Adrenal venous sampling as used in a patient with primary pigmented nodular adrenocortical disease
Introduction
Primary pigmented nodular adrenocortical disease (PPNAD) is a rare cause of ACTH independent Cushing syndrome (CS), as the incidence of PPNAD reported accounts for 1% of CS only. However, a number of CS cases resulted from such adrenal conditions as unilateral adrenal adenoma, adrenal carcinoma, or bilateral adrenal hyperplasia which is either pigmented nodular adrenocortical disease known as bilateral micronodular hyperplasia, or bilateral adrenal macronodular hyperplasia. Adrenal venous sampling (AVS) has been used as diagnostic for primary hyperaldosteronism, distinguishing between hyperaldosteronism due to bilateral hyperplasia and unilateral aldosteronoma (1). Selective AVS has always been a gold standard for localization diagnosis of patients with primary hyperaldosteronism (2-4).
Morphological changes in the adrenal glands can lead to very different functional disorders, probably clinically overt or hard to diagnose. On the other hand, adrenal imaging may indicate normal or minor even minimal adrenal nodularity, hardly distinguishable from normal glands. Radiological test found the adrenal glands of normal sizes in half of the cases. The typical radiological appearance characteristics of PPNAD on the CT are described as a “string of beads”, similar to CTH-dependent adrenal adenomatous hyperplasia (5). There can already be functional relevance yet with structural changes too small to be picked up by imaging. AVS serves to determine the source of hormone excess by means of analysis of adrenal blood (2).
Methods
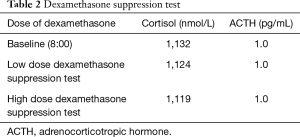
A 21-year-old woman was referred to our hospital with a 2-year history of progressive lumbodynia. She was noted with a moon facies, purple striae on the abdomen, weight gain, a buffalo hump, central obesity, hypertension (BP 190/116 mmHg), and hypokalemia. The woman was 160 cm tall and 65 kg in weight [body mass index (BMI) of 25.4 kg/m2]. Endocrine testing found elevated concentrations of cortisol, with loss of circadian rhythms, and while dramatic drop of ACTH (Table 1).
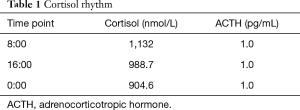
Full table
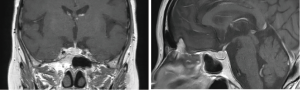
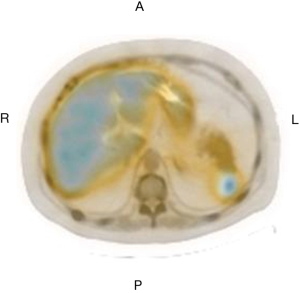
Plasma cortisol concentration cannot be suppressed in dexamethasone suppression test (be it high or low dosage), with significant suppression of ACTH (Table 2). Endocrinological examinations direct to a diagnosis of ACTH-independent Cushing’s syndrome. Chest CT examination suggested multiple old fractures of the ribs on bilateral sides, with multiple compression fractures of the thoracic spine. CT scan revealed moderately full adrenal glands on both kidneys, and suspicious small nodular shadow on the external branch of the left adrenal gland, while enhancement scan found no overt abnormal enhancement (Figure 1) 99mTc-Octreotide somatostatin receptor. SPECT/CT imaging (Figure 2) showed slightly increase of radioactive uptake at the left adrenal; Head MRI showed no delayed enhancement in the saddle region (Figure 3).
Full table
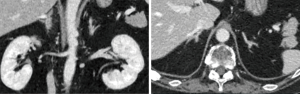
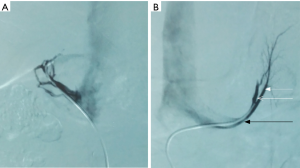
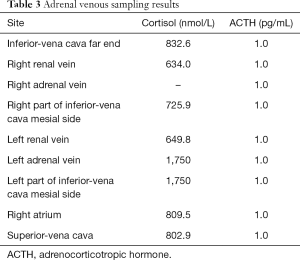
We chose to verify if the catheter tip was properly positioned according to images from the venography, and to correct the dilution difference by measuring cortisol levels (Figure 4). AVS found elevated plasma cortisol concentration of the left adrenal venous and left part of inferior vena cava mesial side, while the plasma cortisol concentration was not detectable in right adrenal vein (Table 3). The results suggest that the patient has an adrenal hyperplasia with cortisol production mostly from the left side.
