
Effective combinatorial immunotherapy for castration-resistant prostate cancer: new future chance?
Prostate cancer (pCa) is the second most common non-cutaneous malignant neoplasm in men worldwide, with an estimated incidence of 1.1 million new cases per year. Furthermore, it is the fifth leading cause of cancer-related death, representing 6.6% of total male mortality (1).
New cases of pCa mostly show a localized disease at first presentation diagnosis and they are potentially curable, unfortunately relapses occur in 20% to 30% of these patients despite a curative intent therapy. Moreover, the current incidence of lethal pCa metastatic evidence at the time of diagnosis has declined to 5% approximately (2,3).
Androgenic deprivation therapy (ADT) is a standard of care against pCa. This therapy reduces at first the tumor burden and/or circulating PSA to low or undetectable levels (4). However, the response duration should be variable from months to years with unavoidable disease progression in patients with metastatic disease (5). The pCa growing despite adequate ADT is defined as castration-resistant prostate cancer (CRPC) (5).
Several new agents have been developed in metastatic CRPC (mCRPC) treatment, leading to the ability of androgen receptor (AR) signaling inhibition. These strategies include those drugs interfering with androgenic stimulation as abiraterone and enzalutamide, already approved in mCRPC disease over the last decade (6-9).
Despite a survival related improvement due these second-generation AR targeted therapies, acquired or inherent resistance may occur in all patients so that metastatic pCa currently remains incurable. Failure of ADT and chemotherapies (docetaxel and cabazitaxel) is the major cause of death in patients with CRPC (10,11).
New strategies will be necessary to improve cancer management. In order to assess an adequate process of anticancer therapy, targeting immune system represent a promising option. Checkpoint blockade immunotherapies have shown exciting results in several tumor types as NSCLC, melanoma and renal-cell cancer (12).
The presence of inflammatory cells and T-cell infiltrates in pCa tissues provides the activity of a host immune-response towards this neoplasm (13,14). Potential benefit from immunotherapeutic strategies in patients with CRPC is further suggested by preclinical studies achievements in experimental pCa models and the clinical activity results of sipuleucel-T (15-17).
Despite that premises, current data demonstrates failures of various immune system targeting agents in mCRCP. Two phase III clinical trials assessing ipilimumab versus placebo after progression to docetaxel-chemotherapy and ipilimumab versus placebo in chemotherapy-naïve mCRPC setting showed no significant difference between the ipilimumab group and the placebo group in terms of overall survival (18,19).
Resistance towards immune checkpoint blockade (ICB) in pCa has to be still identified.
Myeloid-derived suppressor cells (MDSCs) play an important role in immunotherapy failure as well as pCa promotion and progression. In healthy subjects, immature myeloid cells (IMCs) generated in bone marrow differentiate into mature macrophages, granulocytes or dendritic cells. In cancer patients appears a partial blockade in IMCs differentiation, which produce an expansion of this population. Moreover, among this pathological context there are evidences of upregulated expression of immune suppressive factors (ARG1, NOS2, NO, ROS) resulting in IMC population spreading with immune suppressive activity; these cells are known as MDSCs (20,21). A high amount of circulating MDSCs are associated with prostate-specific antigen levels and higher risk of metastasis in pCa (21). Furthermore, a better knowledge of the immune infiltrate composition and interactions between cancer and immune system would help to identify proper candidates for immunotherapy (22).
In this clinical scenario Lu and co-workers hypothesized that the combination of target therapy against mCRPC-infiltrating MDSCs with ICB agents may improve the response to immunotherapy (23).
They conducted a preclinical trial using a novel chimeric mouse model of mCRPC, engineered with signature genes mutations implicated in the genesis of human pCa. The genetically engineered mice exhibited autochthonous tumor evolution among an intact immune system (23).
Traditionally, preclinical studies have largely used xenograft models of human pCa, using cell lines of prostate tumor implanted into immune-deficient mice. However, xenograft models have several important limitations due to heterologous microenvironment and absence of endogenous immune response. Thus, the study of combination therapy using xenograft models appears to be inappropriate (24).
Lu and his colleagues employed novel non-germline mCRPC model availing mouse embryonic stem cell clones (JH61 and JH58) derived from PB-Cre+ PtenL/L p53L/L Smad4L/L mTmGL/+ LSL-LUCL/+ (CPPSML) genotypes which exhibited age-dependent green fluorescent protein (GFP+) LUC+ pCa growth (23).
