Transcolonic natural orifice specimen extraction for laparoscopic radical right hemicolectomy on ascending colon cancer: one case report and literature review
Introduction
Both laparoscopic-assisted and total laparoscopic resection have been well described for the surgical management of colorectal diseases (1,2). However, both approaches require about 5–10 cm abdominal incisions for specimen extraction and anastomosis of the bowel, which cause higher the risk of wound infection, incisional hernia and pain during the postoperative period (3-5). Natural orifice specimen extraction surgery (NOSES) is a new technique that combines traditional laparoscopy with specimen extraction through a natural orifice. Currently, specimens are delivered transcolonically, transrectally, transanally, or transvaginally (6). NOSES can reduce cutaneous trauma and incision-related morbidity (7,8). Until now, transanal extraction was the main option for rectosigmoid colectomy and left-sided colectomy, in addition to the transvaginal route, which is valid for all colorectal segments (7). However, no successful case about the ascending colon cancer with transcolonic specimen extraction was reported. In this paper, we describe the technical approach to laparoscopic radical resection of right colon cancer with transluminal colonoscopic specimen extraction that avoided minilaparotomy incisions and additional surgical incisions (i.e., transvaginal extraction). This may be an alternative technique for treatment of both male and female patients with right colon neoplasms.
Case presentation
Patient information and clinical findings
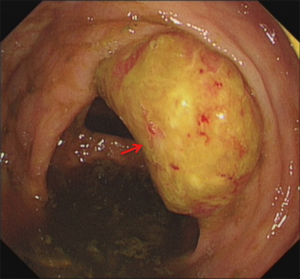
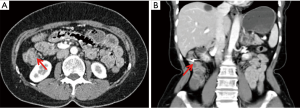
A 56-year-old female patient was admitted to hospital for finding a mass in ascending colon during physical examination. A 1.5 cm × 2.0 cm tumor was found by colonoscopy in the middle of ascending colon (Figure 1). The pathology of the biopsied specimen showed high-grade intraepithelial neoplasia and carcinogenesis. The CEA and CA199 was normal in blood tests. The plain and enhanced CT scan of the chest, abdomen and pelvic cavity showed that the local wall of the ascending colon was inconsistently thickened: the thicker part was 22 mm, and the corresponding enteric cavity was narrow. No abnormal lymph nodes and distant metastases were detected (Figure 2). Meanwhile the patient had no family history of colorectal cancer and was mentally stable.
Surgical techniques
The patient underwent transcolonic specimen extraction by colonoscope after laparoscopic radical resection of right colon cancer on June 11, 2019.
Preoperative preparation
We took the following bowel preparation for the patient undergoing NOSES: diet adjustment, semiliquid diet 3 days before surgery, liquid diet 2 days before surgery. From 6 pm to 8 pm the day before surgery, the bowel preparation was performed with 90 mL of sodium phosphate oral solution mixed well with 1.5 L of water and the patient need to drink the solution in 30 minutes.
Trocar location
Following general anesthesia and insertion of a urinary catheter, the patient was placed in the modified lithotomy position, with legs abducted and slightly flexed at the knees. The abdomen was insufflated by CO2 and a total of five abdominal trocars (one 12 mm, one 10 mm and three 5 mm trocars) were used.
