
Prevalence, risk factors and prognostic value of anxiety and depression in cervical cancer patients underwent surgery
Introduction
Cancer diagnosis and unfavorable prognosis, which might lead to heavy emotional burden, force cancer survivors to face numbers of challenges during the process of their disease trajectory, including treatments required for curing and controlling cancer progression, fear of health loss and possible death, physical symptoms, limitation of daily lives, and notably, emotional instability (1). In the general cancer population, the prevalence of anxiety and depression ranges from 8–24% with the consideration of cancer type, the treatment duration and the treatment instrument (2,3). Cervical cancer is one frequently diagnosed cancer, and for the cervical cancer survivors, one of the emerging problems is the psychological well-being, such as: postoperative anxiety, depression, reduced self-esteem, etc. (4,5). Anxiety and depression contribute to difficulties in symptom control, poor compliance with treatment, prolonged recovery, which might have negative influence on quality of life and prognosis in cervical cancer patients (4). Therefore, it is essential to explore a deep understanding of the implication of anxiety/depression in cervical cancer.
Accumulating evidence reveals that anxiety and depression are highly prevalent in several cancer patients underwent laparoscopic surgery other than cervical cancer, such as colorectal cancer, bladder cancer and prostate cancer (6-8). Furthermore, the existence of anxiety and depression is indicated to influence the tumor progression as well as the prognosis by affecting patients’ mental state, quality of life and the adherence to the consolidation therapies after surgery (5). For example, one study reveals that anxiety and depression are correlated with poor quality of life, elevated incidence of postoperative morbidity and even the unfavorable long-term prognosis in colorectal cancer patients underwent elective resection (7). However, few related studies have been reported in cervical cancer patients underwent surgery yet. Therefore, this present study was performed to explore the prevalence and risk factors of anxiety and depression, as well as the association of anxiety and depression with survival profiles in cervical cancer patients underwent surgery.
Methods
Subjects
In this prospective cohort study, 158 newly diagnosed cervical cancer patients who underwent surgical resection at our hospital were recruited between January 2011 and December 2013. The inclusion criteria were as follows: (I) diagnosed as primary cervical cancer according to the World Health Organization classification; (II) International Federation of Gynecology and Obstetrics (FIGO) stage I–II, and about to undergo surgical resection; (III) presenting with normal cognitive function, and able to independently fulfill the hospital anxiety and depression scale (HADS). The exclusion criteria were: (I) with an age less than 18 years; (II) antecedent depressive disorders or other mental disorders before cervical cancer diagnosis; (III) unable to be followed up regularly, which was assessed by investigators based on the cervical cancer patients’ overall conditions; (IV) human immunodeficiency virus infection; (V) concomitant with other malignant tumors; (VI) pregnant or lactating women. Besides, a total of 150 age and gender matched healthy subjects were screened as controls to fulfill the HADS assessment when they were undergoing the healthy examination in our hospital during the same period. This study was approved by the Institutional Review Board of our hospital, and all participants provided written informed consents before recruitment. The present study was approved by the Ethics Committee of Harbin Medical University Cancer Hospital with the approval number “KY2010-04”. And the study was conducted in accordance with the provisions of the Declaration of Helsinki.
Baseline data collection
On the recruitment, cervical cancer patients’ baseline characteristics were documented in the case report form (CRF) as follows: (I) demographic information including age, marry status, level of education, and employment status before surgery, (II) smoke/drink status, (III) comorbidities including hypertension, hyperlipidemia, and diabetes, (IV) histological types including squamous carcinoma, adenocarcinoma, and adenosquamous carcinoma, (V) tumor features including pathological grade, tumor size, lymph node metastasis, and FIGO stage, (VI) human papillomavirus (HPV) status. FIGO stage was classified according to the 2009 International FIGO staging system (9).
