
A review of pituitary abscess: our experience with surgical resection and nursing care
Introduction
Pituitary abscess (PA) is a rare disease in the saddle area and accounts for approximately 0.24% to 0.6% of all pituitary lesions (1). Since the first case of PA was reported by Simomonds in 1941, PA has received increasing attention from neurosurgeons. Because of its difficult prognosis, PA is potentially life-threatening if not appropriately diagnosed and treated. Although the visual access of computerized tomography (CT) and magnetic resonance imaging (MRI) is more universal, PA is still easily confused with other saddle lesions, including cystic pituitary adenoma, craniopharyngioma, and Rathke’s cyst (1). Compared with radiology and symptomatology, pathology is a more direct and accurate approach for diagnosing PA. Neurosurgical intervention provides an effective way for specimen collection and lesion clearance. Between January 2005 and March 2016, we diagnosed and operated more than 1,100 patients with saddle lesions. However, there were only 4 cases pathologically diagnosed as PA at our centre. There is still some controversy regarding the pathogenesis and treatment of PA, such as infection sources, imaging features, and mode of neurosurgical interventions. To further understand and provide a reference basis for these issues, more data are needed. Here, we present these four cases of PA that were evaluated and treated at our institution.
We reviewed the clinical manifestations, images, hormonal levels, therapeutic plans and postoperative pathologies. Four patients with PA were sieved out of 1,156 cases of pituitary adenomas and other sellar lesions at our centre. Three female patients and one male patient consisted of this report, whose average age was 39.5 years. All patients were finally diagnosed as PA, based on histopathological examinations. Each patient got assessments of hormone and haemogram. One required right transfrontal approach, and another three patients underwent transsphenoidal surgery. However, 2 of these patients suffered from recurrence of PA 2 months after operation, and the second operation was conducted on the primary surgical approach. Everyone recovered well at their respective follow-up (Table 1).
Full table
Case presentation
Case 1
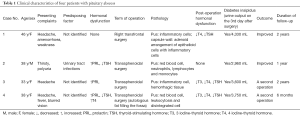
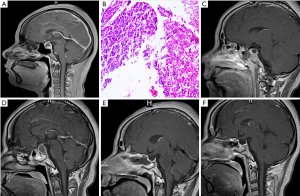
A 46-year-old female patient complained for headache with fullness in the head, amenorrhoea and weakness for 1 year. She was an immunocompetent woman without hypertension, diabetes mellitus, trauma or history of infection, and no medical history was taken. The body temperature was stable in the normal range (36.5–37.3 °C), and other vital signs were normal. Visual acuity was separately 1.0 in both the right and left eyes. Common vision of both eyes was confirmed by computerized perimetry. Her urinalysis showed that the white blood cell count in the urine was 370.2/HPF, and the red blood cell count was 6/HPF. Levofloxacin was administered for urinary tract infection. The complete blood count, biochemical tests, and markers for viral hepatitis and HIV were all normal. The hormonal levels were as follows: PRL, 25.55 ng/mL; and TSH, 0.44 mIU/mL; all other related hormones were within normal ranges. A 1 cm × 1 cm × 1 cm sellar mass elevating the optic tract was found on MRI scanning. T2-weighted sagittal section showed the lesion was a hyperintense area and contrast MRI showed a central hypointense area with peripheral rim enhancement (Figure 1A,B). The initial diagnosis was considered as either pituitary tumour or apoplexy. We opted to perform right transfrontal surgery considering the elevated optic nerve and the potential of severing the optic nerve. A yellow cystic lesion with a solid capsule wall was seen via microscope (Figure 1C), which undoubtedly adhered to the optic chiasma and bulged backward. A fine needle was used for paracentesis, however it failed after several attempts. A small cut on the wall was made by using microscissors while the fine needle extracted 1 ml of pus. We completed a subtotal resection, and the remainder of the lesion adhered to the optic chiasma. The adherent part of capsule wall was carefully fulgerized by bipolar coagulation. The operative area underwent repeated washes with physiological saline containing antibiotics. The histopathology demonstrated that most of the cells in the liquid were disintegrated with a few inflammatory cells and red blood cells (Figure 1D,E). The capsule walls were described as an adenoid arrangement of epithelioid cells mixed with inflammatory cells. The patient was administered ceftriaxone sodium for 4 weeks to prevent infection, desmopressin to reduce the polyuria symptoms, and thyroid hormone tablets to prevent hormone reduction. Postoperative MRI showed that the cystic mass was completely removed (Figure 1F). She did not feel any discomfort and was discharged on postoperative day 10.
