and pneumonitis can also be associated with pembrolizumab (34). Immune-related adverse events usually are reversible if recognized promptly, however delayed recognition can lead to severe toxicity (35). Depending on the grade of toxicity, treatments involve withholding or permanently discontinuing the medication and/or administration of corticosteroids for immunosuppression.
Pembrolizumab in head and neck cancer is currently under further investigation in multiple advanced trials. Preliminary results from the first 50 out of 172 patients enrolled in a phase 2 trial (KEYNOTE-055, NCT02255097) evaluating pembrolizumab for HNSCC with progression after platinum and cetuximab found an ORR of 18.0% (95% CI, 8.6–31.4%) confirming findings from KEYNOTE-012 (36). One (2%) patient died because of a treatment-related adverse event in this trial whereas none in KEYNOTE-012. As a part of the accelerated approval condition, Merck is conducting a multicenter, randomized phase 3 trial to assess if pembrolizumab has superiority over standard therapy for recurrent or metastatic HNSCC with disease progression on or after platinum-containing chemotherapy (KEYNOTE-040, NCT02252042). The study uses pembrolizumab as the experiment group with investigator’s choice (IC) of standard treatment (methotrexate, docetaxel, or cetuximab) as the control arm and will be looking at overall survival (OS) for primary endpoint. KEYNOTE-048 is another phase 3 clinical trial currently recruiting patients with recurrent or metastatic HNSCC with no prior systemic therapy (NCT02358031). This study will be evaluating pembrolizumab as first line treatment for recurrent or metastatic HNSCC with enrolled patients randomized to either of the three groups—pembrolizumab monotherapy, pembrolizumab + platinum + 5-FU, or cetuximab + platinum + 5-FU. Pembrolizumab also demonstrated promising antitumor activity in treatment-refractory advanced (unresectable and/or metastatic) salivary gland carcinoma cohort in a phase 1b clinical trial (KEYNOTE-028, NCT02054806) and is under active investigation in the phase 2 KEYNOTE-158 trail (NCT02628067) (37).
Nivolumab (Opdivo®, Bristol-Myers Squibb, New York City, USA) is another IgG4 monoclonal antibody against PD-1 receptor that has shown promise in HNSCC. More specifically, nivolumab was found to improve OS and have better tolerability when compared with methotrexate, docetaxel, or cetuximab in patients with platinum-refractory recurrent or metastatic HNSCC in a randomized, open-label, phase 3 trial CheckMate-141 (NCT02105636) (38). A total of 361 patients aged 18 years or older with recurrent or metastatic HNSCC who had disease progression within 6 months of platinum-based chemotherapy and ECOG 0–1 were randomized 2:1 to nivolumab (3 mg/kg intravenously every 2 weeks) or single-agent of IC (methotrexate, docetaxel, or cetuximab). A 30% reduction in risk of death was seen in nivolumab-treated group with a median OS of 7.5 months (95% CI, 5.5–9.1) compared to 5.1 months (95% CI, 4.0–6.0) for IC. Nivolumab was effective for HNSCC regardless of PD-L1 status, however there was a positive correlation between degree of PD-L1 expression and medication response as ORR for nivolumab-treated patients with PD-L1 ≥1%, 5%, and ≥10% was 18.2%, 25.9%, and 32.6%, respectively, and 3.3%, 2.3%, and 2.9% for IC. Treatment-related adverse events occurred in 58.9% of patients on nivolumab vs. 77.5% of patients on IC; of which 13.1% in nivolumab vs. 35.1% on IC were grade 3–4. Given these data, the FDA has granted priority review to nivolumab for recurrent or metastatic HNSCC and will be announcing their decision regarding approval no later than November 11, 2016 (39).