Anxiety and depression assessment
All enrolled cervical cancer patients underwent the assessment of depression and anxiety using the HADS on the day of discharge from hospital. And they were required to independently fulfill the HADS after they were given simple instructions by nurses. In terms of the controls, assessment of depression and anxiety by HADS was performed on the recruitment. When the HADS was filled out by cervical cancer patients or controls, then an independent nurse collected the scales, and calculated the HADS-anxiety (HADS-A) score as well as HADS-depression (HADS-D) score, respectively. The HADS consisted of seven questions which were scored from 0 to 3 points individually, which all together resulted in 0–21 points. And based on the HADS-A and HADS-D score, the severity of anxiety and depression was assessed as: 0–7, no anxiety/depression; 8–10, mild anxiety/depression; 11–14, moderate anxiety/depression; 15–21, severe anxiety/depression (10).
Follow up
After the surgery, based on the surgical findings, margin status, disease stage as well as cervical cancer patients’ will, observation or appropriate adjuvant treatment was administered to cervical cancer patients by their treating physicians according to the cervical cancer guidelines. And follow up was performed every 3–6 months for 2 years, every 6 months for another 3–5 years. All cervical cancer patients were consecutively followed up to death or 60 months, with the last follow up date of December 2018. Disease-free survival (DFS) was calculated from the date of surgery to the date of relapse or death. Overall survival (OS) was calculated from the date of surgery to the date of death.
Statistical analysis
Data were processed and analyzed by the SPSS 24.0 (IBM, Chicago, IL, USA) and the GraphPad Prism 6.01 (GraphPad Software Inc., San Diego, CA, USA). Normality determination for the continuous variable was determined by the Kolmogorov-Smirnov test. Continuous data were displayed as mean and standard deviation (SD) or median and inter-quartile range (IQR) as appropriate; categorical data were expressed as count (percentage). Comparisons of HADS-A and HADS-D score between two groups were determined by Student’s t-test; comparisons of anxiety and depression rate between two groups were determined by chi-square test; and comparisons of anxiety and depression severity (ordinal categorical data) between two groups were determined by Wilcoxon rank-sum test. Factors related to the anxiety or depression were determined by univariate and multivariate logistic regression model analyses. DFS and OS between groups were illustrated by Kaplan-Meier curves, and the comparisons of DFS and OS between groups were determined by the log-rank test. P value <0.05 was considered statistically significant.
Results
Study flow
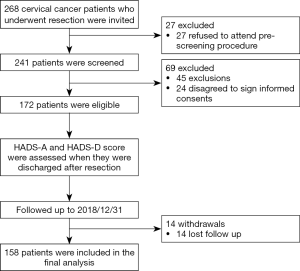
A total of 268 cervical cancer patients who underwent resection were initially invited, and 27 of them were excluded because they refused to attend pre-screen procedure (Figure 1). Two hundred and forty-one patients were further screened for eligibility, and 69 of them were excluded including 45 patients due to exclusions and 24 patients who disagreed to sign informed consents. The remained eligible 172 patients were assessed by HADS-A and HADS-D scores when they were discharged after resection and were followed up to death or consecutive 60 months. During the follow-up, 14 patients were excluded because of lost follow-up, and the remaining 158 patients were included in the final analysis.
Baseline characteristics of cervical cancer patients
The mean age of cervical cancer patients was 47.4±10.2 years (Table 1). The number of patients with education of primary school or less, high school, undergraduate and graduate or above were 15 (9.5%), 70 (44.3%), 55 (34.8%) and 18 (11.4%), respectively. As for histological type, there were 35 (22.2%) patients with adenocarcinoma, 115 (72.8%) patients with squamous carcinoma and 8 (5.1%) patients with adenosquamous carcinoma. Regarding pathological grade, there were 46 (29.1%) patients in G1, 57 (36.1%) patients in G2 and 55 (34.8%) patients in G3. Besides, there were 89 (56.3%) patients who were at FIGO stage I and 69 (43.7%) patients who were at FIGO stage II. The other detailed baseline characteristics were shown in Table 1.