Case 2
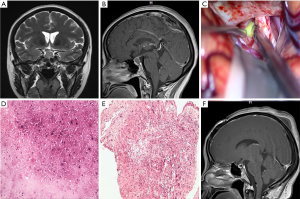
A 38-year-old male patient suffering from thirst and polyuria for more than 4 months was seen at our clinic. Headache, blurred vision and sexual dysfunction were not mentioned, and his physical examination and laboratory finding were normal. An automated test of visual acuity and vision was also normal. The brain CT scan showed a slightly hyperdense area in the saddle area (Figure 2A). Bone around the saddle area was not invaded (Figure 2B). Contrast T1-weighted MRI revealed a mass with symmetric rim enhancement (Figure 2C,D), which was diagnosed as a pituitary adenoma (pre-operation diagnosis). The patient was administered desmopressin to control the increased urine volume (4 L/day). Although the urine volume was regulated, his thirst symptoms did not subside. He underwent a transsphenoidal surgery, where a small amount of dark yellow and red liquid exuded from the pituitary. An analysis of the pus revealed a mass of red blood cells as well as neutrophils, lymphocytes and monocytes. The histopathological diagnosis was PA (Figure 2E). He experienced four weeks treatment of ceftriaxone, and stopped the desmopressin until the urine volume was normal. Postoperative hormone levels did not show any abnormality. At postoperative day 9, He recovered well and left hospital. MRI was nearly normal on the 20th day (Figure 2F). At his 1-year follow-up, the thirst and polyuria symptoms were completely abated.
Case 3
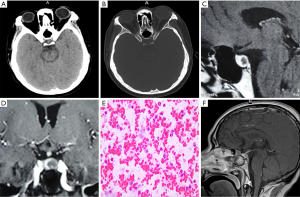
A 38-year-old woman with headache, fever and blurred vision for 18 days was referred to our centre. Her visual acuity was normal, but a defect of the inferior temporal quadrant vision of both eyes was found. The PRL levels were 2,108 ng/mL (normal range, 5–25 ng/mL), whereas the other hormone levels were within their respective normal ranges. An MRI of the saddle area showed a cystic lesion with an uneven signal centre. Based on the radiology and symptoms, the preoperative diagnosis was a prolactin-secreting pituitary adenoma with haemorrhage. She underwent the transsphenoidal surgery, and yellow pus flowed out (Figure 3A-C). The patient was administered vancomycin and ceftriaxone to treat the Gram-positive bacteria. The hypothyroidism and polyuria manifested as insomnia, thirsty and weakness, which were treated with zolpidem tartrate, desmopressin and thyroid hormone tablets, respectively. At 2 months after surgery, she complained of headache and fever. MRI showed a mixed abnormal mass in the saddle area uplifted in the optic chiasma (Figure 3D-F). The patient underwent the same procedure, and the graft was completely removed. Vancomycin and ceftriaxone continued to be used for 6 weeks after surgery. At her 1-year follow-up, the patient did not suffer from any symptoms, and her hormone levels were normal.
Case 4
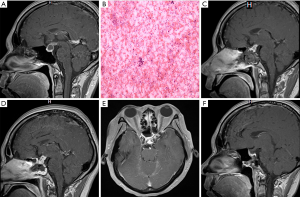
A 33-year-old woman was admitted to our hospital complaining of cyclical headaches for 2 months, which were bifrontal in location. She underwent two lumbar punctures before she was admitted to our centre, the results of which were normal with normal nerve functions. Her hormone levels were as follows: PRL, 50.58 ng/mL; T3, 1.17 nmol/L; TSH, 1.54 mIU/L; FSH, 6.13 IU/L; T4, 73.1 nmol/L; and FT4, 12.5 pmol/L. T1-weighted MRI with contrast enhancement of the saddle area revealed a cystic mass with an elevated saddle diaphragm, and there was a hyperintense signal at the bottom of the cyst (Figure 4A-C). Based on the MRI, we initially diagnosed the lesion as pituitary adenoma apoplexy. Transsphenoidal surgery was performed for her progressive headache. When the dura mater was cut, a white viscous liquid flowed out. The entire mass was cleared, and a slight cerebrospinal leak was discovered upon further examination under the microscope. The autologous fat was plugged in the fossa. There was no bacterial growth after liquid culture; thus, either PA or pituitary apoplexy was considered by histopathology. Anti-infection and antidiuresis medications were administered as an empirical treatment. None of abnormalities afflicted her, and she discharged 2 weeks after operation. However, she experienced an acute severe headache 2 months after PA surgery. As the MRI showed a larger cystic mass in the saddle area (Figure 4D-F), the recurrence of PA was first considered. Ceftazidime was used to control infection. After the preparations were completed, she underwent a second operation using the same approach as before. After the yellow and white pus were aspirated, the graft was removed, and antibiotic water was repeatedly washed in the fossa. The patient was administered linezolid for 6 weeks because of the identification of Gram-positive bacteria and her allergy to vancomycin. On the 14th day after the operation, her haemogram (white blood cell count, 6.63×109/L) and C reactive protein levels (<5.0 mg/L) were normal. She recovered well and was finally discharged from the hospital.