In addition to PD-1 inhibitors, monoclonal antibodies that target PD-L1 are under investigation. Currently there is a phase 2 study evaluating durvalumab, an Fc optimized monoclonal antibody against PD-L1, as monotherapy for recurrent or metastatic HNSCC (NCT01693562) and more studies looking into the effect of combining durvalumab with other therapies as discussed in later sections. Both avelumab and atezolizumab are IgG1 anti-PD-L1 monoclonal antibodies; both have ongoing phase 1 trials evaluate use in patients with advanced solid tumors including HNSCC (NCT01772004 and NCT01375842, respectively). A phase 2 trial of avelumab in patients with recurrent or metastatic nasopharyngeal carcinoma is soon to open (NCT02875613).
Ipilimumab (Yervoy®, Bristol-Myers Squibb) is an IgG1 monoclonal antibody against CTLA-4 that has received the FDA approval for metastatic melanoma, and is currently being evaluated in combination with cetuximab and IMRT for locally advanced HNSCC (NCT01860430, NCT01935921). Ipilimumab blocks the interaction of CTLA-4 with its ligands, CD80/CD86, and removal of this negative regulation subsequently augments T-cell activation and proliferation. Compared to PD-1 inhibitors, ipilimumab is associated with more severe immune-related toxicity (40). Another anti-CTLA-4 antibody that has been evaluated in several clinical trials in HNSCC is tremelimumab (NCT02319044, NCT02369874, NCT02551159).
Immunotherapy—therapeutic vaccine
An increasing number of HNSCC are virally mediated with exogenous proteins and therefore place them at a unique advantage of potential benefit of therapeutic vaccination as a treatment or prevention option. Commercially available HPV vaccines (Cervarix®, GlaxoSmithKline, Philadelphia, USA and Gardasil®, Merck & CO. Inc.) are highly effective in preventing ano-genital cancers but not effective in treating existing HPV infections or HPV-associated malignant lesions. Vaccine efficiency in reducing HPV-associated HNSCC incidence is currently being evaluated; it will take longer to collect the data as HPV oropharyngeal cancers can take years to develop after initial infection (41). HPV infected cells do not express detectable level of capsid antigens, as a result HPV prophylactic vaccine does not work for preexisting HPV lesions as the vaccine consists of viral-like particles and works by inducing strong antibodies against capsid antigen L1 in recipients. HPV infected cells, however, do express E6 and E7 proteins which can be used as targets in the development of HPV therapeutic vaccines. Both viral E6 and E7 proteins are expressed early and throughout the course of infection and participate in oncogenesis (42,43).
There are products advancing to clinical trials for HPV therapeutic vaccine. VGX-3100 is a synthetic plasmid targeting HPV-16 and HPV-18 E6 and E7 protein. A phase 2 study showed histopathological regression in women with cervical intraepithelial neoplasia 2/3 treated with VGX-3100 delivered by electroporation (44). Patients treated with VGX-3100 who had lesion regression were also found to have increased CD8-positive infiltrates compared to no change in intensity of CD8-positive infiltrates in placebo group patients who had histopathological regression. Even though the response rate in these pre-malignancies was low (50% in experimental arm vs. 30% in placebo group), it was the first trial to successfully demonstrate that therapeutic vaccines’ ability in inducing immunity in patients with existing HPV-associated lesions. A phase 1/2a trial looking into safety, tolerability, and immunogenicity of VGX-3100 plus adjuvant interleukin-12 in patients with HPV-associated HNSCC is undergoing (NCT02163057).
Another method of viral protein delivery that is under investigation is called ADXS11, a live attenuated Listeria monocytogenes based immunotherapy that secretes antigen-adjuvant fusion protein consisting of HPV-16 E7. One phase 1 trial of ADXS11 in HPV-positive oropharyngeal cancer was terminated early due to dose limiting toxicity (NCT01598792) and a phase 2 trial studying modified ADXS11 as neoadjuvant to ablative TORS for patients with newly diagnosed HPV-16-positive oropharyngeal cancer is currently recruiting (NCT02002182).
