
Rarely seen primary cardiac natural killer/T cell lymphoma: a case report
Introduction
Primary cardiac lymphoma (PCL), defined as a kind of non-Hodgkin’s lymphoma (NHL) merely involving the heart and/or pericardium (1) or NHL presenting with cardiac manifestations as well as the bulk of the tumor was located in the heart (2), is a really rare malignancy accounting for 1.3% of primary cardiac tumors and 0.5% of extra-nodal lymphomas (3).
Extra-nodal natural killer/T-cell lymphoma (ENKTL) is a distinct subtype of natural killer (NK) cell lymphoma, although uncommon in western counties, it makes up 5% to 10% of all lymphomas in Chinese people. In ENKTL, nasal cavity and other parts of the upper aerodigestive tract are primarily involved, but primary heart involvement, as far as we know, has seldom been reported.
In this report, we focus on an extremely rare case of primary cardiac NK/T-cell lymphoma arising in a 40-year-old woman, and a brief review of the literature is presented. We present the following case in accordance with the CARE-Guideline (4).
Case presentation
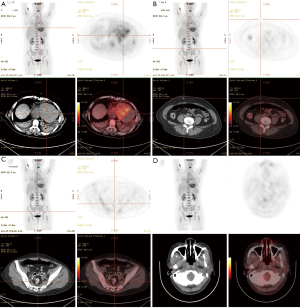
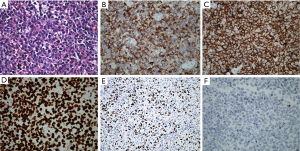
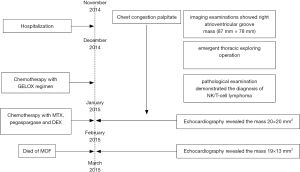
A 40-year-old Han ethnic woman without history of cardiovascular and other disorders manifesting as paroxysmal chest congestion, nausea for about 20 minutes on 15th November 2014, after five days the chest congestion reoccurred with palpitate and electrocardiogram revealed ventricular tachycardia, so amiodarone was used but failed to cardiovert. Then she was admitted to the department of cardiology of our hospital, clinical examination showed only hypotension of 97/58 mmHg, the heart rate was 112 and regular. Her hemoglobin (Hb) was 100 g/L, white blood cell (WBC) count 10.26×109/L with increased neutrophil, platelet count 337×109/L, troponin-I 2.72 ng/mL (normal range: 0–0.028). The patient was a farmer and had no history of discomforts like this. No evidence and previous history of human immunodeficiency virus, treponema pallidum and human hepatitis B virus infection. Electrocardiogram revealed T-wave inversion in V1-6, II, III, aVF leads. Coronary angiography showed only 50% stenosis of mid-left anterior descending coronary artery. CT scan and cardiac ultrasonic contrast showed an 87 mm × 78 mm mass at right atrioventricular groove and pericardial effusion. To confirm the tumor origin and find out if there were metastases, a whole-body PET/CT scan (Figure 1) was applied to this woman, and it revealed only a mass of accelerated glycolytic metabolism (SUV 7.1) at right atrioventricular groove and pericardial effusion, indicating the mass was a certain kind of malignancies. On 26th November, the patient felt sudden chest congestion, palpitate and profuse sweating, so an emergent thoracic exploring operation was performed, which showed plenty of dark red pericardial effusion, a huge mass of about 80×70×50 mm3 at right atrioventricular groove and many nodules about the size of a grain of rice on the heart surface especially on the surface of pulmonary trunk. During the emergent thoracic exploring operation, some of the nodules were collected to perform pathological examination. And eventually the histologic and immunohistochemical examination (Figure 2) demonstrated the diagnosis of NK/T-cell lymphoma, with the phenotypic features of LCA (+), Fli-1 (−), VIM (+), PCK (−), S100 (−), HMB45 (−), CD20 (−), CD79a (−), PAX-5 (−), CD2 (+), CD3 (+), CD5 (−), CD43 (+), mum-1 (−), bcl-2 (+), CD10 (−), bcl-6 (−), CD56 (+), GrB (−), CD30 (−), ALK (−), CD68 (−), TdT (−), MPO (−), TIA-1 (+), SMA (−), EMA (−), CD31 (−), CD34 (−), des (−), Ki-67 (Li 96%).
