The natural history of oral mucosal lesions with both lichenoid and epithelial dysplastic features: a systematic review
Introduction
It is not uncommon to find mild epithelial dysplastic changes in oral inflammatory lesions. Similarly, cases of oral epithelial dysplasia (OED) can present with features of stromal inflammation. In such cases, the diagnosis is often rendered based on what the pathologist considers as the primary pathology. In cases of established (moderate to severe) OED with signs of mild non-specific inflammation, epithelial dysplasia is regarded as the primary pathology and the inflammation is attributed as a reaction to the dysplasia (1-4). In a predominantly inflammatory lesion with signs of mild epithelial dysplasia, the inflammation is considered as the primary pathology while dysplasia is considered as reactionary atypia secondary to the inflammation.
There are two major drawbacks with the above presumptions:
- Determining the primary pathology based on the predominant features may be misleading as it is possible that a mild epithelial dysplasia has elicited a strong inflammatory reaction, or a mild inflammation has led to prominent atypical changes resembling true epithelial dysplasia;
- Recent studies have provided proof that mild epithelial dysplasia in predominantly inflammatory lesions including oral lichen planus (OLP) and oral lichenoid lesion (OLL) has a malignant potential equal to that of OED (5,6). Thus, the epithelial changes in OLP and OLL which are often disregarded as the reactionary atypia to inflammation could represent a true epithelial dysplastic change. It is also vital to acknowledge that epithelial dysplasia irrespective of whether it is primary or secondary features has a malignant risk and must be closely followed up (4-6).
What is the need for establishing the primary pathology?
If epithelial dysplasia, irrespective of whether it is primary or a secondary feature can impart a malignant potential, then the question arises as to the importance of establishing the primary pathology. The following reasons emphasize the clinical significance of diagnosing the primary pathology:
- In case, the primary inflammatory lesion is proven to show true dysplastic changes in the absence of known risk factors, then it can be assumed that the respective inflammatory lesion (OLP or OLL) has inherent malignant potential. Thus, such cases irrespective of the presence of dysplasia or associated risk factors can be classified as oral potentially malignant disorders (OPMDs) and must be closely followed up for signs of malignant transformation (2-4);
- To facilitate accurate estimation of epidemiological data. At present, the prevalence, incidence and malignant transformation rate of oral mucosal lesions presenting with both lichenoid and dysplastic features have been either over or under-represented due to the absence of universally accepted diagnostic criteria. Thus, by accurately identifying the primary pathology, precise epidemiological data can be estimated. Based on the transformation rate obtained from the epidemiological data, the treatment plan and follow-up can be formulated for each of these entities (1-3,7). The present systematic review was undertaken to assess the natural history of oral mucosal lesions presenting with both lichenoid and epithelial dysplastic features. Understanding their true nature could aid in accurately diagnosing and treating these enigmatic entities.
Methods
Protocol and registration
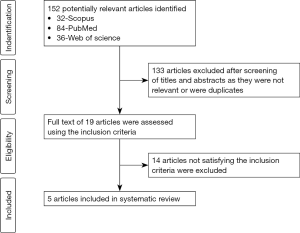
A thorough screening of the International prospective register of systematic reviews (PROSPERO) databases was made to confirm that there were no similar systematic reviews. After establishing the primary protocol, the systematic review was registered with PROSPERO and was allotted the registration number CRD42019118656. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were strictly followed. Figure 1 illustrates the PRISMA flowchart summarizing the search strategy of the study
Eligibility criteria
Inclusion criteria
Original study articles in the English language where the cases exhibited both lichenoid and dysplastic features and provided sufficient clinicopathological details were included.
Exclusion criteria
Articles with cases that did not have both lichenoid and epithelial dysplastic features or exhibited features of malignancy at the first diagnosis or did not provide sufficient clinicopathological details. Narrative reviews, systematic reviews, and meta-analysis, case reports/series, and articles not in English language.
Focused question
What is the natural history of oral mucosal lesions presenting with both lichenoid and epithelial dysplastic features?
Search strategy
A literature search was performed in Scopus, PubMed, and Web of Science on all articles published till July 2019 using the keywords “oral lichenoid dysplasia; OED with lichenoid features; OLP with dysplastic features; OLL with dysplastic features”.
Study selection and data extraction
Articles were selected for the systematic review in 2 stages. The first stage involved screening by two independent reviewers (ATR and SGP) of the titles and abstracts of all the identified articles to eliminate any potential duplicates and irrelevant articles. The second stage involved the assessment of the full texts of the remaining articles by the reviewers using the eligibility criteria. Kappa statistics were carried out to assess inter-observer reliability. Data including the author’s name, year of publication, country of origin, clinicopathological features, number of cases and the corresponding diagnosis rendered, and follow-up data (if available) were extracted from the included articles.