In addition to viral protein E6/E7, cellular protein p16 has also been an interest of therapeutic vaccine development. Limited success with E6 and E7 vaccines could be partially due to immunoevasion and immunoediting against the viral antigen in patients with persistent HPV infections (45). Cyclin-dependent kinase inhibitor p16 is consistently overexpressed in HPV-associated cancers. The theoretical risk of systemic tissue-destructive autoimmune reaction with p16 vaccine is low given expression level of p16 in normal tissue is very low and may be contributing to aging-related pathologies (46). In the phase 1/2a clinical trial no unexpected serious adverse reaction was found (NCT01462838). Of the 26 patients with advanced HPV-associated malignancies enrolled in the study, seven have HNSCC and all noticed to have immune response after vaccination. The best clinical response observed in this trial was stable disease; tumor regression was not seen, potentially due to the advanced stage of diseases in recruited patients. Another small phase 1 trial is evaluating a p16_37-63 peptide vaccination with cisplatin-based chemotherapy to improve the prognosis and quality of life for patients with HPV-positive cancers (NCT02526316).
Immunotherapy—adoptive T-cell therapy
Before development of immune checkpoint inhibitors and therapeutic cancer vaccines, interests have been drawn to passive immunization, also known as adoptive T-cell transfer or therapy. Adoptive T-cell therapy involves harvesting and ex vivo expansion of patient’s own tumor antigen specific T-cells, followed by reinfusion into the patient in hopes of enhancing a patient’s antitumor immune response (47). It has potential success in HNSCC as HPV- and EBV-associated diseases have foreign (viral) antigens that are excellent targets. It has been demonstrated that EBV-specific cytotoxic T lymphocytes (CTL) therapy has antitumor activity in advanced nasopharyngeal cancers. However, the use of lymphodepleting chemotherapy prior to CTL infusion did not enhance clinical benefit (48). Clinical benefit of EBV-specific CTL in recurrent or metastatic nasopharyngeal cancer was further demonstrated in a phase 2 study where it was used as first-line therapy in combination with chemotherapy (49). Even though specific data regarding HPV-positive HNSCC is not available at this time, adoptive T-cell therapy has showed some promising results in other HPV-associated malignancy (50). In this small phase 2 study, three out of nine patients with platinum-refractory metastatic cervical cancer experienced objective tumor responses with two complete responses over 1 year. Similar phase 2 with metastatic HPV-associated carcinoma including oropharyngeal cancer has been done and is in final data collection stage (NCT01585428).
Rationale of combining immunotherapies
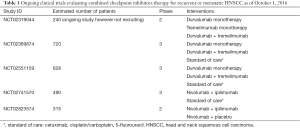
The new paradigm of checkpoint blockade is promising and combination of different immunotherapies opens up more potential therapeutic interventions. Different groups of checkpoint inhibitors have distinct immunologic effects; therefore by combining them, one can influence different phases of T-cell induction and maturation to achieve a stronger response. For example, blockade of PD-1 leads to gene changes regarding cytolysis and natural killer cell function whereas CTLA-4 blockade induces a proliferative upregulation of a transitional memory T cell subset (51). Higher response rate indeed were observed in patients with advanced melanoma treated with combined nivolumab and ipilimumab than either approach alone (52). Current clinical trials assessing the efficacy of anti-PD-1 and anti-CTLA-4 antibodies combination in recurrent or metastatic HNSCC are listed below (Table 1).