After recovery from the surgery, the patient was transferred to our department, and then we conducted some further examinations. Bone marrow cytology and biopsy inspection showed no signs of bone marrow involvement. Serum troponin-I level was 1.029 ng/mL and lactate dehydrogenase (LDH) 382 U/L (normal range: 135–214), quantification of circulating Epstein-Barr virus (EBV)-DNA was 1.98×105 copies/mL (normal range: <500 copies/mL). Thus the final diagnosis was primary cardiac NK/T cell lymphoma (Ann Arbor stage IE, IPI score 1). On 12th December the GELOX regimen was applied to the patient (Gemcitabine 1,500 mg as an intravenous drip on day 1 and day 8, oxaliplatin 150 mg as an intravenous drip on day 1, pegaspargase 3,750 IU as an intramuscular injection on day 1). After chemotherapy the patient’s fibrinogen seriously decreased so before she left hospital fresh frozen plasma was infused, in addition LDH level and EBV-DNA were reexamined as the results of 226 U/L and 9.99×103 copies/mL, respectively. The patient no longer complained with chest congestion when came back to hospital, and her LDH was 242 U/L and EBV-DNA 5.53×104 copies/mL, other standard laboratory tests disclosed no obvious abnormalities except mild anemia. Echocardiography revealed the mass at right atrioventricular groove was 20×20 mm2. Next the patient received chemotherapy as following: methotrexate (MTX) 4,800 mg as a continuous intravenous drip on day 1 (with calcium folinate to rescue), pegaspargase 3,750 IU as an intramuscular injection on day 2, dexamethasone (DEX) 40 mg as an intravenous drip from day 1 to 4. Just like the previous, fresh frozen plasma was infused, furthermore granulocyte-colony-stimulating factor (G-CSF) was utilized as a consequence of neutropenia. Similarly, before the third course some laboratory tests were conducted, LDH was 320 U/L and EBV-DNA 1.17×104 copies/mL, WBC count was 1.5×109/L with neutrophil count 0.22×109/L, Hb 66g/L and Plt count 93×109/L, coagulation function tests were normal. Echocardiography revealed the mass was 19×13 mm2. The patient received G-CSF and blood transfusion in advance of the chemotherapy as same as the second course. After chemotherapy the patient suffered from severe fibrinogen decrease and grade IV marrow suppression with neutrophil count as little as 0.01×109/L, PLT count 8×1012/L. Some days later, gastrointestinal bleeding and pulmonary infection arose, finally the patient died of multiple organ failure (MOF) despite various active treatments, and the last detection of EBV-DNA was 8.3×103 copies/mL. The timeline of interventions and outcomes was summarized as Figure 3.
Discussion
According to Petrich et al. (5) who analyzed the characteristics of 197 patients diagnosed of PCL and reported in the literature, PCL is more common in elderly people with the median age of 63-year-old (9 to 90-year-old), and has a male predominance with the male-to-female ratio of 1.94. Symptoms at onset are non-specific, dyspnea was most common, and other common symptoms were arrhythmia, chest pain, constitutional complaints including fever, chills, sweats and weight loss, while few patients presented with superior vena cava syndrome. In 179 of 197 cases who had described chamber involvement, 92% affected the right chambers, and the right atrium was most frequently compromised followed by right ventricle, left atrium and left ventricle.