Results
Study selection
The search terms yielded a total of 152 (PubMed-84, Scopus-32, Web of Science-36) articles. After removing the 133 irrelevant and duplicates articles based on their titles and abstracts, the full text of the remaining 19 articles was assessed using the inclusion criteria. Only 5 of the 19 articles satisfied all the inclusion criteria, including the provision of sufficient clinicopathological details. Out of the 5 included studies, 181 cases were described to have both lichenoid and epithelial dysplastic features. Kappa’s value between the two reviewers for the first step of the review was 0.98 and the second step was 1. Table 1 summarizes the data extracted from the included studies.
Table 1
| S. No. | The first author/year/country of origin (reference number) | Aim and objective | Characteristics and diagnosis rendered of oral mucosal lesions presenting with both lichenoid and epithelial dysplastic features | Cases included in the study |
|---|---|---|---|---|
| 1 | Shearston et al./2019/Australia (8) | Determine the malignant potential of OLP, OLL, OLD | Oral mucosal lesions with features typical of OLP with except for the presence of epithelial dysplasia were diagnosed as OLD (and) oral mucosal lesions with features of OLL with epithelial dysplasia were diagnosed as OLD | Total cases included: 44 cases |
| Histopathological features of epithelial dysplasia with a background of OLP/lichenoid infiltrate | ||||
| Other relevant details: 5 years follow-up showed the malignant transformation of 3 cases | ||||
| 2 | Sanketh et al./2019/India (9) | Differentiating OLP with and without dysplasia, OED with and without lichenoid features using p53, ki-67, α-SMA, and COX-2 | Oral mucosal lesions with features typical of OLP with the except for the presence of epithelial dysplasia were diagnosed as OLP with dysplasia | Total cases included: 9 cases; 5 cases: histopathological features of OLP with epithelial dysplasia |
| Oral mucosal lesions with epithelial dysplasia and lichenoid inflammation were diagnosed as OLD | 4 cases: histopathological features of epithelial dysplasia with lichenoid inflammation | |||
| Other relevant details: the markers could not differentiate the study groups | ||||
| 3 | Rock et al./2018/Canada (5) | To compare the malignant nature of epithelial dysplasia with and with oral lichenoid mucositis (OLM) | Oral mucosal lesions with OLP or OLL features (OLM) with the presence of epithelial dysplasia were diagnosed as OLM with dysplasia | Total cases included: 73 cases |
| Histopathological features of epithelial dysplasia and OLM. The OLM in the study could be representing OLP or OLL | ||||
| Other relevant details: 5 years follow-up showed the malignant transformation of 6 cases and the transformation rate was similar to that of OED | ||||
| 4 | Patil et al./2015/India (7) | Investigating the existence of OLD | Oral mucosal lesions only compatible with OLP due to the lack of at least one typical feature (unilateral presentation; mixed deep inflammatory infiltrate, basal cell degeneration, presence of epithelial dysplasia) were diagnosed as OLL with dysplasia | Total cases included: 41 cases |
| 8 cases: clinical presentation: Bilateral presentation with at least a minor reticular component; histopathological presentation: subepithelial inflammatory band predominantly of lymphocytes; basal cell degeneration; presence of epithelial dysplasia | ||||
| 4 cases: clinical presentation: Unilateral presentation with at least a minor reticular component; histopathological presentation: Subepithelial inflammatory band predominantly of lymphocytes; basal cell degeneration; presence of epithelial dysplasia | ||||
| 4 cases: clinical presentation: bilateral presentation with at least a minor reticular component; histopathological presentation: mixed inflammatory infiltrate extending into deeper portions of the connective tissue; basal cell degeneration; presence of epithelial dysplasia | ||||
| Oral mucosal lesions with epithelial dysplasia and lichenoid inflammation were diagnosed as OLD | 3 cases: clinical presentation: predominant cases were unilateral (the specific number could not be obtained for this subgroup); histopathological presentation: mixed inflammatory infiltrates (lymphocytes and plasma cells) extending to deep connective tissue; presence of epithelial dysplasia | |||
| 22 cases: clinical presentation: Specific clinical type of presentation (reticular/plaque) is not mentioned. Although the bilateral/unilateral presentation pattern is mentioned for all the cases included as OED, these details have not been specified for the 22 OED cases shown to exhibit lichenoid features; histopathological presentation: epithelial dysplasia with mixed lichenoid inflammation in 15 cases and basal cell degeneration in 7 cases | ||||
| 5 | Jaafari-Ashkavandi et al./2011/Iran (10) | Analysis of clinicopathologic features of OLP | Oral mucosal lesions typical of OLP except for the presence of epithelial dysplasia was diagnosed as dysplastic OLP | Total cases included: 14 cases |
| Clinical presentation: 11 were keratotic and 3 were erosive-ulcerative; histopathological presentation: subepithelial inflammatory band predominantly of lymphocytes; basal cell degeneration; presence of epithelial dysplasia | ||||
OLL, oral lichenoid lesion; OLD, oral lichenoid dysplasia; OLP, oral lichen planus; OLM, oral lichenoid mucositis.
