“Prostate management” under MRI-guidance: 7 years of improvements
Introduction
In 2017, 161,360 men were diagnosed for a prostate cancer (PCa) and 26,730 died because of PCa. Both diagnostic and treatment of PCa remains a challenge for future generation of urologist and radiologist to hope to improve our management. Active surveillance and focal therapy for good prognostic PCa may be therapeutic alternative to overtreatment.
On one hand, MRI is known and validate as the best radiological exam to explore the prostate (1-3). On the other hand, MR imaging-guided cryosurgery offers superior multi-planar ice-ball monitoring, accurate needle-guidance using MR-fluoroscopy sequences, and potential safety advantages over US-guidance (4,5).
It is much more labor intensive and expensive to perform MRI guidance and there is no evidence to show superiority yet. However, we believe that evaluation and treatment of an index lesion of the prostate should be managed from diagnosis to treatment with MRI-guidance.
The aim of this paper is to present the involvement of our technics of prostate biopsies and cryosurgery under MRI-guidance, to explain the gain in feasibility and reproducibility of the technic performed by urologist by handling MRI-environment and to show the active collaboration with interventional radiology.
In 2017, 161,360 men were diagnosed to have PCa in the USA out of which 26,730 died of this cancer. Diagnosis and treatment of PCa remains a challenge for future generations of urologists and radiologists. Active surveillance and focal therapy of patients with good prognosis PCa may be a therapeutic alternative to overtreatment.
MRI is known to be the best radiological investigation in evaluating the prostate (1-3). In addition, MRI-guided cryosurgery offers superior multi-planar ice-ball monitoring, accurate needle-guidance using MR-fluoroscopy sequences, and potential safety advantages over ultrasound guided procedures (4,5).
Although it is far more labor intensive as well as expensive to perform MRI guided procedures and there is no evidence of its superiority yet. However, we believe that evaluation and treatment of an index lesion of the prostate should be fully managed under MRI-guidance.
The focus of this paper is to present the involvement as well as the development of our techniques used in prostate biopsy and cryosurgery performed under MRI guidance. Moreover, it further explains the gain in feasibility and reproducibility of the technique performed by urologists, through MRI environment, and finally it emphasizes on the active collaboration with interventional radiology.
Methods
From 2009 to 2018, 62 patients necessitated MRI-guided prostate procedures. Patients were selected for this biopsy technique in case of transrectal ultrasound impossibility (rectal amputation, anal stenosis…), important discordance between pathology and MRI (especially in the anterior zone of the prostate). All the cryosurgeries were performed under MRI-guidance.
During this 9 years of experience, improvement of our technics to protect rectum and urethra, enhancement of precision and reproducibility was achieved. Procedures were performed both by urologist and radiologist under MRI-guidance in a dedicated hybrid-room.
A large-bore 1.5 T interventional MRI scanner (Magnetom-Espree and Magnetom-Aera; Siemens, Erlangen, Germany), pelvic phased-array coil, and MR-compatible cryoablation system (MR-Seednet, Galil-Medical, Yokneam, Israel), were used for MR-guidance. Multiplanar T2 BLADE (slice thickness =2.5 mm, TR =2,000 ms, TE =137 ms) and/or 3D T2 SPACE (slice thickness =2 mm, TR =1,000 ms, TE =126 ms) and/or T2 TrueFISP (slice thickness =5 mm, TR =4 ms, TE =2 ms) sequences were acquired for pre-procedural planning and thermoprotection, intra-procedural probe placement-confirmation and ice-ball monitoring, and assessment of post-procedural complications.
From 2009 to 2018, 62 patients required MRI-guided prostate procedures. The selection of patients was based on the fact that transrectal ultrasound guided procedures were technically impossible due to rectal amputation, anal stenosis…etc. and due to significant discordance between the pathology and MRI findings (especially in the anterior zone of the prostate). Hence, all cryosurgery prostate procedures were carried out under MRI-guidance.
Throughout 9 years of experience, our techniques to protect the rectum and the urethra has undergone quite a noticeable improvement; in return, the enhancement of accuracy and reproducibility were achieved. Procedures were performed by both urologists and radiologists under MRI-guidance in a dedicated hybrid-room.
A large-bore 1.5 T interventional MRI scanner (Magnetom-Espree and Magnetom-Aera; Siemens, Erlangen, Germany), pelvic phased-array coil, and MR-compatible cryoablation system (MR-Seednet, Galil-Medical, Yokneam, Israel), were used in MR-guidance. Multiplanar T2 BLADE (slice thickness =2.5 mm, TR =2,000 ms, TE =137 ms) and/or 3D T2 SPACE (slice thickness =2 mm, TR =1,000 ms, TE =126 ms) and/or T2 TrueFISP (slice thickness =5 mm, TR =4 ms, TE =2 ms) sequences were acquired for pre-procedural planning, thermoprotection, intra-procedural probe placement-confirmation, ice-ball monitoring, and assessment of post-procedural complications.
