
Brigatinib and the new generation of ALK-inhibitors for non-small cell lung cancer
Introduction
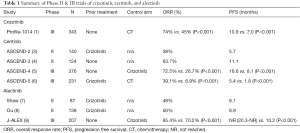
About 2–7% of non-small cell lung cancer (NSCLC) is driven by the fusion protein between echinoderm microtubule-associated protein-like 4 (EML4) and anaplastic lymphoma kinase (ALK) (1). The first ALK-inhibitor approved for the treatment of NSCLC was crizotinib with an objective response rate (ORR) up to 74%. Despite this, progression-free survival (PFS) on crizotinib is only 10.9 months, and the cancer invariably recurs with 25–50% of recurrences in the CNS (1,2) (Table 1). Given the protracted natural history of metastatic ALK-rearranged NSCLC in the CNS, treatment options aside from those causing significant neurocognitive degeneration, such as whole brain radiotherapy, are limited (10).
Full table
The limited PFS and rates of progression in the CNS have led to the development of second-generation ALK-inhibitors; results of their clinical trials are summarized in Table 1. One of these drugs, ceritinib, is FDA-approved for the treatment of ALK-rearranged NSCLC following treatment with crizotinib (4). This was based on evidence of superior second-line ceritinib to chemotherapy in crizotinib-resistant (CR) patients in ASCEND-5 (5.4 vs. 1.6 months; P<0.001)(6). Alectinib is another FDA-approved second generation ALK-inhibitor approved as first-line therapy in ALK-rearranged NSCLC. J-ALEX, a Phase III trial comparing first-line alectinib to crizotinib was terminated early from its clear benefit with a median PFS of over 20.1 months (8,9). However, resistance to these two drugs also invariably occurs. In CR patients, progression occurs even more rapidly with second-line ceritinib and alectinib than progression on first-line crizotinib; phase II trials of alectinib and Phase III trials of ceritinib in CR patients yielded PFS of only 8.1 and 5.4 months, respectively (6,7). Thus, PFS beyond one year in CR patients remains elusive.
Activity and safety of brigatinib in ALK-rearranged non-small-cell lung cancer and other malignancies: a single-arm, open-label, phase 1/2 trial (2)
Gettinger et al. present Phase I/II clinical data (NCT02094573) on the activity and safety of another novel, second generation, oral, investigational ALK-inhibitor, brigatinib (AP26113; ARIAD Pharmaceuticals, Cambridge, MA, USA) (2). Among varied dosing regimens, all eight ALK-inhibitor naïve patients with ALK-rearranged NSCLC achieved an objective response. CR trying to replace hyphen with space patients treated with brigatinib attained median PFS of 14.5 months (95% CI: 9.2 to not reached). The CNS ORR to brigatinib was similar to what has been reported in previous trials of ceritinib (45–58%) and alectinib (58%) (3,4,7,11-12). 53% of patients with measurable baseline intracranial metastatic disease responded, and 35% of patients with non-measurable baseline intracranial metastatic disease had a response to brigatinib (2).
Although brigatinib remains investigational, there is a reason to believe that it may have efficacy in patients resistant to crizotinib, ceritinib, and even alectinib. In particular, the G1202R mutant of the ALK kinase domain accounts for approximately 75% of identifiable ceritinib and alectinib secondary mutations in the ALK domain that confer ALK-inhibitor resistance (12). One preclinical study demonstrated brigatinib’s efficacy in G1202R and L1196M-mutants as well as EGFRTM-mutant ALK-rearranged NSCLC, suggesting broader activity than any currently approved ALK-inhibitor (13). In fact, brigatinib maintained activity against all 17 secondary ALK-mutants analyzed with a superior activity profile to crizotinib, ceritinib, and alectinib. Thus, the 14.5 months PFS reported by Gettinger et al., the longest PFS observed with any ALK-inhibitor in CR-patients, may soon be a reality.
Toxicity will be another determining factor for potential role of brigatinib in ALK-rearranged NSCLC. Serious adverse events have been reported with other ALK-inhibitors, paradoxical for a targeted therapy. PROFILE 1,014 related significantly more diarrhea (61% vs. 13%), edema (49% vs. 12%), vomiting (46% vs. 36%), and constipation (43% vs. 30%) with crizotinib compared to chemotherapy (1). Rates of crizotinib discontinuation secondary to its adverse events have been as high as 20.2% and as many as 74% experience dose interruptions (9). Likewise, ASCEND-5 reported significant grade 3 or 4 nausea and vomiting associated with ceritinib compared to chemotherapy (7.8% vs. 1.8%) (6). Moreover, nearly 50% of patients treated with ceritinib experience a grade 3 or 4 adverse event. Alectinib, conversely, has proven more tolerable with only 29% experiencing dose interruptions and 8.7% completely discontinuing therapy (9).