Data collected
Of the 5 included studies (5,7-10), two were from India (7,9), one from Canada (5), one from Australia (8) and one from Iran (10). The various diagnosis rendered among these 181 cases included OLD (n=73); OLP with epithelial dysplasia/dysplastic OLP (n=19); oral lichenoid mucositis (OLP or OLL) with epithelial dysplasia (n=73); OLL with dysplasia (n=16). Follow-up data from the included studies showed the malignant transformation of a few cases diagnosed as OLD and OLM (OLP or OLL) with dysplasia.
Discussion
Oral mucosal lesions presenting with both lichenoid and epithelial dysplastic features are often misdiagnosed. The cause for the misdiagnosis in most of these cases is due to the difficulty in identifying the primary pathology and the lack of universally accepted diagnostic criteria (1-4,7,9). The present review analyses the varied spectrum of clinicopathological features and diagnoses rendered in original studies investigating oral mucosal lesions with both lichenoid and epithelial dysplastic features. Only cases that provided sufficient clinicopathological details were included in the review. Cases exhibiting malignant features at the first diagnosis were excluded as in such cases, the natural history of the lesion cannot be determined. The included cases were diagnosed as 4 major entities including OLP with dysplasia/dysplastic OLP, OLD, OLL with dysplasia, OLM with dysplasia. The diagnosis depended primarily on whether the concerned authors accepted the presence of epithelial dysplasia in OLP or not. The entity OLM with dysplasia entailed both OLL and OLP lesions exhibiting epithelial dysplasia (5), thus can, in turn, be classified as OLP with dysplasia and OLL with dysplasia. The three enigmatic oral mucosal lesions exhibiting lichenoid and epithelial dysplastic features (OLP with dysplasia, OLL with dysplasia, and OLD) in the included articles are discussed below.
OLD
OLD as an entity was first proposed by Krutchkoff et al. in 1985 (11,12). OLD represents a primary OED with secondary lichenoid features. Being a primary dysplastic lesion, the patients may have a history of known risk factors including tobacco, alcohol, etc. The clinical features of OLD are nonspecific which may be unilateral or bilateral, plaque/erosive/ulcerative/reticular presentations. The secondary lichenoid features may range from mild to severe inflammation in the connective tissue. The inflammatory pattern is non-specific ranging from a sub-epithelial band as noted in OLP to diffuse mixed inflammatory infiltrates resembling OLL. The inflammation is presumed to be a reaction to the epithelial dysplasia. The inflammatory component in OLD is not clinically significant but often leads to misdiagnosis. In such cases, it is vital to observe the basal cell layer. OLD like OED does not have basal cell degeneration as a major diagnostic feature. Thus, any sign of basal cell degeneration should invite the possibility of the lesion more likely being OLP or OLL with secondary dysplastic features (1-4). But, the presence of basal cell degeneration cannot be designated as an exclusion criterion for OLD, as it, in turn, would cause diagnostic dilemmas similar to van der Meij criteria (13,14) excluding epithelial dysplasia from OLP.
OLP with dysplasia
The definition and clinicopathological criteria for OLP have been constantly modified due to the lack of understanding of its natural history. OLP represent an oral mucosal lesion wherein the inflammatory component represents a reaction to the antigens expressed by the basal keratinocytes. The inflammatory reactions to these self-antigens lead to the degeneration of the basal cells of the epithelium. The inflammatory component is intense but restricted to the sub-epithelial connective tissue resembling a band. The inflammation is primarily composed of T-lymphocytes. Clinically the lesion has a bilateral presentation. Although several patterns (reticular, erosive, atrophic, etc.) are part of the diverse clinical spectrum of OLP, it is mandatory that at least a minor reticular component is present to diagnose the lesion as OLP (13,14). The debate as to the natural history of OLP arises in the presence of dysplastic features in the epithelium.