Mice that developed GFP+ cancer cells at 3 months, with a dissemination of cancer cells also to lung and lymph nodes, underwent to androgen deprivation therapy protocol (castration followed by enzalutamide-admixed diet) in order to induce CRPC. Then, CPPSML chimaeras with MRI documented mCRCP were assigned to therapeutic trials (23).
The selected target agents were the tyrosine kinase inhibitors dasatinib (Dasa) and cabozantinib (Cabo), and the phosphoinositide 3-kinase PI3K/mTOR dual inhibitor BEX235 (BEZ). Moreover, a combination of anti-CTLA-4 and anti-PD1 was used for ICB.
CPPSML chimaeras were randomized to receive single agent or combination treatment for 4 weeks. The combination CABO + ICB and BEZ + ICB showed a synergic efficacy to bring a significant burden disease reduction. On the contrary, administration of target single agents, dual ICB cocktail or DASA + ICB had minimal impact on prostate tumor mass and metastasis reduction (23).
Furthermore, authors explored tumor micro-environment modifications using CyTOF analysis of mouse prostate tumors (23).
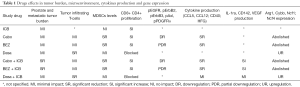
They demonstrated that Cabo + ICB and BEZ + ICB treatment was not associated with significant reduction of tumor-infiltrating T cells, but showed a reduction of Gr-MDSCs and an increase of CD8+/Treg ratio. Cabo or BEZ in combination with ICB mitigated the suppressive activity of intratumoral MDSCs on CD4+ and CD8+ T-cell proliferation (Table 1) (23).
Full table
Moreover, as parallel evidence, CD4+ and CD8+ T-cell proliferation was entirely blocked by Dasa. A significant reduction of tumour-infiltrating T cells was associated with Dasa treatment, related to T cell depletion into tumor microenvironment, probably due to the small impact of Dasa + ICB.
Cabo and BEZ combination treatment with ICB induced downregulation of pEGFR, pErbB2, pErbB3, pAxl and pPDGFRα, and reduced phosphorylated MET and VEGFR2. Finally, these combinations affected cytokine production in primary CRPC, with CCL5, CCL12, CD40, HGF reduction and IL-1ra, CD142 and VEGF increase. These cytokines modifications, less pronounced in Dasa + ICB treatment, may influence the activity of myeloid cells and upregulate the gene expression responsible of MDSC-induced immune suppression (Arg1, Cybb, Ncf1, Ncf4) (Table 1) (23).
In conclusion, it appears reasonable believing that synergic effects of ICB and target therapies against mCRCP-infiltrating MDSCs, might be related to the selective MDSCs depletion and tumor microenvironment changes.
Lu and colleagues confirmed the immunosuppressive T cells activity caused by MDSCs into tumor microenvironment, generating resistance to ICB. Whereas treatment with targeted agents against MDSCs enforced T cells, enhancing ICB.
On top of that, this paper highlights the importance of longitudinal immune-response study approach. In fact, the dynamicity of the immune system prevents conduction of data analysis extrapolated from a specific time point. Thus, exploring the microenvironment tumor changes and MDSCs levels appear incredible interesting.
Genetically optimization of an engineered mouse model of pCa leaded to significant advances to understand cellular pathways from cancer initiation to castration resistance, through observation of disease progression.
The development of a CPPSML chimeric mCRPC model in mice, looking for an efficient combinatorial immunotherapy, plays a promising approach in order to understand the relationship between novel therapies and microenvironment modifications. Probably, this model will provide important insights into pCa mechanisms.
Based on these preclinical trials results, future clinical studies in human mCRCP patients should explore molecular mechanisms causing immunotherapy de novo resistance in pCa, in order to achieve the best combination therapy, identifying the most effective schedule protocols.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Peng Zhang (Department of Urology, Zhongnan Hospital of Wuhan University, Wuhan, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.07.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-86. [Crossref] [PubMed]
- Howlader N, Noone AM, Krapcho M, et al. editors. SEER Cancer Statistics Review, 1975-2013, National Cancer Institute. Bethesda, MD. Available online: https://seer.cancer.gov/csr/1975_2013/, based on November 2015 SEER data submission, posted to the SEER web site, April 2016.