Post-operation therapy and nursing care
Post-operation therapy and nursing care are very important for patients with PA. After operation, the patient was suggested lay down in the first 3 days, and daily input and output fluid volumes were recorded by nurses and kept steady, especially 24 h urine volume and every hour urine volume. Antibiotics were used for routine therapy after surgery, and could be chosen according to the results of microbiological detection for abscess. Diabetes insipidus is one of the most common complications after PA surgery. Thus, we should pay much more attention to daily urine volume. Sometimes medications of minirin are needed to control diabetes insipidus. Hypothalamic response is one of the complications as well, but more serious. In such situation, fever and diabetes insipidus may occur, and electrolytes are in disorder, thus, measures should be taken to observe the patient by nurses and keep the internal environment in balance. Hypopituitarism is also observed in patients after PA operation, and prednisone tablets were prescribed daily, and the dose of prednisone was slowly decreased after patient discharge.
Discussion
PA is a rare infectious disease in the saddle area, and its diagnosis is challenging for clinicians (1,2). With the development of technology, blood counts, hormone levels and imaging have become the standards for diagnosis. Classical signs of infection such as fever or laboratory markers of inflammation are easier to be identified, but they still lack sensitivity and specificity (3). Changes in the hormonal levels and imaging provide evidence regarding the position and size of the lesion, but these diagnostic measures do not offer conclusive evidence (4). In addition, the low incidence rate, self-limitations and asymptomatic regional infection contributing to PA cannot be completely excluded (5). According to this evidence, surgical intervention and pathological examination are the most useful methods for diagnosis and treatment.
PA has complex pathogenesis and can be subdivided into two categories (6-9). The first type is primary PA, which manifests via haematogenous metastasis and direct spreading (4). The other consists of the propagation of a regional infection, including sphenoid sinusitis, cavernous sinus thrombophlebitis, meningitis, and infection following tooth extraction, to the pituitary gland to result in secondary PA (6). A transsphenoidal or transcranial approach to the pituitary gland is also a potential source of secondary PA (8,10). After an operation to remove an intrasellar tumour, complications such as blood supply disorders and hypoimmunity may increase the risk of infection (10). Cases 3 and 4 might have acquired their infections from the graft during the earlier surgery.
The pathogenic microorganisms in abscesses are widespread and include Gram-positive bacteria, Gram-negative bacteria, anaerobes and fungi (8,11). Streptococcus and Staphylococcus are the most predominant Gram-positive bacteria, whereas Escherichia coli, Mycobacterium and Neisseria have also been reported (3,10,11). Because only 50% of cases can culture the pathogens (12), broad-spectrum antibiotics are used as an empirical therapy. Identifying the pathogen is necessary for therapeutic management. In 2 of our cases, the insufficient volume of pus prevented culturing of the bacteria, but the other 2 patients were diagnosed with a Gram-positive bacterial infection, which influenced the selection of antibiotics.
MRI with multiparameter characteristics and a multiaxial plane provides important evidence to confirm the position of the lesions (13). Based on the MRI results, a cystic mass with a peripheral rim enhancement with contrast, occasionally associated with hormonal disturbance and symptoms of infection, may correlate with this diagnosis.
Because of the varied compositions of pus, the radiological features of PA cannot be distinguished from other pituitary lesions. Pituitary adenoma with haemorrhage and necrosis, which can fluctuate in the presence of an MRI signal, is often confused with PA. Upon enhancement, PA has a uniform rim thickness and a thickened pituitary stalk, whereas pituitary adenoma with a cyst just shows a slightly curved capsule wall as usual (14). Although MRI with gadolinium enhancement may help to identify PA, there are still some diseases that are difficult to distinguish, such as craniopharyngioma, Rathke’s cyst, hypophysis, and benign hyperplasia of the pituitary (15-17).
Neurosurgical intervention is a direct and effective method. Compared with the transfrontal approach, the transsphenoidal approach has the advantage of reduced trauma and a fast recovery (18). Three of our patients underwent the transsphenoidal approach, but 2 of them required a second operation, and the potential infection risk of each approach should be considered. The graft and antibiotic resistance might have contributed to the recurrence. The transfrontal approach causes a larger wound and increased risk of damage to nerve function. We chose this approach for one case because we theorized that the mass had a high probability of adhering to the optic nerve. In using the transfrontal approach, a larger operative field can be provided to ensure that as much of the mass is removed as possible. If the abscess recurs, reintervention is still the first choice (19). Additionally, antibiotic therapy to heal a high index of suspicion for PA has been reported. A 74-year-old woman with recurring PA was administered an antibiotic regimen comprising panipenem/betamipron, clindamycin and chloramphenicol). Although the size temporarily increased, she eventually recovered well without requiring an operation (20).