Serious adverse events reported by the Phase I/II study of brigatinib were dyspnea (7%), pneumonia (7%), and hypoxia (5%) (2). The most common toxicity was nausea (53%), primarily Grade 1 or 2. Doses had to be reduced in 16% of the patients in the Phase II dose expansion phase. Overall, the daily 90 mg dose appeared to improve tolerability without sacrifice of efficacy, and the 180 mg dosing, following 90 mg 7-day lead in, appeared to minimize the aforementioned pulmonary events. Four patients (22%) who received the 90 mg daily dose and nine patients (28%) experienced dose interruptions lasting more than two days. Only thirteen (9%) of patients had discontinued brigatinib due to adverse events. Given this, brigatinib may have tolerability more similar to alectinib than crizotinib and ceritinib. Albeit promising, adequately powered trials with these two regimens demonstrating the toxicity profile and Phase III trials comparing brigatinib to crizotinib in ALK-inhibitor-naïve patients with advanced ALK-rearranged NSCLC are still in progress (ALK in Lung Cancer Trial of AP26113; NCT02094573).
The future of ALK-inhibiting therapy in NSCLC
Despite recent proliferations of ALK-inhibitor drugs, each drug’s role and, in particular, the sequence in which they are administered to prolong life, remains uncertain. ASCEND-4 reported improved survival with first-line ceritinib compared to crizotinib, but the sequential prescription of a second generation ALK-inhibitor at the onset of progression with crizotinib may be superior (5,14). For example, PFS on crizotinib is 10.9 months in patients who have not been treated with chemotherapy, and, if these Gettinger et al. data are validated in larger trials, the addition of brigatinib after onset of crizotinib resistance has potential to extend PFS to over 2 years after initiation of ALK-inhibitor therapy. The sheer morbidity of CNS progression, however, may eventually give pause to crizotinib’s first-line use. Conversely, perhaps the increasingly rapid generation of resistance to second-generation inhibitors in CR patients justifies further investigation of first-line use of more broadly-acting ALK-inhibitors.
While these data presented by Gettinger et al. are impressive, brigatinib does not end the pressing need for innovative treatment of ALK-rearranged NSCLC. ALK-inhibition therapy, as transiently effective as it may be inevitably culminates in resistance. Of the 137 patients in all cohorts, 67 discontinued brigatinib due to disease progression. The heterogeneity with which ALK-rearranged NSCLC generates mutant genotypes resistance to these drugs accounts for this (14). To date, therapeutic research in ALK-rearranged NSCLC has focused on developing ALK-inhibiting agents with broader range of activity. A potentially more advantageous approach may be to evaluate ALK-inhibitors alongside other targeted therapies.
For example, Mammalian Target of Rapamycin (mTOR) inhibition represents a potential synergistic target alongside EML4-ALK. Studies have demonstrated downstream signaling effects from the EML4-ALK fusion protein that increase mTOR expression (15). This, in turn, contributes to the cancer stem cell phenotype that perpetuates the inevitability of tumor resistance to ALK-inhibition. Therefore, simultaneous ALK and mTOR inhibition may synergistically diminish the cancer stem cell phenotype. Not only does mTOR represent a synergistic target with ALK-inhibition, but these same studies demonstrated potential reversal of CR in cell lines treated with mTOR inhibition (16).
EML-ALK driver mutations also appear to favor expression of programmed cell death ligand-1 (PD-L1), generating the evasion of immune surveillance. In one translational study of 532 resected pulmonary adenocarcinomas, higher levels of PD-L1 expression were associated with both shorter PFS with crizotinib (P=0.001) and OS after treatment of crizotinib (P=0.002) (16). Pembrolizumab, an anti-PD-1 therapy already approved by the FDA in NSCLC expressing over 50% PD-L1, may offer synergistic benefit alongside ALK-inhibition (17). Furthermore, the same study suggests that both upregulation in signal transducer and activator of transcription 3 (STAT3) and hypoxia inducible factor (HIF)-1α increase PD-L1 expression in ALK-rearranged NSCLC, identifying two more potentially synergistic targets with ALK-inhibition (16). One Phase I study (NCT02511184) is underway to evaluate crizotinib plus pembrolizumab in the treatment of ALK-positive NSCLC.
Conclusions
In summary, early clinical data reported from Gettinger et al. truly appear promising; brigatinib has proven both tolerable and potentially efficacious. However, resistance and progression will likely remain a challenge with brigatinib, despite its superior preclinical potency and broader range of activity. Thus, the future role of ALK-rearranged NSCLC may theoretically rely on combination, targeted therapy. Investigating these strategies, rather than marginally more effective designer ALK-inhibitors, may prove more beneficial in the treatment of NSCLC.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Wei Xu (Division of Respiratory Disease, Department of Geriatrics, the First Affiliated Hospital of Nanjing Medical University, Nanjing, China).
