Uniportal video-assisted thoracoscopic surgery for lung neoplasms with tracheal bronchus: a case report
Introduction
Tracheal bronchus (TB) is an anomaly where a bronchus directly arises from the trachea, with an incidence of 0.1–5% (1-3). Most patients with TB are often asymptomatic. Some may suffer recurrent pneumonia, persistent cough, hemoptysis, and acute respiratory distress. Due to the low incidence of TB, there were even less reports about it with lung cancer. For TB may lead to intubation complications (4), it is important for thoracic surgeon and anesthesiologist to evaluation the existed of TB before surgery. Here, we report the first case where a patient with TB underwent uniportal video-assisted thoracoscopic surgery (VATS) for lung neoplasms. We present the following case in accordance with the CARE Guideline (5).
Case presentation
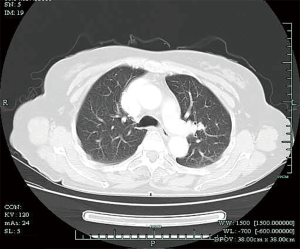
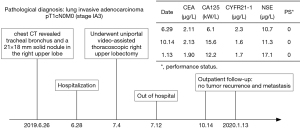
A 63-year-old woman came to our hospital complaint about an abnormal shadow on chest computed tomography (CT) during a routine examination, without any clinical symptoms. She did not smoke and denied family and medical history. CT showed a 21 mm × 18 mm solid mass in the right upper lobe S1 (Figure 1), which could can be significantly enhanced upon contrast-CT. That strongly raised a suspicion for primary lung adenocarcinoma. CT also revealed an infrequent variation where a bronchus arose from the trachea and running directly toward to the right upper lobe (Figure 2). For the suspicion of adenocarcinoma, the patient underwent an uniportal video-assisted thoracic surgery on 4th July, 2019.
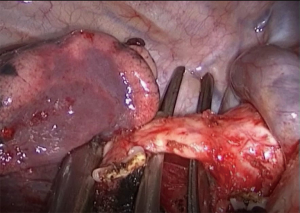
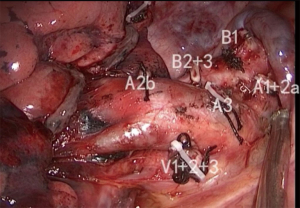
During the surgery (Video 1), we found two bronchi which were located behind the hilum and running toward the right upper lobe. And one of the two branched directly from the trachea, which was confirmed to be TB (Figure 3). Meanwhile, a pulmonary vein (V1+2+3) running towards the root of pulmonary artery and returning the left atrium. No lobulation was observed between lobes. During the operation, first, we exposed the pulmonary artery through the mediastinal pleura by dissection. Subsequently, artery (A) 1+2b, TB, V1+2+3, A3, B2+3, and A2a were transected in this order (Figure 4). Mediastinal lymph nodes including groups 2, 3, 4, 7 were resected, and we use an endostapler to transect the TB and upper lobe bronchus separately. Frozen-section pathology was adenocarcinoma. The uniportal video-assisted thoracoscopic right upper lobectomy was success. And the patient recovered uneventfully after surgery. Specifically, the pathological diagnosis supported the diagnosis of adenocarcinoma, pT1cN0M0 (stage IA3). Chest X-ray and blood test were performed the first day after surgery and the day before the patient out of hospital to exclude complication like hemorrhage or pulmonary atelectasis. The patient doesn’t need chemotherapy after surgery and comes to our outpatient for follow-up. The patient did not complaint noticeable discomfort and there were no obvious signs of tumor recurrence and metastasis at the patient’s 3 and 6 months follow-up by doing blood test, ultrasound of abdominal and adrenal, chest CT. Performance status and the changes of the patient’s tumor indexes were shown in the timeline (Figure 5). Now the patient is still being followed up outpatient.
Discussion
In 1785, Sandifort first used TB to describe a right upper lobe bronchus that directly originated from the trachea. Later, some scholars extended this concept. Currently an unnormal bronchus who directly arises from the trachea or main bronchus and runs into the right upper lobe is defined as TB. Since a TB is normal in some ruminant animals, bronchus suis, or “pig bronchus,” is used as an alternate name (6). McLaughlin et al. reported an incidence of 2% (1). Barat et al. reported that its incidence ranges between 0.1% and 5% (2,3).
Most patients with TB are often asymptomatic. Some of the patients got the TB detected upon CT or bronchoscopy unintentionally. However, it can cause recurrent pneumonia, persistent cough, hemoptysis, and acute respiratory distress, especially in children. Meanwhile, TB is also related with vessel variations and other congenital malformation (7,8). TB may also lead to intubation complications (9,10), so anesthetist should know about TB in case the occur of atelectasis, hypoxemia when performing endotracheal intubation. Some studies have reported TB during thoracotomy (11,12).