In conclusion, PA is rare disease that lack unique imaging features or specific symptoms. There are several instances in which PA should be considered in the differential diagnosis. In MRI showing a peripheral rim enhancement and a thickened pituitary stalk, PA should be highly suspected. Although very rare, neurosurgical intervention should be considered with other factors. The keys for successfully treating PA include an early diagnosis, early operation, symptomatic treatment and the standardized use of spectrum-specific antibiotics.
Acknowledgments
Funding: This study was supported by the Nanjing Science and Technique Development Foundation (No. 201605077), and the National Natural Science Foundation of China (No. 81601069).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.06.36). The authors have no conflicts of interest to declare.
Ethical statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Simmonds M. Zur pathologic der hypophysis. Verh Disch Pathol 1914;17:208-12.
- Zhang X, Sun J, Shen M, et al. Diagnosis and minimally invasive surgery for the pituitary abscess: a review of twenty nine cases. Clinical Neurology and Neurosurgery 2012;114:957-61. [Crossref] [PubMed]
- Hazra S, Acharyya S, Acharyya K. Primary pituitary abscess in an adolescent boy: a rare occurrence. BMJ Case Rep 2012;2012. [PubMed]
- Meftah A, Moumen A, Eljadi H, et al. Pituitary abscess simulating a pituitary adenoma. Presse Med 2016;45:602-4. [Crossref] [PubMed]
- Gonzales M, Marik PE, Khardori RK, et al. A pituitary abscess masquerading as recurrent hypernatremia and aseptic meningitis. BMJ Case Rep 2012;2012. [PubMed]
- Soga Y, Oka K, Sato M, et al. Cavernous sinus thrombophlebitis caused by sphenoid sinusitis--report of autopsy case. Clin Neuropathol 2001;20:101-5. [PubMed]
- Naama O, Gazzaz M, Boulahroud O, et al. Infection of a Rathke cleft cyst: a rare cause of pituitary abscess. Surg Infect (Larchmt) 2014;15:358-60. [Crossref] [PubMed]
- Hong W, Liu Y, Chen M, et al. Secondary headache due to aspergillus sellar abscess simulating a pituitary neoplasm: case report and review of literature. Springerplus 2015;4:550. [Crossref] [PubMed]
- Pepene CE, Ilie I, Mihu D, et al. Primary pituitary abscess followed by empty sella syndrome in an adolescent girl. Pituitary 2010;13:385-9. [Crossref] [PubMed]
- Beatty N, Medina-Garcia L, Al Mohajer M, et al. Polymicrobial Pituitary Abscess Predominately Involving Escherichia coli in the Setting of an Apoplectic Pituitary Prolactinoma. Case Rep Infect Dis 2016;2016:4743212 [Crossref] [PubMed]
- Hao L, Jing C, Bowen C, et al. Aspergillus sellar abscess: case report and review of the literature. Neurol India 2008;56:186-8. [Crossref] [PubMed]
- Dutta P, Bhansali A, Singh P, et al. Pituitary abscess: report of four cases and review of literature. Pituitary 2006;9:267-73. [Crossref] [PubMed]
- Erdogan G, Deda H, Tonyukuk V. Magnetic resonance imaging and computerized tomography images in a case of pituitary abscess. J Endocrinol Invest 2001;24:887-91. [Crossref] [PubMed]
- Chen CC, Carter BS, Wang R, et al. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guideline on Preoperative Imaging Assessment of Patients With Suspected Nonfunctioning Pituitary Adenomas. Neurosurgery 2016;79:E524-6. [Crossref] [PubMed]
- Coulter IC, Mahmood S, Scoones D, et al. Abscess formation within a Rathke's cleft cyst. J Surg Case Rep 2014;2014: [Crossref] [PubMed]
- Lee IH, Zan E, Bell WR, et al. Craniopharyngiomas: Radiological Differentiation of Two Types. J Korean Neurosurg Soc 2016;59:466-70. [Crossref] [PubMed]
- Colli ML, Migowski W Jr, Czepielewski MA, et al. Pituitary abscess simulating apoplexy. Arq Bras Endocrinol Metabol 2006;50:1122-6. [Crossref] [PubMed]
- Hanba C, Svider PF, Shkoukani MA, et al. Pediatric pituitary resection: characterizing surgical approaches and complications. Int Forum Allergy Rhinol 2017;7:72-9. [Crossref] [PubMed]
- Nishimura K, Takao T, Mimoto T, et al. A case of anterior hypopituitarism showing recurrent pituitary mass associated with central diabetes insipidus. Endocr J 2003;50:825-9. [Crossref] [PubMed]
- Uchida Y, Tsuchimochi N, Oku M, et al. Successful treatment of pituitary abscess with oral administration of sparfloxacin. Intern Med 2008;47:1147-51. [Crossref] [PubMed]