Excision of tumor and extraction of specimen
Operative exploration showed no tumor metastasis nodules in the liver, gallbladder, stomach, spleen, small intestine and mesenteric root, greater omentum and peritoneum wall. We did not see the ascending colon tumor directly. The surgery was performed according to the principle of complete mesocolic excision (CME). The ileocolic vessel, the right colic vessel, and the right branch of middle colic vessel were separated and ligated with Hem-o-lock (Figure 3A,B). The mesocolon was dissected from the terminal ileum to the middle of the transverse colon. The assistant inserted a 60 mm linear stapler through the 12 mm trocar of the left upper abdominal. The terminal ileum and the middle of the transverse colon were transected with 60-mm linear stapler. The terminal ileum stump and the middle of the transverse colon stump were sterilized with iodine. The specimen was packed into a sterilized plastic bag (Figure 3C). Under the guidance of laparoscopy, colonoscope reached the closed transverse colon through the anus. After intestinal irrigation by colonoscopy, the stump of the colon was opened with ultrasound knife and sterilized with iodine (Figure 3D). The tip of the colonoscope was exposed, the internal foreign object forceps was outstretched, the specimen bag and resected bowel was clamped by foreign object forceps and the specimen bag was tied to the foreign object forceps with silk thread (Figure 3E). With the help of laparoscopic nondestructive forceps, the bag with specimen was moved to the transverse colon and removed through the left half of the transverse colon, splenic flexure of colon, descending colon, sigmoid colon, rectum and anus (Figure 3F). The opened transverse colon was closed with 60 mm linear stapler.
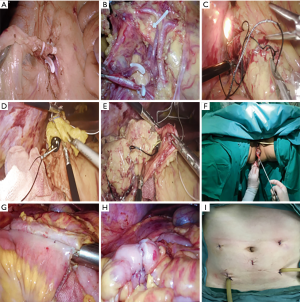
Digestive tract reconstruction
The transverse colon was straightened and the terminal ileum was pulled to the upper abdomen making it parallel to the transverse colon. The corner of the terminal ileum was cut open with an ultrasonic knife along the anastomotic nail, and the opened bowel was sterilized with iodine. The same operational procedure was repeated with the transverse colon. The assistant inserted a 60 mm linear stapler through the 12 mm trocar of the left upper abdominal. The terminal ileum and the transverse colon were functional side to side anastomosed with a 60 mm stapler (Figure 3G). The anastomotic seromuscular layers were enforced with a suture line to reduce the anastomotic tension (Figure 3H). Two drainage tubes were placed in the abdominal cavity (Figure 3I).
Surgical and pathological outcome
The specimen was successfully extracted via the colon through the rectum and anal canal, only leaving five trocars incisions on the abdomen. The operating time was 246 minutes and intraoperative blood loss was 20 mL. The length of resected specimen was 50 cm with a 1.8×1.6×0.5 cm3 tumor at the ascending colon (Figure 4). Oral intake and out-of-bed activity were tolerated on postoperative day 1. The peritoneal drainage tubes were all removed 3 days after surgery. The patient was discharged 6 days after the operation without postoperative complications. No adverse and unanticipated events throughout the patient’s treatment. Postoperative pathological examination revealed moderately differentiated adenocarcinoma invading the deep muscle layer. The tumor staging was pT2N0M0, without nerve and vessel invasion. No tumor cells were detected in the pelvic lavage fluid, and the resection margins were free of tumor. None of the 38 lymph nodes resected contains metastatic cancer. The immunohistochemical staining (Figure 5) was MSH2(25D12)(+), MSH6(+), MLH1(+) and PMS2(+). The details of historical and current treatment were showed in Table 1.
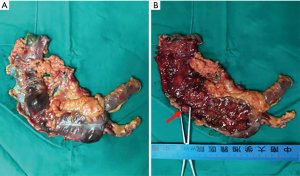
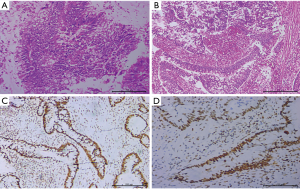
Table 1
| Date | Preoperative treatment process | Postoperative treatment |
|---|---|---|
| May 26 | Colon mass was found by colonoscopy | |
| June 5 | Ascending colon cancer | |
| June 5–10 | Hospitalization and preoperative examination | |
| June 10: 6–8 pm | Bowel preparation | |
| June 11 | Operation: Transcolonic natural orifice specimen extraction for laparoscopic radical right hemicolectomy | |
| June 12 | Oral intake and out-of-bed activity | |
| June 14 | Two peritoneal drainage tubes were removed | |
| June 17 | Discharge |
Discussion
Early colonic cancer lesions can be removed by endoscopy with advantage of safety, noninvasion and good prognosis (9). In this case, tumor has invaded the muscle layer of colon. Therefore, we thought endoscopic resection was risky. We then proposed a minimal invasive laparoscopic surgery for this patient. Due to the complicated anatomy adjacent to the right hemicolon, a large longitudinal incision is often needed in radical colectomy, which leads to severe postoperative pain, mental stress and long time for recovery. Therefore, we planned to do a more minimal invasive radical right hemicolectomy than the standard laparoscopic operation to reduce incision-related complications.