Full table
Results
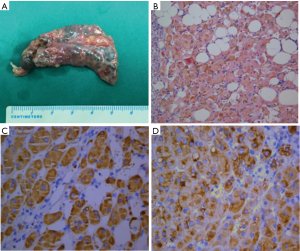
The patient underwent a left adrenalectomy surgery, and the specimen appeared dark brown or dark pigmentation, without capsule. Immunohistochemical staining was positive for α-inhibin+ and Syn+ (Figure 5). The result of the histological study of the glands was consistent with PPNAD. Postoperative endocrinological examination of the patient 3 months later revealed significant decrease of the plasma cortisol concentration, and improvements of symptoms.
Discussion
PPNAD is a rare cause of CS, presenting clinically as part of the Carney’s Complex mostly. Fifty percent of the patients are characteristic of familiar aggregation, featuring autosomal recessive inheritance, with susceptibility gene locus at 2p16 or17q22-24. PPNAD often strikes children and adolescents, yet their clinical manifestation and imaging results tend to be atypical, rarely found with osteoporosis or multiple fractures in their first visit to doctors. When diagnosed as PPNAD, the patients need to be examined in detail as to their family history and physical checkup. They should be appraised for possibility of the Carney’s Complex, and excluded of left atrial myxomas if confirmed of Carney’s Complex which is highly risky of sudden death. Other symptoms also need to be appraised one by one for early treatment. In view of its familiar congregation tendency, family members of the patients also need to take clinical or gene screening in an effort to identify patients of atypical clinical manifestation for early treatment or follow-up visits.
PPNAD is characteristic of persistent automatic hypercortisolism, and its adrenal lesions can hardly be found with B ultrasound; CT scan can hardly detect nonspecific changes, while the adrenal glands are found with irregular augmentation or small nodules, or basically normal to appear hardly distinguishable with normal variants at the adrenal glands (1). Selective adrenal venous sampling (AVS) currently continues to be a gold standard for localization diagnosis in patients with primary hyperaldosteronism (2-4). In addition to cortisol-producing adenoma (CPA), manifestations can also include simultaneously present non-hormonally active tumors, pheochromocytomas or ACTH-independent macronodular adrenal hyperplasia. AVS has also been used to investigate pheochromocytomas (2). Precise preoperative diagnosis, localization diagnosis, and appropriate follow-up treatment of the disease, are dependent upon interdisciplinary cooperation and thorough understanding of PPNAD.
PPNAD, as a cause of ACTH-independent Cushing’s syndrome, may be difficult to diagnose. Firstly, adrenal imaging can be normal or there may only be minor or minimal adrenal nodularity that can hardly be distinguished from normal glands. Secondly, hyperplasia is described histologically not specific and nondescript itself. Lastly, typical adrenal hyperplasia cases do not have cortical cellular pigmentation as seen in this patient’s histology. Hence the histological specimen was reviewed to confirm the findings (5). Whether the adrenal gland should be removed would be a difficult decision. AVS alone cannot confirm the diagnosis of PPNAD, yet it can be used as a surgical indication for adrenal gland resection.