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.03.20). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 2014;371:2167-77. [Crossref] [PubMed]
- Gettinger SN, Bazhenova LA, Langer CJ, et al. Activity and safety of brigatinib in ALK-rearranged non-small-cell lung cancer and other malignancies: a single-arm, open-label, phase 1/2 trial. Lancet Oncol 2016;17:1683-96. [Crossref] [PubMed]
- Crinò L, Ahn MJ, De Marinis F, et al. Multicenter Phase II Study of Whole-Body and Intracranial Activity With Ceritinib in Patients With ALK-Rearranged Non-Small-Cell Lung Cancer Previously Treated With Chemotherapy and Crizotinib: Results From ASCEND-2. J Clin Oncol 2016;34:2866-73. [Crossref] [PubMed]
- Felip E, Orlov S, Park K, et al. ASCEND-3: A single-arm, open-label, multicenter phase II study of ceritinib in ALKi-naïve adult patients (pts) with ALK-rearranged (ALK+) non-small cell lung cancer (NSCLC). J Clin Oncol 2015;33:abstr 8060.
- De Castro G, Tan DS, Crinò L, et al. PL03.07: First-line Ceritinib Versus Chemotherapy in Patients with ALK-rearranged (ALK+) NSCLC: A Randomized, Phase 3 Study (ASCEND-4). J Thorac Oncol 2017;12:S7. [Crossref]
- Scagliotti G, Kim TM, Crinò L, et al. Ceritinib vs chemotherapy (CT) in patients (pts) with advanced anaplastic lymphoma kinase (ALK)-rearranged (ALK+) non-small cell lung cancer (NSCLC) previously treated with CT and crizotinib (CRZ): results from the confirmatory phase 3 ASCEND-5 study. Ann Oncol 2016;27:LBA42. _PR. [Crossref]
- Shaw AT, Gandhi L, Gadgeel S, et al. Alectinib in ALK-positive, crizotinib-resistant, non-small-cell lung cancer: a single-group, multicentre, phase 2 trial. Lancet Oncol 2016;17:234-42. [Crossref] [PubMed]
- Ou SH, Ahn JS, De Petris L, et al. Alectinib in Crizotinib-Refractory ALK-Rearranged Non-Small-Cell Lung Cancer: A Phase II Global Study. J Clin Oncol 2016;34:661-8. [Crossref] [PubMed]
- Nokihara H, Hida T, Kondo M, et al. Alectinib (ALC) versus crizotinib (CRZ) in ALK-inhibitor naive ALK-positive non-small cell lung cancer (ALK+ NSCLC): Primary results from the J-ALEX study. J Clin Oncol 2016;34:abstr 9008.
- Wardak Z, Choy H. Improving Treatment Options for Brain Metastases From ALK-Positive Non–Small-Cell Lung Cancer. J Clin Oncol 2016;34:4064-5. [Crossref] [PubMed]
- Ou SH, Jänne PA, Bartlett CH, et al. Clinical benefit of continuing ALK inhibition with crizotinib beyond initial disease progression in patients with advanced ALK-positive NSCLC. Ann Oncol 2014;25:415-22. [Crossref] [PubMed]
- Hatcher JM, Bahcall M, Choi HG, et al. Discovery of inhibitors that overcome the G1202R ALK Resistance Mutation. J Med Chem 2015;58:9296-308. [Crossref] [PubMed]
- Zhang S, Anjum R, Squillace R, et al. The Potent ALK Inhibitor Brigatinib (AP26113) Overcomes Mechanisms of Resistance to First- and Second-Generation ALK Inhibitors in Preclinical Models. Clin Cancer Res 2016;22:5527-38. [Crossref] [PubMed]
- Tan DS, Araújo A, Zhang J, et al. Comparative Efficacy of Ceritinib and Crizotinib as Initial ALK-Targeted Therapies in Previously Treated Advanced NSCLC: An Adjusted Comparison with External Controls. J Thorac Oncol 2016;11:1550-7. [Crossref] [PubMed]
- Passaro A, Lazzari C, Karachaliou N, et al. Personalized treatment in advanced ALK-positive non-small cell lung cancer: from bench to clinical practice. Onco Targets Ther 2016;9:6361-76. [Crossref] [PubMed]
- Koh J, Jang JY, Keam B, et al. EML4-ALK enhances programmed cell death-ligand 1 expression in pulmonary adenocarcinoma via hypoxia-inducible factor (HIF)-1α and STAT3. Oncoimmunology 2015;5:e1108514 [Crossref] [PubMed]
- Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]