NOSES combines the minimal invasive idea of Natural Orifice Translumenal Endoscopic Surgery (NOTES) with the operating advantage of laparoscopic surgery (10,11). NOSES without a long abdominal incision contributes to not only better cosmetic results but also less postoperative pain (12), which accelerates patients’ recovery and early ambulation. Moreover, NOSES reduces the rate of surgical site infection and incisional hernia (13,14). The two natural orifices, the vagina and the anus (colon), are good choices for specimen extraction in colorectal resection surgery (7,8). Compared to anus, vagina has a greater extensibility. So for bulky specimen, extracting it from the posterior vaginal fornix incision would be our priority, which is especially suitable for right hemicolectomy (6,15,16). However, due to the anatomy of the pouch of Douglas, transvaginal specimen extraction is more complicated than transanal specimen extraction. Therefore, transvaginal extraction needs more effective extraction devices to protect the adjacent organs, such as the sigmoid colon and rectum. Additionally, transvaginal extraction of specimen has its limitations. This method is not suitable for male patients, teenagers, virgins and women of childbearing age. Still, the surgical incision in the vagina is difficult for most patients to accept, even if the patient has already gone through menopause. Transcolonic and then transanal extraction of specimen is more aligned with physiological and anatomical structure. In this case, the patient’s preoperative assessment showed that the mass was small, so we preferred the transcolonic extraction of specimen to avoid additional wounds. Radical resection of right colon cancer with transcolonic extraction of specimen requires crossing the two natural barriers, which are splenic flexure of colon and the sigmoid flexure. We should select a suitable patient because these barriers make the extraction process more complicated. Kayaalp et al. (8) showed that the extraction failed in these cases where the width of the specimen was greater than 12 cm. Further, Eshuis et al. (17) advocated that extraction of specimens through the colon should have a maximum diameter of 5 cm in patients without inflammatory masses. The research showed that transcolonic removal was successful in eight of ten patients, and the two cases failed because of the oversized masses. Therefore, we considered the specimen size as main influence factor in intracolonic extraction of specimens. In our case, the patient was diagnosed with ascending colon cancer before the operation. The electronic colonoscopy showed largest diameter of the mass was less than 2 cm, and the patient’s body mass index (BMI) was 20.54 kg/m2. Intraoperative evaluation of the mesocolon showed no hypertrophy. Therefore, we considered transcolonic extraction of the specimen as feasible and safe. During operation, we must follow the principles of aseptic and nontumor extraction, which are key to evaluate the success of NOSES. Here are few tips: The intestine remains open in the abdominal cavity when extracting the specimen and reconstructing the digestive tract under laparoscopy, so the intestinal tract should be fully prepared before operation; Iodophor gauze is used to disinfect the closed-end and opened corner of bowel for the functional side-to-side anastomosis; Extraction of specimen requires a tightened sterile protector in case tumor cells fall off the abdominal cavity; The specimen with a sterile protector should be straightened by laparoscopy forceps, and be pulled out slowly by endoscopy foreign object forceps; In the process of transcolonic extraction of specimens, we should be very careful to avoid damaging the aseptic protective sleeve and specimen. Yagci et al. (18) and Kayaalp et al. (8) believed that division of the colon mesenteric during operation can make specimen extraction through a natural orifice easier. However, for colon cancer, specimen integrity should be protected to reduce the possibility that tumors may be planted in the abdominal cavity.