Despite satisfying most clinicopathological criteria including a bilateral presentation, presence of a reticular component, sub-epithelial lymphocytic band, and basal cell degeneration, the diagnosis of OLP is often excluded due to the presence of epithelial dysplasia. The reason for exclusion stems from hypothesis put forth by Krutchkoffs et al. (11,12), wherein they considered lesions that were typical of OLP clinicopathologically but had epithelial dysplasia to actually represent OLD, wherein the subtle features of epithelial dysplasia might have been missed during the initial diagnosis due to the inflammatory infiltrate. In addition, Krutchkoffs et al. suggested that WHO 1978 (15) criteria for OLP were very liberal wherein cases with both unilateral/bilateral presentation, all clinical pattern irrespective of the presence of reticular component where all diagnosed as OLP, thus causing an overrepresentation of the prevalence and malignant potential of OLP. Although it is agreeable that the WHO criteria of 1978 (15) were relatively less stringent in diagnosing OLP, it is equally important to note that Kruchkoffs criteria (11,12) which were based on the premise that cases of OLP presenting with dysplasia actually represent misdiagnosed OLD could lead to underrepresentation of OLP’s prevalence and malignant potential. Similar to Krutchkoffs, van der Meij criteria (13,14) acknowledges the over-representation of OLP by the WHO 1978 criteria (15), thus, they introduced several exclusion criteria to objectify the final diagnosis of OLP. These included a mandatory bilateral clinical presentation and the presence of at least a minor reticular component for the clinical diagnosis of OLP. Histopathologically the presence of a subepithelial inflammatory band predominantly consisting of T lymphocytes and basal cell degeneration was considered diagnostic (typical) of OLP. In the absence of any one of these features, the clinical and/or histopathological diagnosis was considered not typical but only compatible, thus were excluded from the diagnosis of OLP (13,14). Although the criteria suggested by van der Meij et al. (13,14), is relatively more objective, the controversial part of the criteria is on a similar premise with Krutchkoff’s (11,12) wherein the presumption was that OLP does not have any inherent malignant potential. Thus, if a case is typical both clinically and histopathologically but exhibits features of epithelial dysplasia, then according to van der Meij et al. (13,14) the lesion is clinically typical but histopathologically only compatible and must be excluded from the diagnosis of OLP. The only difference between Kruthkoffs et al. (11,12) and van der Meij et al. (13,14) was that cases with OLP features and epithelial dysplasia were categorized as OLD by Krutchkoff et al. whereas such cases were categorized as OLL by van der Meij et al.
OLL with dysplasia
OLL was used by van der Meij et al. (13,14) to indicate a lesion whose clinicopathological features are compatible but not typical of OLP. This, in turn, could lead to an overestimation of the prevalence and malignant potential of OLL. A More specific diagnostic criterion for OLL requires a history of potential triggering agents (medications, a prosthetic material, toothpaste, etc.) and/or positive patch test against any one of the suspected triggering agents. Diagnosing OLL based on the allergic history and/or patch test and the clinicopathological lichenoid features would be relatively more objective. The clinical presentation of OLL is nonspecific which could be unilateral/bilateral presentation, erosive/ulcerative/atrophic/plaque-like or even reticular pattern. With respect to the histopathological features, OLL, unlike OLP, exhibits a non-specific pattern wherein the inflammation can be local or diffuse. The inflammatory infiltrate depends on the chronicity of the lesion, wherein usually, a mixture of acute and chronic inflammatory cells is noted (2-4).
Among the various entities diagnosed in the included studies (OLL with dysplasia, OLP with dysplasia and OLD), the primary pathology remains obscure. The diagnosis is either rendered based on the absolute absence of a feature (epithelial dysplasia as in Vender Meij criteria) or on the predominance of a feature (lichenoid or dysplasia). An additional area of controversy is the nature of the epithelial dysplasia noted in OLP and OLL. A hypothesis was that the dysplastic features seen in OLP do not represent true epithelial dysplasia but are reaction changes (cellular atypia) to the intense inflammation (4). Rock et al. (5) examined the true nature of dysplasia in OLP, by comparing the malignant potential of lesions diagnosed as OED and lesions diagnosed as oral lichenoid mucositis (OLP and OLL) with dysplasia. The study found no significant difference in the malignant potential between the two groups. Thus, they concluded that the dysplasia in lichenoid mucositis (OLL or OLP) carries malignant potential similar to that of OED. Based on the clinicopathological features and the malignant transformation noted in the cases of the included studies, it is clear that cases being diagnosed with lichenoid features can exhibit epithelial dysplasia and vice versa. Further irrespective of the primary pathology, these enigmatic entities (OLD, OLP with dysplasia, OLL with dysplasia) posses a malignant potential and must be classified as an OPMD. Despite providing insight into the malignant potential of oral mucosal lesions with both lichenoid and epithelial dysplastic features, the present review could not elicit the primary pathology in such lesions. Long-term prospective studies analyzing the natural progression of OED, OLP and OLL would aid in delineating the primary and secondary pathology, which in turn would aid in understanding their natural history.
