Giant posterior mediastinum dumbbell schwannoma: a case report
Introduction
Neurogenic tumors are the most radical mediastinal tumors, 75–95% of which occur in the posterior mediastinum. The majority of these tumors are benign and have a low incidence rate. Most of the published articles on these tumors are case reports. Here, we report the case of a patient with giant right posterior mediastinum dumbbell schwannoma with unique numbness and weakness of both lower limbs as the main symptoms who visited our department for treatment. The clinical data of this case were analyzed and the relevant literature was reviewed to improve our understanding of the clinical characteristics, diagnosis, treatment, and prognosis of mediastinal neurogenic tumors.
Case presentation
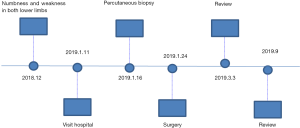
A 63-year-old female patient visited our hospital on January 11, 2019, with complaints of numbness and weakness in both lower limbs for more than 1 month. Other symptoms such as drooping eyelids, dysphagia, unclear speech, fever, cough, expectoration, chest tightness, suffocation, night sweats, chills, chest pain, palpitation, abdominal pain, hematemesis, and black stools were absent. Since the onset of numbness and weakness, the patient experienced no deterioration in spirit, diet, sleep quality, or bowel and bladder functions and no significant weight loss. The patient’s personal and family medical history was unremarkable. Physical examination showed sanity, no enlargement of the superficial lymph nodes, the trachea located in the midline, no chest deformity, no ulcer, spider nevus in the chest skin, normal respiratory motility, solid sound on percussion of the right lower lung field, weak breath sound in the right lower lung field and clear breath sound in the rest of the lung on auscultation, no dry or moist rales, right lower limb muscle strength of level 1, and left lower limb muscle strength of level 4, numbness in both lower limbs, especially for the right. The movement and sensation of both upper limbs were normal. Her electrocardiogram and laboratory findings showed no significant abnormality. A preoperative computed tomography (CT) scan showed the presence of a large soft and solid mass of 18 cm × 15 cm × 9 cm in size in the right posterior mediastinal spine, with round, clear boundaries, smooth edges, and uneven internal density with uneven enhancement (Figure 1). The lesion had destroyed the 10th thoracic vertebra, including the vertebral body and vertebral pedicle, and entered the vertebral canal, resulting in spinal cord compression at that level. Based on these CT results, we next decided to perform CT-guided puncture biopsy of the lesion to determine whether it was benign or malignant. The pathological findings of the biopsy specimen suggested schwannoma, a benign tumor. Therefore, surgical resection was selected as the treatment course and performed on January 23, 2019, with the patient under general anesthesia. First, removal of thoracic vertebral lesions by decompression internal fixation was performed by an orthopedist using a posterior midline incision, followed by the resection of the giant right mediastinal schwannoma by us using a left lateral incision. If the biopsy results showed a malignancy, then the treatment we choose would be chemotherapy without surgical resection.
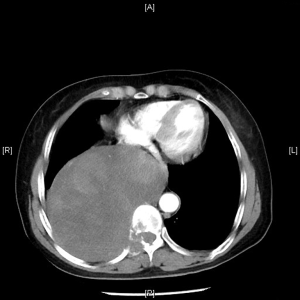
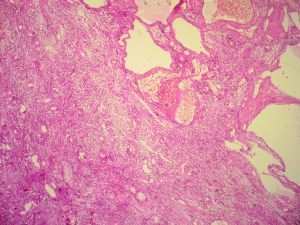
Because the biopsy results revealed schwannoma, surgical resection was performed. During the operation, the right thoracic giant mass was found to be completely solid (Figure 2). The right thoracic giant mass was found to be completely fixed during the operation. The resection was successful. The postoperative pathological testing of the right posterior mediastinal mass confirmed schwannoma (Figure 3). Finally, it was diagnosed as giant posterior mediastinum dumbbell schwannoma, compressed destruction of the 10th thoracic vertebra, muscle weakness of both lower limbs and osteoporosis. During the operation, it was found that the patient had severe osteoporosis and the nail fixation of the thoracic vertebra was not firm. The nails were placed so deep that it cut the surgeon’s glove during the removal of the mediastinal tumor. The tumor is large and easy to bleed. Postoperative recovered of the patient was good, with right muscle strength recovered to level 4 and left muscle strength recovered to level 4+, no numbness in both lower limbs, as noted during follow-up on March 3, 2019. In September, she walked independently to review, the muscle strength and sensation of both lower limbs were normal (Figure 4).
Discussion
Most neurogenic tumors originate from the posterior mediastinal paravertebral gutter, whereas a few partially occur in the intervertebral foramen, resulting in a dumbbell-shaped tumor growth. The classification of neurogenic tumors is complex and is based on the primary cell: it can be derived from the nerve sheath cells of the peripheral nervous system or the spinal ganglion cells of the autonomic nervous system (1). Mediastinal neurogenic tumors grow slowly and lack specific clinical manifestations. Common clinical symptoms include chest and back pain, cough, chest tightness and shortness of breath, superior vena cava obstruction syndrome, and Horner syndrome. The numbness and weakness in both lower limbs observed in our patient are rare symptoms. Our case highlights three critical points. First, we performed a biopsy to rule out malignancy. If malignancy had been detected, chemotherapy without surgical resection would have shown a better prognosis. Second, the lesion destroyed the 10th thoracic vertebra, including the vertebral body and vertebral pedicle, and entered the vertebral canal, leading to spinal cord compression over several years. This finding should not suggest that the lesion was malignant. Third, the pathological findings of the biopsy specimen also revealed that the tumor was benign. Thus, we selected surgical resection as the treatment course in which the spine tumor was first resected by an orthopedic surgeon, followed by the resection of the intrathoracic tumor by us. This procedure was preferred instead of first opting for thoracic tumor resection, which would require a recovery period before the subsequent orthopedic surgery.