Although there has been reported the transcolonic extraction by colonoscopy in four studies (Table 2), we performed the first successful laparoscopic radical resection of right colon cancer with transcolonic specimen extraction using colonoscopy and shared our experience from this case. As previously mentioned, Eshuis et al. (17) only studied ileocolic specimens. Similarly, Takayama et al. (20) described an ileocolic resection for a polyp. Saad et al. (19) reported a case of transverse colon resection for a polyp through the transcolonic extraction. Kayaalp et al. (8) reported three cases with Crohn’s, carcinoid, and cecal adenocarcinoma. The case with cecal adenocarcinoma failed because the tumor diameter was too large. These cases above show that transcolonic specimen extraction by colonoscopy for radical resection of right colon cancer is feasible in well selected patients. However, transcolonic NOSES is highly dependent on the patient’s clinical condition and is exclusive for small tumors. In addition, experienced laparoscopic operational skills, tacit surgical cooperation between laparoscopic physicians and endoscopic physicians, adequate preoperative bowel preparation, and aseptic and nontumor intraoperative techniques are strictly required.
Table 2
| Variables | Our patient | Cuneyt Kayaalp (8), median [range] | Eshuis (17), median [range] | Saad (19) | Takayama (20) |
|---|---|---|---|---|---|
| Number of patients | 1 | 3 | 10 | 1 | 1 |
| Age (yr) | 56 | 48 [20–68] | 31 [19–61] | 70 | 71 |
| Gender | F | 1 M, 2 F | 3 M, 7 F | F | M |
| BMI (kg/m2) | 20.5 | 23 [20–27] | 23.7 [18–31] | NA | NA |
| Operating time (min) | 246 | 336.7 [210–500] | 208 [157–327] | NA | 240 |
| Blood loss (mL) | 20 | 143.3 [10–400] | NA | NA | 28 |
| Specimen length (cm) | 50 | 19 [13–27] | 25.5 [16–64] | NA | 8 |
| Specimen width (cm) | 10 | 8.67 [6–12] | >7 cm (n=2); ≤7 cm (n=8) | NA | NA |
| Failure | No | Yes 1, no 2 | Yes 2, no 8 | No | No |
| Complications | No | No | Yes 3, no 7 | No | No |
| Resection location | RRHC | Ileocolic 1, RHC 2 | Ileocolic | Transverse | Ileocolic |
| Pathology | Cancer | Crohn’s 1, carcinoid 1, cancer 1 (failure) | Crohn’s | Adenoma | Adenoma |
| Oral diet (d) | 1 | 2.67 [2–3] | NA | NA | 1 |
| Hospital stay (d) | 6 | 4.67 [4–5] | 5 [2–10] | 5 | 4 |
NA, not available; F, female; M, male; RRHC, radical right hemicolectomy; BMI, body mass index; RHC, right hemicolectomy.