Conclusions
Based on the clinicopathological features described in the included cases, an entity with OED can exhibit one or more lichenoid features and a lichenoid lesion can exhibit varying degrees of epithelial dysplasia. Thus, it would be objective to diagnose OLP, OLL based on the presence of characteristic features rather than the absence of epithelial dysplasia. From a clinical point of view, any case presenting with both lichenoid and epithelial dysplastic features irrespective of the primary pathology must be categorized as OPMD and treated accordingly. Stratification of malignant risk in such cases would depend on the grade of the epithelial dysplasia rather than the primary diagnosis.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: Provenance and Peer Review: This article was commissioned by the editorial office, Translational Cancer Research for the series “Oral Pre-cancer and Cancer”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2020.01.51). The series “Oral Pre-cancer and Cancer” was commissioned by the editorial office without any funding or sponsorship. SCS and KHA served as the unpaid Guest Editors of the series. SP served as an unpaid Guest Editor of the series and serves as an unpaid Editorial Board Member of Translational Cancer Research from Jul 2018 to Jun 2020. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Raj AT. Oral lichenoid dysplasia and exophytic oral verrucous hyperplasia: mythical entities of oral pathology. Oral Oncol 2017;70:75. [Crossref] [PubMed]
- Raj AT. Formulating a clinicopathological algorithm for oral lichenoid dysplasia and related lesions. Oral Oncol 2017;71:186-7. [Crossref] [PubMed]
- Raj AT, Patil S. Diagnostic flaws in oral lichen planus and related lesions. Oral Oncol 2017;74:190-1. [Crossref] [PubMed]
- Raj AT, Patil S, Gupta AA. True nature of mild epithelial dysplasia in oral lichenoid mucositis – Is it a reactionary change to the sub-epithelial inflammation or represents true malignant potential? A hypothesis. Med Hypotheses 2018;120:48. [Crossref] [PubMed]
- Rock LD, Laronde DM, Lin I, et al. Dysplasia Should Not Be Ignored in Lichenoid Mucositis. J Dent Res 2018;97:767-72. [Crossref] [PubMed]
- Zhang LW, Cheng X, Li YH, et al. High frequency of allelic loss in dysplastic lichenoid lesions. Lab Invest 2000;80:233-7. [Crossref] [PubMed]
- Patil S, Rao RS, Sanketh DS, et al. Lichenoid dysplasia revisited-evidence from a review of Indian archives. J Oral Pathol Med 2015;44:507-14. [Crossref] [PubMed]
- Shearston K, Fateh B, Tai S, et al. Oral lichenoid dysplasia and not oral lichen planus undergoes malignant transformation at high rates. J Oral Pathol Med 2019;48:538-45. [Crossref] [PubMed]
- Sanketh DS, Kumari K, Rao RS, et al. Expression of Ki-67, p53, α-SMA, and COX-2 in lichen planus and related lesions: A pilot study. J Oral Biol Craniofac Res 2019;9:230-5. [Crossref] [PubMed]
- Jaafari-Ashkavandi Z, Mardani M, Pardis S, et al. Oral Mucocutaneous Diseases: Clinicopathologic Analysis and Malignant Transformation. J Craniofac Surg 2011;22:949Y951.
- Krutchkoff DJ, Eisenberg E. Lichenoid dysplasia: a distinct histopathologic entity. Oral Surg Oral Med Oral Pathol 1985;60:308-15. [Crossref] [PubMed]
- Eisenberg E, Krutchkoff DJ. Lichenoid lesions of the oral mucosa. Diagnostic criteria and their importance in the alleged relationship to oral cancer. Oral Surg Oral Med Oral Pathol 1992;73:699-704. [Crossref] [PubMed]
- van der Meij EH, Schepman KP, van der Waal I. The possible premalignant character of oral lichen planus and oral lichenoid lesions: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;96:164-71. [Crossref] [PubMed]
- van der Meij EH, Schepman KP, Smeele LE, et al. A review of the recent literature regarding the malignant transformation of oral lichen planus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:307-10. [Crossref] [PubMed]
- WHO Collaborating Centre for Oral Precancerous Lesions. Definition of leukoplakia and related lesions: an aid to studies on oral precancer. Oral Surg Oral Med Oral Pathol 1978;46:518-39. [Crossref] [PubMed]