Partially due to the low incidence of TB, there were only a lower number of reports about lung cancer with TB. With the development of thoracoscopy, currently thoracic surgery can be performed with the assistance of video thoracoscope. Yurugi et al. ever reported a case about thoracoscopic right upper lobectomy with TB (13). Here, we report a case of uniportal VATS right upper lobectomy for lung neoplasms with TB, which, to our knowledge, is the first one of its kind. Adhesions and lymphadenopathy which are caused by repeated infections are common in patients with TB. Although the patient in our case didn’t have the history of repeated pneumonia, prompt actions including conversion from VATS to thoracotomy would have been taken if any difficulties or dangerous situations encountered during the surgery.
Although we identified the incidental finding of this patients before surgery, it did not show in the report of chest CT scan. Further examination like three-dimensional reconstruction CT or fiberoptic bronchoscopy can be done to figure out it. Due to the risk of anesthesia for TB patients, thoracic surgeon and anesthesiologist should discuss intubation risks, patient’s condition and operation plan in depth before surgery. If necessary, fiberoptic bronchoscopy should be performed before anesthesia to evaluation the airway of patient to reduce the risks of airway injury.
By careful operation, uniportal VATS right upper lobectomy was successfully performed in this case. In the surgical procedure, lymph nodes were feasible at the root of the TB around hilum, and the adhesive lymph nodes was successfully dissected. And the patient recovered uneventful after this surgery. By using uniportal VATS, the invasive harm to the patient is minimal, and the recovery after surgery is enhanced.
Conclusions
TB can be recognized by chest CT scan, but it is better to complete three-dimensional reconstruction CT or fiberoptic bronchoscopy to identified TB before surgery. Through detailed preoperative assessment and cooperation of thoracic surgeon and anesthesiologist, uniportal VATS right upper lobectomy is safe and can be successful performed. It can expedite the recovery of patients. In case of the pulmonary vessel variations and other congenital malformation, we’d better take the advantage of CT bronchography or 3D-CT angiography before surgery.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr-20-908). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent for the publication of the report, and the accompanying images, was provided by the patient. The submission version of the report was read by her, and the report’s content was confirmed as being correct to the best of her knowledge. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- McLaughlin FJ, Strieder DJ, Harris GB, et al. Tracheal bronchus: association with respiratory morbidity in childhood. J Pediatr 1985;106:751-5. [Crossref] [PubMed]
- Barat M, Konrad HR. Tracheal bronchus. Am J Otolaryngol 1987;8:118-22. [Crossref] [PubMed]
- Agarwal S, Banks MA, Dalela S, et al. Incidental finding of tracheal bronchus complicating the anesthetic management of a left video-assisted thoracoscopic procedure. J Anaesthesiol Clin Pharmacol 2016;32:106-8. [Crossref] [PubMed]
- Conacher ID. Implications of a tracheal bronchus for adult anaesthetic practice. Br J Anaesth 2000;85:317-20. [Crossref] [PubMed]
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol 2017;89:218-35. [Crossref] [PubMed]
- Doolittle AM, Mair EA. Tracheal bronchus: classification, endoscopic analysis, and airway management. Otolaryngol Head Neck Surg 2002;126:240-3. [Crossref] [PubMed]
- Samara OA, Al-Ryalat NT, Ghafel AN, et al. Incidental finding of an aberrant left pulmonary artery, an aberrant right subclavian artery, and a tracheal bronchus in an adult woman with a meningioma and a history of medulloblastoma. Surg Radiol Anat 2020;42:397-400. [Crossref] [PubMed]
- Chabowski M, Szymanska-Chabowska A, Szolkowska M, et al. Mediastinal lymphangioma in an adult with a tracheal bronchus. Srpski Arhiv za Celokupno Lekarstvo 2017;145:400-2. [Crossref]
- Ming Z, Lin Z. Evaluation of tracheal bronchus in Chinese children using multidetector CT. Pediatr Radiol 2007;37:1230-4. [Crossref] [PubMed]
- Chassagnon G, Morel B, Carpentier E, et al. Tracheobronchial Branching Abnormalities: Lobe-based Classification Scheme-Erratum. Radiographics 2016;36:1258. [Crossref] [PubMed]
- García-Hernández C, Carvajal Figueroa L, Celorio Alcántara Á, et al. Thoracoscopic lobectomy for the treatment of tracheal bronchus. A pediatric case report. Cir Cir 2017;85:557-61. [PubMed]
- Moon YJ, Kim SH, Park SW, et al. The implications of a tracheal bronchus on one-lung ventilation and fibreoptic bronchoscopy in a patient undergoing thoracic surgery: a case report. Can J Anaesth 2015;62:399-402. [Crossref] [PubMed]
- Yurugi Y, Nakamura H, Taniguchi Y, et al. Case of thoracoscopic right upper lobectomy for lung cancer with tracheal bronchus and a pulmonary vein variation. Asian J Endosc Surg 2012;5:93-5. [Crossref] [PubMed]