Table 1
| Items | Cervical cancer patients (N=158) |
|---|---|
| Age (years), mean ± SD | 47.4±10.2 |
| Marry status, n (%) | |
| Single | 13 (8.2) |
| Married | 126 (79.7) |
| Divorced/widowed | 19 (12.0) |
| Level of education, n (%) | |
| Primary school or less | 15 (9.5) |
| High school | 70 (44.3) |
| Undergraduate | 55 (34.8) |
| Graduate or above | 18 (11.4) |
| Employment before surgery, n (%) | |
| No | 57 (36.1) |
| Yes | 101 (63.9) |
| Smoke, n (%) | 24 (15.2) |
| Drink, n (%) | 38 (24.1) |
| Hypertension, n (%) | 30 (19.0) |
| Hyperlipidemia, n (%) | 22 (13.9) |
| Diabetes, n (%) | 11 (7.0) |
| Histological type, n (%) | |
| Adenocarcinoma | 35 (22.2) |
| Squamous carcinoma | 115 (72.8) |
| Adenosquamous carcinoma | 8 (5.1) |
| Tumor size, n (%) | |
| <4 cm | 87 (55.1) |
| ≥4 cm | 71 (44.9) |
| Pathological grade, n (%) | |
| G1 | 46 (29.1) |
| G2 | 57 (36.1) |
| G3 | 55 (34.8) |
| Lymph node metastasis, n (%) | |
| No | 125 (79.1) |
| Yes | 33 (20.9) |
| FIGO stage, n (%) | |
| I | 89 (56.3) |
| II | 69 (43.7) |
| HPV status, n (%) | |
| Negative | 41 (25.9) |
| Positive | 117 (74.1) |
SD, standard deviation; HPV, human papillomavirus; FIGO, International Federation of Gynecology and Obstetrics.
Prevalence and severity of anxiety and depression between cervical cancer patients and controls
The HADS-A score was increased in cervical cancer patients (8.2±3.4) (N=158) compared with controls (4.9±2.9) (N=150) (P<0.001) (Figure 2A). The prevalence of anxiety was also elevated in cervical cancer patients (44.9%) compared with controls (16.0%) (P<0.001) (Figure 2B), and the anxiety severity of cervical cancer patients was higher compared with those in controls (P=0.001) (Figure 2C). The HADS-D score was elevated in cervical cancer patients (7.3±3.3) compared with controls (4.4±2.8) (P<0.001) (Figure 2D). The prevalence of depression was elevated in cervical cancer patients (36.1%) compared with controls as well (12.7%) (P<0.001) (Figure 2E), and depression severity was higher in cervical cancer patients compared with controls (P=0.003) (Figure 2F). These data suggested that the prevalence and severity of anxiety and depression were higher in cervical cancer patients underwent surgery compared with controls.

Factors affecting anxiety risk in cervical cancer patients
Univariate logistic regression displayed that diabetes [odds ratio (OR): 6.169, P=0.023], lymph node metastasis (OR: 2.232, P=0.045), FIGO stage II (OR: 2.080, P=0.025) were risk factors for anxiety in cervical cancer patients (Table 2). And backward stepwise multivariate logistic regression presented that diabetes (OR: 8.012, P=0.011) and FIGO stage (II) (OR: 2.394, P=0.010) were independently predictive factors for increased anxiety risk in cervical cancer patients underwent surgery.