As to the female patient we reported, she was in her forties and right ventricle was involved, with no specific symptoms at onset. But PCL related ventricular tachycardia (VT) was not so common in literatures. Since the mass presenting in our case invaded right ventricle myocardium, we supposed that the likely mechanism accounting for PCL related VT is just similar with some cardiomyopathies, such as hypertrophic cardiomyopathy that has been tightly associated with the development of VT (6). Moreover, the real specificity of this case consists in the histological type—NK/T cell lymphoma. As is reported, the overwhelming majority of PCL is B-cell origin, among which the subtype of diffuse large B-cell lymphoma (DLBCL) is the most common (5,7). Primary cardiac T-cell lymphomas are extremely rare and only have been reported as single-case reports both in adults and children, especially in immunocompetent individuals (8-12), and interestingly, in 4 of 9 cases the pathological type was T cell lymphoblastic lymphoma (T-LBL), which requires to accumulate more cases to explore whether the T-LBL is the most common type of T-cell PCL. And of note, to the best of our knowledge, this is the second reported primary cardiac NK/T-cell lymphoma (12), but not like the case we reported, CT scan of other parts or PET/CT scan were not performed in literature (12) so that the diagnosis of PCL was not absolutely precise.
The diagnosis of PCL is usually delayed for reasons of its rarity and insufficient recognition. Chest CT scan, echocardiography including transthoracic of transesophageal, magnetic resonance imaging are all useful diagnostic techniques, but the final diagnosis should to be confirmed by pathological examination through needle biopsy even thoracic surgery, as well as cytology of pericardial diffusion that was reported to be diagnostic in 60% of cases (13).
As for its rarity, the best therapeutic approach to PCL was not established, but similarly to other NHLs, chemotherapy and/or radiotherapy were mostly taken, with surgery not improving the therapeutic effect (14). And as to ENKTL, a highly aggressive disease with grim prognosis, whose optimal treatment strategies have not been fully defined, often showed limited response to conventional chemotherapy regimens such as CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), at least partly because of frequent multidrug resistance gene expression by tumor cells (15). So different with Lepeak et al. reported (12), at beginning we chose the GELOX regimen, which was proved superior to CHOP regimen in early stage ENKTL patients (16). Furthermore, ENKTL shows a tight association with Epstein-Barr virus (EBV), and the plasma EBV-DNA load at presentation is associated with clinical disease stage and treatment response, the rapid drop of EBV-DNA during therapy is a good maker of outcome (17,18). Thus, when the load of EBV-DNA was higher than that at the end of the first course, the more intensive regimen consisting of L-asparaginase, methotrexate and dexamethasone, which has been evaluated to be effective in patients with refractory or relapsing ENKTL (19), was applied to the patients in the second course with the consideration of not only improving the efficacy but also preventing central nervous system invasion. However, the more intensive therapy brought about more severe side effects, to some extent leading to the fatal complications. Radiation therapy (RT) alone, as an important treatment modality for localized disease, could produce complete response rates of up to 70% (20), but disappointingly, the efficacy of sequential RT to NK/T cell PCL was finally not able to be estimated in our case.
After all, PCL are exceedingly rare events, with its standard treatment strategies and prognosis not been fully determined, and when dealing with PCL, both the particular original site and the pathological type should be taken into account. As we emphasized in this case of NK/T cell PCL, who achieved a partial remission with at least 50% tumor mass reduction, novel effective regimen and the role of EBV-DNA testing are of great importance.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2019.11.42). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- McAllister HA, Fenoglio JJ. Tumors of the cardiovascular system. In: Atlas of Tumor Pathology. 2nd Series. Fascicle15. Washington, DC: Armed Forces Institute of Pathology; 1978:99-100.
- Burke A, Virmani R. Tumors of the heart and great vessels. In: Atlas of Tumor Pathology. 3rd Series. Fascicle 16. Washington, DC: Armed Forces Institute of Pathology; 1996:171-9.