Full table
Conclusions
Significant advancements have been made in immunotherapy treatments for advanced HNSCC treatment. Better understanding of immune evasion of tumors offers more treatment options particularly with the checkpoint inhibitors. The anti-PD-1 antibody pembrolizumab has recently been granted accelerated approval for recurrent or metastatic HNSCC by the FDA as it demonstrated durable response rate. Further studies are ongoing to assess potential survival benefit. Another anti-PD-1 antibody, nivolumab, is currently undergoing FDA priority review and the decision regarding its approval is pending. Other checkpoint inhibitors (anti-PD-L1, anti-CTLA-4 antibodies) as well as therapeutic vaccine and adoptive T-cell therapy all show promising results. Clinical trial participation for recurrent or metastatic HNSCC patients should be encouraged.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Marin Feldman Xavier) for the series “Advances on Clinical Immunotherapy” published in Translational Cancer Research. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.01.14). The series “Advances on Clinical Immunotherapy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin 2016;66:7-30. [Crossref] [PubMed]
- Gillison ML, Koch WM, Capone RB, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst 2000;92:709-20. [Crossref] [PubMed]
- Chaturvedi AK, Anderson WF, Lortet-Tieulent J, et al. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J Clin Oncol 2013;31:4550-9. [Crossref] [PubMed]
- Raab-Traub N. Epstein-Barr virus in the pathogenesis of NPC. Semin Cancer Biol 2002;12:431-41. [Crossref] [PubMed]
- McQuade LL, Gunn GB, William WN, et al. Head and neck cancer. In: Kantarjian HM, Wolff RA. editors. The MD Anderson Manual of Medical Oncology. 3rd edition. New York: McGraw-Hill Education, 2016;379-400.
- Sacco AG, Cohen EE. Current treatment options for recurrent or metastatic head and neck squamous cell carcinoma. J Clin Oncol 2015;33:3305-13. [Crossref] [PubMed]
- U.S. Food & Drug Administration. Cetuximab (Erbitux). Available online: http://www.fda.gov/AboutFDA/CentersOffices/OfficeofMedicalProductsandTobacco/CDER/ucm278957.htm
- Baxi S, Fury M, Ganly I, et al. Ten years of progress in head and neck cancers. J Natl Compr Canc Netw 2012;10:806-10. [PubMed]
- Mallick S, Benson R, Rath GK. Radiation induced oral mucositis: a review of current literature on prevention and management. Eur Arch Otorhinolaryngol 2016;273:2285-93. [Crossref] [PubMed]
- Straub JM, New J, Hamilton CD, et al. Radiation-induced fibrosis: mechanisms and implications for therapy. J Cancer Res Clin Oncol 2015;141:1985-94. [Crossref] [PubMed]
- Erbitux® (cetuximab). Indianapolis (IN): Eli Lilly and Company; 2015. Available online: http://pi.lilly.com/us/erbitux-uspi.pdf
- Hoffmann TK, Dworacki G, Tsukihiro T, et al. Spontaneous apoptosis of circulating T lymphocytes in patients with head and neck cancer and its clinical importance. Clin Cancer Res 2002;8:2553-62. [PubMed]
- Reichert TE, Strauss L, Wagner EM, et al. Signaling abnormalities, apoptosis, and reduced proliferation of circulating and tumor-infiltrating lymphocytes in patients with oral carcinoma. Clin Cancer Res 2002;8:3137-45. [PubMed]
- Chikamatsu K, Sakakura K, Whiteside TL, et al. Relationships between regulatory T cells and CD8+ effector populations in patients with squamous cell carcinoma of the head and neck. Head Neck 2007;29:120-7. [Crossref] [PubMed]
- López-Albaitero A, Nayak JV, Ogino T, et al. Role of antigen-processing machinery in the in vitro resistance of squamous cell carcinoma of the head and neck cells to recognition by CTL. J Immunol 2006;176:3402-9. [Crossref] [PubMed]
- Kuss I, Hathaway B, Ferris R, et al. Decreased absolute counts of T lymphocyte subsets and their relation to disease in squamous cell carcinoma of the head and neck. Clin Cancer Res 2004;10:3755-62. [Crossref] [PubMed]