Table 2
| Items | Logistic regression model | |
|---|---|---|
| P value | OR (95% CI) | |
| Univariate logistic regression | ||
| Age (≥40 years) | 0.193 | 1.642 (0.778–3.464) |
| Marry status | ||
| Single | Reference | Reference |
| Married | 0.603 | 1.365 (0.423–4.401) |
| Divorced/widowed | 0.837 | 1.164 (0.275–4.919) |
| Higher level of education | 0.674 | 0.921 (0.627–1.352) |
| Employment before surgery | 0.145 | 0.615 (0.320–1.183) |
| Smoke | 0.589 | 1.271 (0.533–3.034) |
| Drink | 0.144 | 1.729 (0.829–3.608) |
| Hypertension | 0.154 | 1.792 (0.803–3.999) |
| Hyperlipidemia | 0.958 | 1.025 (0.415–2.532) |
| Diabetes | 0.023 | 6.169 (1.288–29.558) |
| Histological type | ||
| Adenosquamous carcinoma | Reference | Reference |
| Adenocarcinoma | 0.942 | 1.059 (0.228–4.921) |
| Squamous carcinoma | 0.684 | 0.742 (0.177–3.116) |
| Tumor size (≥4 cm) | 0.320 | 1.377 (0.733–2.589) |
| Higher pathological grade | 0.164 | 0.754 (0.507–1.122) |
| Lymph node metastasis | 0.045 | 2.232 (1.019–4.890) |
| FIGO stage (II) | 0.025 | 2.080 (1.096–3.946) |
| HPV status (positive) | 0.604 | 1.210 (0.589–2.486) |
| Backward stepwise multivariate logistic regression | ||
| Drink | 0.099 | 1.906 (0.886–4.098) |
| Diabetes | 0.011 | 8.012 (1.619–39.660) |
| FIGO stage (II) | 0.010 | 2.394 (1.227–4.670) |
OR, odds ratio; CI, confidence interval; FIGO, International Federation of Gynecology and Obstetrics; HPV, human papillomavirus.
Factors affecting depression risk in cervical cancer patients
Univariate logistic regression exhibited that diabetes (OR: 5.333, P=0.017), lymph node metastasis (OR: 2.258, P=0.041) were risk factors for depression in cervical cancer patients (Table 3). And backward stepwise multivariate logistic regression presented that diabetes (OR: 5.713, P=0.014) and lymph node metastasis (OR: 2.382, P=0.032) were independently predictive factors for elevated depression risk in cervical cancer patients underwent surgery.
Table 3
| Items | Logistic regression model | |
|---|---|---|
| P value | OR (95% CI) | |
| Univariate logistic regression | ||
| Age (≥40 years) | 0.681 | 1.173 (0.547–2.516) |
| Marry status | ||
| Single | Reference | Reference |
| Married | 0.368 | 1.852 (0.485–7.077) |
| Divorced/widowed | 0.171 | 3.000 (0.622–14.469) |
| Higher level of education | 0.090 | 0.702 (0.466–1.057) |
| Employment before surgery | 0.880 | 0.949 (0.483–1.864) |
| Smoke | 0.283 | 1.619 (0.672–3.897) |
| Drink | 0.910 | 1.045 (0.490–2.228) |
| Hypertension | 0.081 | 2.048 (0.915–4.581) |
| Hyperlipidemia | 0.611 | 1.269 (0.506–3.184) |
| Diabetes | 0.017 | 5.333 (1.355–20.999) |
| Histological type | ||
| Adenosquamous carcinoma | Reference | Reference |
| Adenocarcinoma | 0.782 | 1.250 (0.257–6.070) |
| Squamous carcinoma | 0.836 | 0.855 (0.194–3.767) |
| Tumor size (≥4 cm) | 0.898 | 1.044 (0.544–2.004) |
| Higher pathological grade | 0.876 | 0.968 (0.644–1.455) |
| Lymph node metastasis | 0.041 | 2.258 (1.036–4.922) |
| FIGO stage (II) | 0.300 | 1.413 (0.735–2.717) |
| HPV status (positive) | 0.765 | 1.121 (0.531–2.365) |
| Backward stepwise multivariate logistic regression | ||
| Diabetes | 0.014 | 5.713 (1.429–22.844) |
| Lymph node metastasis | 0.032 | 2.382 (1.076–5.274) |
OR, odds ratio; CI, confidence interval; HPV, human papillomavirus; FIGO, International Federation of Gynecology and Obstetrics.