- Gowda RM, Khan IA. Clinical Perspectives of Primary Cardiac Lymphoma. Angiology 2003;54:599-604. [Crossref] [PubMed]
- Riley DS, Barber MS, Kienle GS, et al. CARE 2013 Explanations and Elaborations: Reporting Guidelines for Case Reports. J Clin Epidemiol 2017;89:218-35. [Crossref] [PubMed]
- Petrich A, Cho SI, Billett H. Primary cardiac lymphoma: an analysis of presentation, treatment, and outcome patterns. Cancer 2011;117:581-9. [Crossref] [PubMed]
- Moon JCC, McKenna WJ, McCrohon JA, et al. Toward clinical risk assessment inhypertrophic cardiomyopathy withgadolinium cardiovascular magnetic resonance. J Am Coll Cardiol 2003;41:1561-7. [Crossref] [PubMed]
- Miguel CE, Bestetti RB. Primary cardiac lymphoma. Int J Cardiol 2011;149:358-63. [Crossref] [PubMed]
- Deepti AN, Noone ML, Mahadevan A, et al. Primary cardiac cytotoxic T-cell lymphoma presenting with neurological deficits: a case report. Cardiovasc Pathol 2008;17:334-8. [Crossref] [PubMed]
- Li B, Li R, Wu B, et al. Primary Cardiac T Cell Lymphoma. J Card Surg 2012;27:457-60. [Crossref] [PubMed]
- Park HK, Choi JY, Park YH. Primary Cardiac T Cell Lymphoma in a Child. Pediatr Cardiol 2006;27:177-9. [Crossref] [PubMed]
- Patel J, Sheppard MN. Primary cardiac T-cell lymphoma in a child. Eur Heart J 2009;30:2713. [Crossref] [PubMed]
- Lepeak LM, Yang DT, Chang JE. Extranodal NK/T-cell lymphoma presenting with primary cardiac involvement. Hematol Rep 2011;3:e9. [Crossref] [PubMed]
- Anghel G, Zoli V, Petti N, et al. Primary Cardiac Lymphoma: Report of Two Cases Occurring in Immunocompetent Subjects. Leuk Lymphoma 2004;45:781-8. [Crossref] [PubMed]
- Chalabreysse L, Berger F, Loire R, et al. Primary cardiac lymphoma in immunocompetent patients: a report of three cases and review of the literature. Virchows Arch 2002;441:456-61. [Crossref] [PubMed]
- Yamaguchi M, Kita K, Miwa H, et al. Frequent expression of P-glycoprotein/MDR1 by nasal T-cell lymphoma cells. Cancer 1995;76:2351-6. [Crossref] [PubMed]
- Wang L, Wang WD, Xia ZJ, et al. Combination of gemcitabine, l-asparaginase, and oxaliplatin (GELOX) is superior to EPOCH or CHOP in the treatment of patients with stage IE/IIE extranodal natural killer/T cell lymphoma: a retrospective study in a cohort of 227 patients with long-term fol. Med Oncol 2014;31:860. [Crossref] [PubMed]
- Kim HS, Kim KH, Kim KH, et al. Whole blood Epstein-Barr virus DNA load as a diagnostic and prognostic surrogate: extranodal natural killer/T-cell lymphoma. Leuk Lymphoma 2009;50:757-63. [Crossref] [PubMed]
- Au WY. Quantification of circulating Epstein-Barr virus (EBV) DNA in the diagnosis and monitoring of natural killer cell and EBV-positive lymphomas in immunocompetent patients. Blood 2004;104:243-9. [Crossref] [PubMed]
- Jaccard A, Gachard N, Marin B, et al. Efficacy of L-asparaginase with methotrexate and dexamethasone (AspaMetDex regimen) in patients with refractory or relapsing extranodal NK/T-cell lymphoma, a phase 2 study. Blood 2011;117:1834-9. [Crossref] [PubMed]
- Wang L, Wang Z, Chen X, et al. First-line combination of gemcitabine, oxaliplatin, and L-asparaginase (GELOX) followed by involved-field radiation therapy for patients with stage IE/IIE extranodal natural killer/T-cell lymphoma. Cancer 2013;119:348-55. [Crossref] [PubMed]