Conclusions
Our study supports the idea that transcolonic NOSES for laparoscopic radical right hemicolectomy on ascending colon cancer is feasible and safe and achieves satisfactory clinical outcomes without noticeable scars in well-selected patients. At the initial stage, it is only suitable to be carried out in well-equipped and large-scale research hospitals.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2020.04.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Franklin ME Jr, Ramos R, Rosenthal D, et al. Laparoscopic colonic procedures. World J Surg 1993;17:51-6. [Crossref] [PubMed]
- Grams J, Tong W, Greenstein AJ, et al. Comparison of intracorporeal versus extracorporeal anastomosis in laparoscopic-assisted hemicolectomy. Surg Endosc 2010;24:1886-91. [Crossref] [PubMed]
- Brennan TJ, Zahn PK, Pogatzki-Zahn EM. Mechanisms of incisional pain. Anesthesiol Clin North Am 2005;23:1-20. [Crossref] [PubMed]
- Hussain A, Mahmood H, Singhal T, et al. Long-term study of port-site incisional hernia after laparoscopic procedures. JSLS 2009;13:346-9. [PubMed]
- Winslow ER, Fleshman JW, Birnbaum EH, et al. Wound complications of laparoscopic vs open colectomy. Surg Endosc 2002;16:1420-5. [Crossref] [PubMed]
- Wolthuis AM, de Buck van Overstraeten A, D'Hoore A. Laparoscopic natural orifice specimen extraction-colectomy: a systematic review. World J Gastroenterol 2014;20:12981-92. [Crossref] [PubMed]
- Franklin ME Jr, Liang S, Russek K. Natural orifice specimen extraction in laparoscopic colorectal surgery: transanal and transvaginal approaches. Tech Coloproctol 2013;17:S63-7. [Crossref] [PubMed]
- Kayaalp C, Kutluturk K, Yagci MA, et al. Laparoscopic right-sided colonic resection with transluminal colonoscopic specimen extraction. World J Gastrointest Endosc 2015;7:1078-82. [Crossref] [PubMed]
- Yamamoto H. Endoscopic submucosal dissection of early cancers and large flat adenomas. Clin Gastroenterol Hepatol 2005;3:S74-6. [Crossref] [PubMed]
- Pascual M, Salvans S, Pera M. Laparoscopic colorectal surgery: Current status and implementation of the latest technological innovations. World J Gastroenterol 2016;22:704-17. [Crossref] [PubMed]
- Leung AL, Cheung HY, Li MK. Advances in laparoscopic colorectal surgery: a review on NOTES and transanal extraction of specimen. Asian J Endosc Surg 2014;7:11-6. [Crossref] [PubMed]
- Wolthuis AM, Fieuws S, Van Den Bosch A, et al. Randomized clinical trial of laparoscopic colectomy with or without natural-orifice specimen extraction. Br J Surg 2015;102:630-7. [Crossref] [PubMed]
- Franklin ME Jr, Liang S, Russek K. Integration of transanal specimen extraction into laparoscopic anterior resection with total mesorectal excision for rectal cancer: a consecutive series of 179 patients. Surg Endosc 2013;27:127-32. [Crossref] [PubMed]
- Wolthuis AM, Penninckx F, D'Hoore A. Laparoscopic sigmoid resection with transrectal specimen extraction has a good short-term outcome. Surg Endosc 2011;25:2034-8. [Crossref] [PubMed]
- Franklin ME Jr, Kelley H, Kelley M, et al. Transvaginal extraction of the specimen after total laparoscopic right hemicolectomy with intracorporeal anastomosis. Surg Laparosc Endosc Percutan Tech 2008;18:294-8. [Crossref] [PubMed]
- Park JS, Choi GS, Lim KH, et al. Clinical outcome of laparoscopic right hemicolectomy with transvaginal resection, anastomosis, and retrieval of specimen. Dis Colon Rectum 2010;53:1473-9. [Crossref] [PubMed]
- Eshuis EJ, Voermans RP, Stokkers PC, et al. Laparoscopic resection with transcolonic specimen extraction for ileocaecal Crohn's disease. Br J Surg 2010;97:569-74. [Crossref] [PubMed]
- Yagci MA, Kayaalp C, Novruzov NH. Intracorporeal mesenteric division of the colon can make the specimen more suitable for natural orifice extraction. J Laparoendosc Adv Surg Tech A 2014;24:484-6. [Crossref] [PubMed]
- Saad S, Schmischke D, Martin C, et al. Hybrid laparoscopic colectomy with transluminal colonoscopic specimen extraction--a step toward natural orifice surgery. Endoscopy 2010;42:E346-7. [Crossref] [PubMed]
- Takayama S, Hara M, Sato M, et al. Hybrid natural orifice transluminal endoscopic surgery for ileocecal resection. World J Gastrointest Surg 2012;4:41-4. [Crossref] [PubMed]