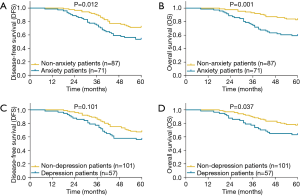
Correlation of anxiety/depression with survival profiles in cervical cancer patients
DFS (P=0.012) (Figure 3A) and OS (P=0.001) (Figure 3B) were both less prolonged in anxiety patients (n=71) compared with non-anxiety patients (n=87). Besides, DFS (P=0.101) (Figure 3C) was similar, while OS (P=0.037) (Figure 3D) was reduced in depression patients (n=57) compared with non-depression patients (n=101). These data suggested that anxiety and depression were associated with unfavorable survival profiles in cervical cancer patients underwent surgery.
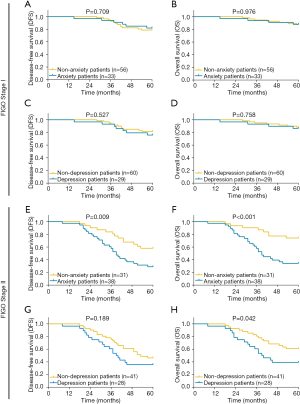
Correlation of anxiety/depression with survival profiles in subgroups
In cervical cancer patients with FIGO stage II, DFS (P=0.009) and OS (P<0.001) were decreased in anxiety patients compared with non-anxiety patients, and OS was also reduced in depression patients compared with non-depression patients (P=0.042) (Figure S1). However, in cervical cancer patients with FIGO stage I, DFS and OS were similar between anxiety patients and non-anxiety patients, between depression patients and non-depression patients (all P>0.05).
Discussion
In the present study, we found that (I) the prevalence and severity level of anxiety and depression were higher in cervical cancer patients underwent surgery compared with controls. (II) Diabetes and FIGO stage II independently predicted higher risk of anxiety, and diabetes as well as lymph node metastasis independently predicted increased risk of depression in cervical cancer patients underwent surgery. (III) Anxiety and depression were associated with unfavorable survival profiles in cervical cancer patients underwent surgery.
Cervical cancer, as one of the most fatal gynecological cancers, is reported to be associated with the emotional disorder, which is responsible for the poor quality of life and even unfavorable clinical outcomes in a long-term period (11,12). Considering reproductive and hormonal functions of the cancer site, cervical cancer patients tend to have troubles with their self-identity, self-image and reduced sexual function, which might cause psychological disorder (4). For example, one study in the Netherlands which assesses the emotional disorders among cervical cancer survivors demonstrates that 33% of the survivors have sexual distress, which co-occurs with anxiety and depression (13). Another Indonesian study exhibits that 57.5% patients have anxiety/depression, which is one of the most frequently reported problems in cervical cancer patients (14). However, there is still no study exploring the prevalence of anxiety and depression in cervical cancer patients underwent surgery, and it has been reported that surgery might influence the prevalence of anxiety and depression in several cancers other than cervical cancer (6,15). In this study, we found that the prevalence of anxiety and depression was 44.9% and 36.1% in cervical cancer patients underwent surgery, and cervical cancer patients had higher prevalence and worse severity of anxiety and depression compared with healthy individuals. Here are several possible explanations: (I) the presence of cervical cancer and the following fear of cervical cancer reoccurrence might lead to heavy psychological burden, which was responsible for the highly prevalent and aggravated anxiety/depression in cervical cancer patients underwent surgery. (II) Additionally, the impairment of physical and social functions, financial burden from treatment as well as the psychological stress of surgery might also be associated with the high prevalence and severity of anxiety/depression in cervical cancer patients underwent surgery.