Results
All procedures, cryosurgery or prostate biopsy, are performed under general anesthesia. Antibiotic prophylaxis (fluoroquinolone) is administered intravenously prior to procedures.
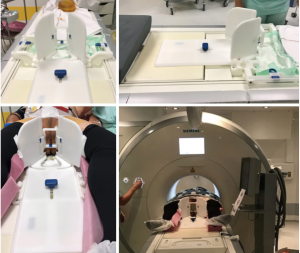
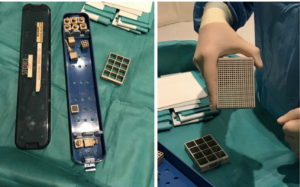
The main improvement between 2012 and 2016 was the construction of an MRI-compatible patient stand: Uni-Lift Prostate Intervention Device (NORAS GmbH, Höchberg, Deutschland) (Figure 1). This device allows a good access to the perineum with a scrotal elevation and strap fixation with respect to MRI-space restriction. Following the example of brachytherapy, an acrylic grid of 100 mm × 120 mm × 25mm is inserted in the patient stand and blocks perforated with 1.3 mm holes spaced 5 mm from each other are put in the grid (Figure 2).
This equipment make procedure easier by improving the precision, helping the needle navigation through the perineum and respect the distance between the cryoprobe during cryosurgery.
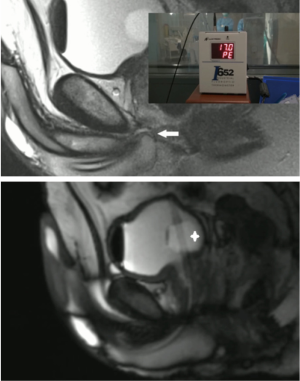
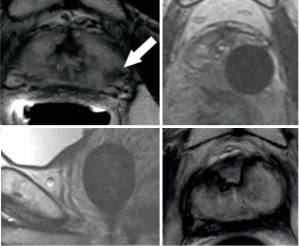
Thermoprotection of the rectal wall, used during cryosurgery, is achieved with a technic of hemo-dissection of the recto-prostatic space (6): we take 50 to 80 milliliters of patient’s blood from the humeral vein and we reinject it into the Denounvillier’s fascia under ultrasound guidance. MRI-control show that the hematoma moves the prostate away from the rectal wall (Figure 3).
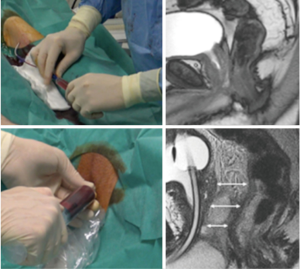
Thermoprotection of the urethra, used during cryosurgery, is achieved both by an irrigation of warm saline serum through a vesico-urethral catheter and by the monitoring of the sphincter’s temperatures (Figure 4). The thermocouple is inserted through the grid under MRI-guidance in the sphincter and thermometry is monitored to stop the procedure when the urethral temperature is below 15 °C.
All procedures, cryosurgeries and prostate biopsies, are performed under general anesthesia. Prophylactic antibiotic (fluoroquinolone) is administered intravenously prior to the intervention.
The major improvement in our technique between 2012 and 2016 was the construction of an MRI-compatible patient stand: Uni-Lift Prostate Intervention Device (NORAS GmbH, Höchberg, Deutschland) (Figure 1). This device permits a good access to the patient’s perineum with a scrotal elevation and strap fixation with respect to MRI-space restriction. Keeping in mind, the modality of brachytherapy, an acrylic grid of 100 mm × 120 mm × 25 mm is inserted into the patient stand and blocks are perforated with holes each sized 1.3 mm. These holes are 5 mm spaced from each other and are put in the grid (Figure 2).
The construction of this device makes the procedure technically easier, improves the accuracy and allows guidance of needle navigation throughout the perineum. Moreover, it respects the distance between the cryoprobes during cryosurgery.
Thermoprotection of the rectal wall during cryosurgery is achieved by a technique based on hemo-dissection of the recto-prostatic space (6): around 50 to 80 milliliters of patient’s blood is withdrawn from the humeral vein and is then injected into the Denounvillier’s fascia under ultrasound guidance. MRI-confirmed that creation of this hematoma moves away the prostate from the rectal wall (Figure 3).
In addition, thermoprotection of the urethra during cryosurgery is achieved by irrigation of the bladder with warm saline using a catheter placed in the bladder and by monitoring the urethral sphincter’s temperature (Figure 4). A thermocouple probe is inserted through the grid under MRI-guidance into the urethral sphincter. Urethral temperature is then monitored by a thermometry which discontinues the procedure when the urethral temperature is below 15 °C.
Finally, these improvements in the field of uro-radio-oncology may allowed in few years the development of focal treatments under MRI-guidance such as these focal cryotherapy of an apical lesion (Figure 5).