Mediastinal neurogenic tumors occurring in the nerve root of the intervertebral foramen may be accompanied by symptoms of spinal cord compression. Preoperative imaging, such as CT or magnetic resonance imaging (MRI), is the main preliminary diagnostic procedure for such tumors as it can provide the accurate location of the tumor and its relationship with adjacent structures and can suggest its nature (benign/malignant). In particular, in cases of dumbbell tumors, chest MRI or CT can clearly show the position and shape of the tumor, its relationship with the surrounding tissue structures, the expansion of the intervertebral foramen, and the compression and erosion of the bone. MRI and CT results can guide the planning of the surgical course to avoid the occurrence of intraoperative complications (2). For large tumors near the chest wall, preoperative pathology of a biopsy specimen can guide the selection of an appropriate treatment. In our case, preoperative puncture biopsy followed by pathological confirmation of the biopsy specimen was performed as the lesion was large.
The type of surgical incision should be selected based on the tumor size and location and the presence of spinal canal invasion. A posterolateral incision offers good exposure and is suitable for the resection of posterior mediastinal and large anterior middle mediastinal neurogenic tumors. Thoracic dumbbell tumor, a special type of mediastinal neurogenic tumor, accounts for approximately 10% of all cases of mediastinal neurogenic tumors. Most of these tumors originate from spinal nerves and involve the upper mediastinum more commonly than the lower mediastinum. Resection of the intrathoracic tumor can be performed by a thoracic surgeon after an orthopedic surgeon first opens the vertebral plate and resects the intraspinal canal tumor, thus allowing increased operation space for the subsequent resection. This can help minimize the occurrence of spinal canal hematoma and avoid vertebral canal hemorrhage, spinal cord compression, or direct spinal cord injury, all of which may have serious consequences. During the operation, complete hemostasis should be achieved and the dural membrane should be tightly sutured. If necessary, muscle flap stuffing and artificial dural coverage may be used to strengthen the dural membrane to prevent epidural hematoma or cerebrospinal fluid leakage (3).
Our case had two issues. First, because schwannomas, especially large tumors, are prone to bleeding, blood preparation should be made before surgery, and preoperative tumor embolization may reduce tumor vascularity and operative blood loss thereby permitting safer resection (4), which was not done in our case. Second, our patient was an elderly female in whom the bone was compressed for several years and who was found to be severely osteoporotic during the operation. Elderly patients should start supplementing calcium and vitamin D before surgery to assist in orthopedic surgery.
The clinical applications of thoracoscopy have expanded greatly in recent years. It is a minimally invasive, efficient, and safe procedure. Thoracoscopic resection can be performed for tumors with a diameter of <6 cm and no obvious external invasion. For tumors >6 cm in diameter and located at the apex, the applicability of thoracoscopic resection depends on whether the tumor is cystic or solid. For large cystic tumors, partial cystic fluid decompression can first be released to shrink the tumor and facilitate the operation under a microscope. Large solid tumors may be excised with small incisions (5). Contraindications for thoracoscopic surgery include a preoperative pathological diagnosis of obvious external invasion of malignant tumors; substantial mass with severe adhesion to peripheral blood vessels or important organs; and large solid tumors. Currently, the surgical resection of dumbbell-shaped neurogenic tumors is mainly performed with a posterior lateral thoracotomy incision combined with a posterior median incision, which is relatively traumatic. Whether thoracoscopic surgery can be used for resecting these tumors is still controversial, and some scholars consider it a surgical taboo. However, owing to further advancements in the minimally invasive techniques of thoracoscopy, in one study, the authors adopted posterior median incision combined with thoracoscopy-assisted surgery to first remove the lamina and the tumor in the spinal canal and subsequently performed thoracoscopic resection of intrathoracic paravertebral tumors. This procedure is expected to be an ideal surgical method for resecting mediastinal dumbbell-shaped neurogenic tumors. Because the tumor was giant and solid in our case, we used posterior midline incision for the resection of the spinal lesion, followed by left lateral incision for the resection of the giant right mediastinal schwannoma.
Radical surgical resection should be the procedure of choice for removing posterior mediastinum dumbbell schwannoma as it shows good prognosis with rare incidence of malignant transformation.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2020.01.28). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ayub S, Shakoor MT, Hasan S, et al. Mediastinal mass diagnosed as a benign schwannoma. Singapore Med J 2011;52:e167-9. [PubMed]
- Razek AAKA, Ashmalla GA. Assessment of paraspinal neurogenic tumors with diffusion-weighted MR imaging. Eur Spine J 2018;27:841-6. [Crossref] [PubMed]
- Chen X, Ma Q, Wang S, et al. Surgical treatment of posterior mediastinal neurogenic tumors. J Surg Oncol 2019;119:807-13. [Crossref] [PubMed]
- Loftus TJ, Pipkin M, Machuca T, et al. Angiographic embolization followed by piecemeal resection of giant posterior mediastinal schwannoma: Case report and concise review. Int J Surg Case Rep 2018;53:250-3. [Crossref] [PubMed]
- Li Y, Wang J. Experience of video-assisted thoracoscopic resection for posterior mediastinal neurogenic tumours: a retrospective analysis of 58 patients. ANZ J Surg 2013;83:664-8. [Crossref] [PubMed]