Risk factors of anxiety and depression include sociodemographic characteristics, clinical characteristics, etc. in cervical cancer patients (5,16). For instance, one study indicates that financial difficulty, young age, advanced tumor stage, low physical well-being and medical co-morbidity predict a high risk of anxiety and depression in cervical cancer patients (5). Another study reveals that isolation and low socioeconomic status are associated with increased risk of anxiety and depression in cervical cancer patients after radiotherapy (4,17). These studies point out several risk factors for anxiety and depression in cervical cancer patients, however, to be specific, factors influencing the risk of anxiety and depression in cervical cancer patients after surgery are obscure. Thus, we assessed the predictive factors of anxiety or depression in cervical cancer patients underwent surgery in this study, which exhibited that diabetes, FIGO stage II were independently predictive factors for higher anxiety risk, and diabetes and lymph node metastasis were independent predictive factors for increased depression risk in cervical cancer patients underwent surgery. The possible reasons might include: (I) advanced clinical tumor features, such as FIGO stage II and lymph node metastasis, might lead to heavier emotional burden, which contribute to higher risk of anxiety and depression. (II) Besides, cervical cancer individuals suffering from diabetes might have an increased possibility of health-care utilization, functional disability and work absence, which might cause higher levels of anxiety and depression.
Some evidence illustrates the close association of anxiety and depression with cancer survivals (18-21). For example, a prior study displays that depression symptoms are associated with increased mortality in patients with lung cancer underwent surgery (20). And another study elucidates that females with depression have a higher risk of death from breast cancer after surgery (21). Although these previous studies provide the evidence for the correlation of anxiety and depression with survivals after surgery in several cancers, no related data have been reported in cervical cancer patients yet. In this study, we observed that in cervical cancer patients underwent surgery, those with anxiety had shorter DFS and OS compared with those without anxiety, and those with depression had shorter OS compared with those without depression, suggesting that anxiety and depression were negatively associated with survival profiles in cervical cancer patients underwent surgery. The possible explanations might include that: (I) cervical cancer patients with anxiety and depression were more reluctant to engage in the treatment and routine revisits, which might contribute to higher possibility of unidentified cancer recurrence and progression after surgery, leading to the poor survival in a long-term period. (II) More severe anxiety and depression might be correlated with greater tumor expression of proteinase factors which supported angiogenesis and invasion in the tumor microenvironment in cellular context, and further contributed to greater likelihood of cancer recurrence and shorter DFS after surgery. (III) Considering the close correlation of stress with neuroendocrine regulation, patients with more severe anxiety and depression might have lower ability to cope the stress, and higher stress might result in dysfunction of immune system and abnormal biologic responses to cancer, leading to unfavorable prognosis in cervical cancer patients underwent surgery (22).
There existed some limitations in our study: (I) The cervical cancer patients were recruited from single-center, more patients from multiple centers were needed to reduce selection bias. (II) The anxiety and depression were assessed by a single scale (HADS), and more anxiety and depression evaluation scales were needed to improve the validation. (III) The effect of pre-surgery anxiety and depression on post-surgery anxiety, depression and survival profiles were not investigated, which needed to be further explored.