Discussion
Improving MRI guided techniques used for the management of PCa represent a challenge for patients and medical community.
This paper demonstrates that improvement and modification of the technique used long with experience in the field of MRI guided prostate procedures facilitated the performance of successful and reproducible procedures performed by both urologists and radiologists such as MRI guided focal cryosurgery of PCa.
By the end of the 20th century, the development of radiological guidance in surgical and medical has increased considerably.
Improvement of imaging studies along with technical procedures facilitated the mission of the radiologists, proved that new prospective of treatment were possible as well as it made access to hybrid-room more attractive to surgeons.
Given that the expertise of urologist in prostate anatomy and PCa management for decades, we believe that the involvement of urologists in the development of new diagnostic techniques and treatment is extremely essential. On the other hand, the experience of the radiologists in MRI semeiology, interventional procedure and focal therapy must be appreciated and recognized.
Compared to ultrasound-guidance, MRI-guidance is more accurate as well as it makes biopsy-needles or cryoprobes positioning easier (7-10). In addition, it allows a real-time monitoring of the iceball.
New softwares are currently able to detect needle/probe position through MRI-images and can also aid urologists or radiologists in navigation and planning (respect the distance between cryoprobes in covering a defined zone…).
In conclusion, these major improvements allow simplification and standardization of the technique used: using similar materials in the same position of different patients while performing biopsy or cryosurgery: keeping in mind MRI-guidance. The next step will be the use of robotic navigation in performing biopsy and cryosurgery of the prostate under MRI guidance.
Conclusions
Future development in “MRI-guided prostate-management” should be carried out by both urologists and radiologists and we hope that simplification of the technique along with urologists’ motivation could have an impact in improving focal therapy of PCa in the hybrid-room.
Treatment modalities of a new area, under-MRI guidance, will be emerging soon and may be utilized leading to good results, excellent accuracy and low side effects. Endo-urethral ultrasounds have been already studied along with MRI diagnosis machines to perform both focal and hemi-ablation treatments.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2020.03.44). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Every patient was informed before every procedure and gave his consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cornud F, Roumiguié M, Barry de Longchamps N, et al. Precision Matters in MR Imaging-targeted Prostate Biopsies: Evidence from a Prospective Study of Cognitive and Elastic Fusion Registration Transrectal Biopsies. Radiology 2018;287:534-42. [Crossref] [PubMed]
- Fütterer JJ, Briganti A, De Visschere P, et al. Can Clinically Significant Prostate Cancer Be Detected with Multiparametric Magnetic Resonance Imaging? A Systematic Review of the Literature. Eur Urol 2015;68:1045-53. [Crossref] [PubMed]
- Pokorny MR, de Rooij M, Duncan E, et al. Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent MR-guided biopsy in men without previous prostate biopsies. Eur Urol 2014;66:22-9. [Crossref] [PubMed]
- Cazzato RL, Garnon J, Shaygi B, et al. How to Perform a Routine Cryoablation Under MRI Guidance. Top Magn Reson Imaging TMRI 2018;27:33-8. [Crossref] [PubMed]
- Wegelin O, van Melick HHE, Hooft L, et al. Comparing Three Different Techniques for Magnetic Resonance Imaging-targeted Prostate Biopsies: A Systematic Review of In-bore versus Magnetic Resonance Imaging-transrectal Ultrasound fusion versus Cognitive Registration. Is There a Preferred Technique? Eur Urol 2017;71:517-31. [Crossref] [PubMed]
- Garnon J, Cazzato RL, Koch G, et al. Trans-rectal Ultrasound-Guided Autologous Blood Injection in the Interprostatorectal Space Prior to Percutaneous MRI-Guided Cryoablation of the Prostate. Cardiovasc Intervent Radiol 2018;41:653-9. [Crossref] [PubMed]
- Kinsman KA, White ML, Mynderse LA, et al. Whole-Gland Prostate Cancer Cryoablation with Magnetic Resonance Imaging Guidance: One-Year Follow-Up. Cardiovasc Intervent Radiol 2018;41:344-9. [Crossref] [PubMed]
- Radtke JP, Kuru TH, Boxler S, et al. Comparative analysis of transperineal template saturation prostate biopsy versus magnetic resonance imaging targeted biopsy with magnetic resonance imaging-ultrasound fusion guidance. J Urol 2015;193:87-94. [Crossref] [PubMed]
- Woodrum DA, Gorny KR, Greenwood B, et al. MRI-Guided Prostate Biopsy of Native and Recurrent Prostate Cancer. Semin Intervent Radiol 2016;33:196-205. [Crossref] [PubMed]
- Cornud F, Bomers J, Futterer JJ, et al. MR imaging-guided prostate interventional imaging: Ready for a clinical use? Diagn Interv Imaging 2018;99:743-53. [Crossref] [PubMed]