- Bauernhofer T, Kuss I, Henderson B, et al. Preferential apoptosis of CD56 natural killer cell subset in patients with cancer. Eur J Immunol 2003;33:119-24. [Crossref] [PubMed]
- Dʼsouza G, Carey T, William WN, et al. Epidemiology of head and neck squamous cell cancer among HIV-infected patients. J Acquir Immune Defic Syndr 2014;65:603-10. [Crossref] [PubMed]
- Jain A, Reyes J, Kashyap R, et al. What have we learned about primary liver transplantation under tacrolimus immunosuppression? Long-term follow-up of the first 1000 patients. Ann Surg 1999;230:441-8; discussion 448-9. [Crossref] [PubMed]
- Deeb R, Sharma S, Mahan M, et al. Head and neck cancer in transplant recipients. Laryngoscope 2012;122:1566-9. [Crossref] [PubMed]
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell 2011;144:646-74. [Crossref] [PubMed]
- Harding FA, McArthur JG, Gross JA, et al. CD28-mediated signalling co-stimulates murine T cells and prevents induction of anergy in T-cell clones. Nature 1992;356:607-9. [Crossref] [PubMed]
- Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 2012;12:252-64. [Crossref] [PubMed]
- Sega EI, Leveson-Gower DB, Florek M, et al. Role of lymphocyte activation gene-3 (Lag-3) in conventional and regulatory T cell function in allogeneic transplantation. PLoS One 2014;9:e86551 [Crossref] [PubMed]
- Leach DR, Krummel MF, Allison JP. Enhancement of antitumor immunity by CTLA-4 blockade. Science 1996;271:1734-6. [Crossref] [PubMed]
- Ribas A. Tumor immunotherapy directed at PD-1. N Engl J Med 2012;366:2517-9. [Crossref] [PubMed]
- Erfani N, Khademi B, Haghshenas MR, et al. Intracellular CTLA4 and regulatory T cells in patients with laryngeal squamous cell carcinoma. Immunol Invest 2013;42:81-90. [Crossref] [PubMed]
- Lyford-Pike S, Peng S, Young GD, et al. Evidence for a role of the PD-1:PD-L1 pathway in immune resistance of HPV-associated head and neck squamous cell carcinoma. Cancer Res 2013;73:1733-41. [Crossref] [PubMed]
- U.S. Food & Drug Administration. Hematology/Oncology (Cancer) Approvals & Safety Notifications. Available online: http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm279174.htm
- Mehra R, Seiwert TY, Mahipal A, et al. Efficacy and safety of pembrolizumab in recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC): Pooled analyses after long-term follow-up in KEYNOTE-012. J Clin Oncol 2016;34:abstr 6012.
- Seiwert TY, Burtness B, Mehra R, et al. Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, muticentre, phase 1b trial. Lancet Oncol 2016;17:956-65. [Crossref] [PubMed]
- U.S. Food & Drug Administration. pembrolizumab (KEYTRUDA). Available online: http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm515627.htm
- Seiwert TY, Haddad RI, Gupta S, et al. Antitumor activity and safety of pembrolizumab in patients with advanced squamous cell carcinoma of the head and neck: preliminary results from KEYNOTE-012 expansion cohort. J Clin Oncol 2015;33:6008.
- Keytruda ® (pembrolizumab). Whitehouse Station (NJ): Merck Sharp & Dohme Corp; 2016. Available online: https://www.merck.com/product/usa/pi_circulars/k/keytruda/keytruda_pi.pdf
- Villadolid J, Amin A. Immune checkpoint inhibitors in clinical practice: update on management of immune-related toxicities. Transl Lung Cancer Res 2015;4:560-75. [PubMed]
- Bauml J, Seiwert TY, Pfister DG, et al. Preliminary results from KEYNOTE-055: Pembrolizumab after platinum and cetuximab failure in head and neck squamous cell carcinoma (HNSCC). J Clin Oncol 2016;34:abstr 6011.
- Cohen RB, Delord JP, Doi T, et al. Preliminary results for the advanced salivary gland carcinoma cohort of the phase 1b KEYNOTE-028 study of pembrolizumab. J Clin Oncol 2016;34:abstr 6017.