In summary, anxiety and depression are highly prevalent, and associates with worse tumor burden as well as unfavorable survival profiles in cervical cancer patients underwent surgery.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2019.11.04). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All participants provided written informed consents before recruitment. The present study was approved by the Ethics Committee of Harbin Medical University Cancer Hospital with the approval number “KY2010-04”. And the study was conducted in accordance with the provisions of the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jim HS, Richardson SA, Golden-Kreutz DM, et al. Strategies used in coping with a cancer diagnosis predict meaning in life for survivors. Health Psychol 2006;25:753-61. [Crossref] [PubMed]
- Krebber AM, Buffart LM, Kleijn G, et al. Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psychooncology 2014;23:121-30. [Crossref] [PubMed]
- Yi JC, Syrjala KL. Anxiety and depression in cancer survivors. Med Clin North Am 2017;101:1099-113. [Crossref] [PubMed]
- Yang YL, Liu L, Wang XX, et al. Prevalence and associated positive psychological variables of depression and anxiety among Chinese cervical cancer patients: a cross-sectional study. PLoS One 2014;9:e94804. [Crossref] [PubMed]
- Klügel S, Lücke C, Meta A, et al. Concomitant psychiatric symptoms and impaired quality of life in women with cervical cancer: a critical review. Int J Womens Health 2017;9:795-805. [Crossref] [PubMed]
- Jakobsson J, Idvall E, Wann-Hansson C. General health and state anxiety in patients recovering from colorectal cancer surgery. J Adv Nurs 2016;72:328-38. [Crossref] [PubMed]
- Sharma A, Sharp DM, Walker LG, et al. Predictors of early postoperative quality of life after elective resection for colorectal cancer. Ann Surg Oncol 2007;14:3435-42. [Crossref] [PubMed]
- Pastore AL, Mir A, Maruccia S, et al. Psychological distress in patients undergoing surgery for urological cancer: a single centre cross-sectional study. Urol Oncol 2017;35:673.e1-673.e7. [Crossref] [PubMed]
- Creasman W. Revised FIGO staging for carcinoma of the endometrium. Int J Gynaecol Obstet 2009;105:109. [Crossref] [PubMed]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. [Crossref] [PubMed]
- Park SY, Bae DS, Nam JH, et al. Quality of life and sexual problems in disease-free survivors of cervical cancer compared with the general population. Cancer 2007;110:2716-25. [Crossref] [PubMed]
- Distefano M, Riccardi S, Capelli G, et al. Quality of life and psychological distress in locally advanced cervical cancer patients administered pre-operative chemoradiotherapy. Gynecol Oncol 2008;111:144-50. [Crossref] [PubMed]
- Bakker RM, Kenter GG, Creutzberg CL, et al. Sexual distress and associated factors among cervical cancer survivors: a cross-sectional multicenter observational study. Psychooncology 2017;26:1470-7. [Crossref] [PubMed]
- Endarti D, Riewpaiboon A, Thavorncharoensap M, et al. Evaluation of health-related quality of life among patients with cervical cancer in Indonesia. Asian Pac J Cancer Prev 2015;16:3345-50. [Crossref] [PubMed]
- Gold M, Dunn LB, Phoenix B, et al. Co-occurrence of anxiety and depressive symptoms following breast cancer surgery and its impact on quality of life. Eur J Oncol Nurs 2016;20:97-105. [Crossref] [PubMed]
- Kim SH, Kang S, Kim YM, et al. Prevalence and predictors of anxiety and depression among cervical cancer survivors in Korea. Int J Gynecol Cancer 2010;20:1017-24. [Crossref] [PubMed]
- Klee M, Thranov I, Machin D. Life after radiotherapy: the psychological and social effects experienced by women treated for advanced stages of cervical cancer. Gynecol Oncol 2000;76:5-13. [Crossref] [PubMed]
- Telepak LC, Jensen SE, Dodd SM, et al. Psychosocial factors and mortality in women with early stage endometrial cancer. Br J Health Psychol 2014;19:737-50. [Crossref] [PubMed]
- Barber B, Dergousoff J, Slater L, et al. Depression and survival in patients with head and neck cancer: a systematic review. JAMA Otolaryngol Head Neck Surg 2016;142:284-8. [Crossref] [PubMed]
- Sullivan DR, Forsberg CW, Ganzini L, et al. Longitudinal changes in depression symptoms and survival among patients with lung cancer: a national cohort assessment. J Clin Oncol 2016;34:3984-91. [Crossref] [PubMed]
- Liang X, Margolis KL, Hendryx M, et al. Effect of depression before breast cancer diagnosis on mortality among postmenopausal women. Cancer 2017;123:3107-15. [Crossref] [PubMed]
- Antoni MH, Lutgendorf SK, Cole SW, et al. The influence of bio-behavioural factors on tumour biology: pathways and mechanisms. Nat Rev Cancer 2006;6:240-8. [Crossref] [PubMed]