- Abdollah F, Schmitges J, Sun M, et al. Comparison of mortality outcomes after radical prostatectomy versus radiotherapy in patients with localized prostate cancer: a population-based analysis. Int J Urol 2012;19:836-44. [Crossref] [PubMed]
- Hussain M, Tangen CM, Berry DL, et al. Intermittent versus continuous androgen deprivation in prostate cancer. N Engl J Med 2013;368:1314-25. [Crossref] [PubMed]
- Messing EM, Manola J, Sarosdy M, et al. Immediate hormonal therapy compared with observation after radical prostatectomy and pelvic lymphadenectomy in men with node-positive prostate cancer. N Engl J Med 1999;341:1781-8. [Crossref] [PubMed]
- Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med 2012;367:1187-97. [Crossref] [PubMed]
- de Bono JS, Logothetis CJ, Molina A, et al. Abiraterone and Increased Survival in Metastatic Prostate Cancer. N Engl J Med 2011;364:1995-2005. [Crossref] [PubMed]
- Ryan CJ, Smith MR, Fizazi K, et al. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol 2015;16:152-60. [Crossref] [PubMed]
- Beer TM, Armstrong AJ, Rathkopf DE, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med 2014;371:424-33. [Crossref] [PubMed]
- Kalina JL, Neilson DS, Comber AP, et al. Immune Modulation by Androgen Deprivation and Radiation Therapy: Implications for Prostate Cancer Immunotherapy. Cancers (Basel) 2017;9:E13 [Crossref] [PubMed]
- Watson PA, Arora VK, Sawyers CL. Emerging mechanisms of resistance to androgen receptor inhibitors in prostate cancer. Nat Rev Cancer 2015;15:701-11. [Crossref] [PubMed]
- Sharma P, Allison JP. The future of immune checkpoint therapy. Science 2015;348:56-61. [Crossref] [PubMed]
- Mercader M, Bodner BK, Moser MT, et al. T cell infiltration of the prostate induced by androgen withdrawal in patients with prostate cancer. Proc Natl Acad Sci U S A 2001;98:14565-70. [Crossref] [PubMed]
- Bronte V, Kasic T, Gri G, et al. Boosting antitumor responses of T lymphocytes infiltrating human prostate cancers. J Exp Med 2005;201:1257-68. [Crossref] [PubMed]
- Drake CG. Prostate cancer as a model for tumour immunotherapy. Nat Rev Immunol 2010;10:580-93. [Crossref] [PubMed]
- Sobol I, Thompson RH, Dong H, et al. Immunotherapy in prostate cancer. Curr Urol Rep 2015;16:34. [Crossref] [PubMed]
- Kantoff PW, Higano CS, Shore ND, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med 2010;363:411-22. [Crossref] [PubMed]
- Kwon ED, Drake CG, Scher HI, et al. Ipilimumab versus placebo after radiotherapy in patients with metastatic castration-resistant prostate cancer that had progressed after docetaxel chemotherapy (CA184-043): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol 2014;15:700-12. [Crossref] [PubMed]
- Beer TM, Kwon ED, Drake CG, et al. Randomized, Double-Blind, Phase III Trial of Ipilimumab Versus Placebo in Asymptomatic or Minimally Symptomatic Patients With Metastatic Chemotherapy-Naive Castration-Resistant Prostate Cancer. J Clin Oncol 2017;35:40-7. [Crossref] [PubMed]
- Lopez-Bujanda Z, Drake CG. Myeloid-derived cells in prostate cancer progression: phenotype and prospective therapies. J Leukoc Biol 2017;102:393-406. [Crossref] [PubMed]
- Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol 2009;9:162-74. [Crossref] [PubMed]
- Solinas C, Chanzá NM, Awada A, et al. The immune infiltrate in prostate, bladder and testicular tumors: An old friend for new challenges. Cancer Treat Rev 2017;53:138-45. [Crossref] [PubMed]
- Lu X, Horner JW, Paul E, et al. Effective combinatorial immunotherapy for castration-resistant prostate cancer. Nature 2017;543:728-32. [Crossref] [PubMed]
- Shen MM, Abate-Shen C. Molecular genetics of prostate cancer: new prospects for old challenges. Genes Dev 2010;24:1967-2000. [Crossref] [PubMed]