- Ferris RL, Blumenschein GR, Fayette J, et al. Further evaluations of nivolumab (nivo) versus investigator’s choice (IC) chemotherapy for recurrent or metastatic (R/M) squamous cell carcinoma of the head and neck (SCCHN): CheckMate 141. J Clin Oncol 2016;34:abstr 6009.
- Bristol-Myers Squibb. Bristol-Myers Squibb Announces Regulatory Updates for Opdivo (nivolumab) in Previously Treated Recurrent or Metastatic Squamous Cell Carcinoma of the Head and Neck. Available online: http://investor.bms.com/investors/news-and-events/press-releases/press-release-details/2016/Bristol-Myers-Squibb-Announces-Regulatory-Updates-for-Opdivo-nivolumab-in-Previously-Treated-Recurrent-or-Metastatic-Squamous-Cell-Carcinoma-of-the-Head-and-Neck/default.aspx
- Linardou H, Gogas H. Toxicity management of immunotherapy for patients with metastatic melanoma. Ann Transl Med 2016;4:272-82. [Crossref] [PubMed]
- D'Souza G, Dempsey A. The role of HPV in head and neck cancer and review of the HPV vaccine. Prev Med 2011;53:S5-S11. [Crossref] [PubMed]
- Spanos WC, Hoover A, Harris GF, et al. The PDZ binding motif of human papillomavirus type 16 E6 induces PTPN13 loss, which allows anchorage-independent growth and synergizes with ras for invasive growth. J Virol 2008;82:2493-500. [Crossref] [PubMed]
- Brehm A, Nielsen SJ, Miska EA, et al. The E7 oncoprotein associates with Mi2 and histone deacetylase activity to promote cell growth. EMBO J 1999;18:2449-58. [Crossref] [PubMed]
- Trimble CL, Morrow MP, Kraynyak KA, et al. Safety, efficacy, and immunogenicity of VGX-3100, a therapeutic synthetic DNA vaccine targeting human papillomavirus 16 and 18 E6 and E7 proteins for cervical intraepithelial neoplasia 2/3: a randomised, double-blind, placebo-controlled phase 2b trial. Lancet 2015;386:2078-88. [Crossref] [PubMed]
- Reuschenbach M, Pauligk C, Karbach J, et al. A phase 1/2a study to test the safety and immunogenicity of a p16INK4a peptide vaccine in patients with advanced human papillomavirus-associated cancers. Cancer 2016;122:1425-33. [Crossref] [PubMed]
- van Deursen JM. The role of senescent cells in ageing. Nature 2014;509:439-46. [Crossref] [PubMed]
- June CH. Principles of adoptive T cell cancer therapy. J Clin Invest 2007;117:1204-12. [Crossref] [PubMed]
- Secondino S, Zecca M, Licitra L, et al. T-cell therapy for EBV-associated nasopharyngeal carcinoma: preparative lymphodepleting chemotherapy does not improve clinical results. Ann Oncol 2012;23:435-41. [Crossref] [PubMed]
- Chia WK, Teo M, Wang WW, et al. Adoptive T-cell transfer and chemotherapy in the first-line treatment of metastatic and/or locally recurrent nasopharyngeal carcinoma. Mol Ther 2014;22:132-9. [Crossref] [PubMed]
- Stevanović S, Draper LM, Langhan MM, et al. Complete regression of metastatic cervical cancer after treatment with human papillomavirus-targeted tumor-infiltrating T cells. J Clin Oncol 2015;33:1543-50. [Crossref] [PubMed]
- Das R, Verma R, Sznol M, et al. Combination therapy with anti-CTLA-4 and anti-PD-1 leads to distinct immunologic changes in vivo. J Immunol 2015;194:950-9. [Crossref] [PubMed]
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med 2015;373:23-4. [Crossref] [PubMed]