Hypercortisolism manifestations of the patient, namely a moon face, central obesity, purple striae on the abdomen, hypokalemia, hypertension, and osteoporosis suggested Cushing’s syndrome. Laboratory examinations indicate overt cortisol elevation, while plasma cortisol concentration cannot be suppressed in dexamethasone suppression test (be it high or low dosage), confirming the Cushing’s disease. Significant decrease of ACTH suggested ACTH-independent Cushing’s syndrome, but the localization diagnosis remains unclear. AVS by section and cortisol concentration measurement results suggested elevated cortisol concentration at the left adrenal gland and the left inferior vena cava mesial side, instead of any elevation at the right side. This indicated cortisol secretion at the left adrenal gland. Laparoscopic left adrenalectomy was undertaken. Pathological examinations suggested multiple nodular hyperplasia at the left adrenal cortex; the sections grey-yellow or grey-brown, adrenal cortex-zona reticularis thickened, suggesting PPNAD.
PPNAD is a rare cause of Cushing’s syndrome, which is ACTH-independent, involving both adrenal glands. The characteristic pathological features include multiple pigmented cortical nodules and atrophy of the internodular cortex (2). The adrenal size ranges from small to normal or slightly enlarged. These findings can be functionally relevant, yet with structural changes too small to be picked up by imaging. AVS serves to determine the source of hormone excess through the analysis of adrenal blood (6).
Patients in question should be well informed at the onset of the examination, to help them aware of potential dysfunctions and keep confidence in further examinations (2). A full knowledge of the anatomy and variations of the adrenal gland vein, serious preoperative preparation and skilled catheterization manipulation are necessary for obtaining sufficient blood sample and for reducing the occurrence of complications (7). High-quality CT examination is highly conducive to planning AVS. On a modern multisection scanner with reconstruction at 2 or 3 mm, the right adrenal vein can be identified in more than 50% of the patients (8). The use of C-arm CT during the sampling procedure can reduce or even eliminate this failure rate. If AVS is augmented by native C-arm CT to check for the correct catheter position, the technical success rate increases substantially (9).
Conclusions
AVS contributes to the diagnosis of PPNAD and that of Cushing’s syndrome as well. This method however is rarely used for the study of hypercortisolism, probably due to the rarity of cases in which adrenal cortisol secretion and bilateral nodules were present at the same time. Yet it can be a useful test in this group of patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Yì-Xiáng J. Wáng, Yong Wang) for the series “Translational Imaging in Cancer Patient Care” published in Translational Cancer Research. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.12.03). The series “Translational Imaging in Cancer Patient Care” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Our research is a retrospective study, and all analyzes are based on existing materials. The patient was not subjected to any additional examination. The article does not require ethical approval. Informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Doppman JL, Gill JR Jr, Miller DL, et al. Distinction between hyperaldosteronism due to bilateral hyperplasia and unilateral aldosteronoma: reliability of CT. Radiology 1992;184:677-82. [Crossref] [PubMed]
- Blondin D, Quack I, Haase M, et al. Indication and technical aspects of adrenal blood sampling. Rofo 2015;187:19-28. [PubMed]
- Kahn SL, Angle JF. Adrenal vein sampling. Tech Vasc Interv Radiol 2010;13:110-25. [Crossref] [PubMed]
- Magill SB, Raff H, Shaker JL, et al. Comparison of adrenal vein sampling and computed tomography in the differentiation of primary aldosteronism. J Clin Endocrinol Metab 2001;86:1066-71. [PubMed]
- Lim LC, Tan LH, Rajasoorya C. Unravelling the mystery in a case of persistent ACTH-independent Cushing’s syndrome. Ann Acad Med Singapore 2006;35:892-6. [PubMed]
- Travis WD, Tsokos M, Doppman JL, et al. Primary pigmented nodular adrenocortical disease. A light and electron microscopic study of eight cases. Am J Surg Pathol 1989;13:921-30. [Crossref] [PubMed]
- Sun Y, Ni C. Blood sampling from adrenal gland vein. Journal of Interventional Radiology 2009;18:631-5.
- Daunt N. Adrenal vein sampling: how to make it quick, easy, and successful. Radiographics 2005;25:S143-58. [Crossref] [PubMed]
- Georgiades C, Kharlip J, Valdeig S, et al. Use of C-arm CT for improving the hit rate for selective blood sampling from adrenal veins. Radiologe 2009;49:848-51. [Crossref] [PubMed]