
Comparison of positioning accuracy of different registration methods and dosimetric analysis of adaptive radiotherapy for breast cancer after breast conserving surgery
Introduction
Breast cancer is a malignant tumor that seriously endangers the health of women. The present goal of breast cancer operation is to shrink the scope of resection. The treatment strategy of early invasive breast cancer has gradually changed from the previous radical mastectomy and modified radical mastectomy to breast preservation. The results of several randomized group studies have confirmed that breast-conserving surgery and modified radical mastectomy have a similar local control rate and long-term survival rate, and have better cosmetic effects in patients with early breast cancer. Therefore, it has become the first choice for an increasing number of patients with early breast cancer.
The mode of whole breast radiotherapy after breast conserving surgery for breast cancer is increasing day by day. Intensity modulated radiotherapy (IMRT) has become a typical and popular mode in recent years (1-4). However, in the process of IMRT, the displacement of the target is a key factor to be considered, which can affect the dose volume parameters of the whole breast IMRT to a certain extent, and increase the boundary of the tumor target. Furthermore, this can easily increase the radiation dose for normal tissues. As a form of IMRT, adaptive radiotherapy (ART) has been used to evaluate the changes in anatomical structure, or changes in tumor retraction, morphology and location during treatment. The dosimetry of the ART treatment plan was compared with that of the original IMRT plan. The aim of the present study was to guide the redesign of the subsequent grading plan, and determine whether ART has advantages in increasing the target dose and reducing the dose of the protector tube. Image-guided radiotherapy (IGRT) has been widely used in postoperative radiotherapy for breast cancer. IGRT is a new tumor radiotherapy technique for target localization and patient positioning through a series of imaging systems. Accurate positioning is an important guarantee for accurate radiotherapy, and a positioning error can cause changes in the target dose. In view of this situation, cone-beam computed tomography (CBCT) technology has gradually become popularized in radiotherapy. Under the guidance of this technique, the positioning error of tumor patients can be effectively corrected, in order to reduce the proportion of the extended boundary, which is of great significance in radiotherapy (5-8). The aim of the present study was to analyze the influence of different registration methods on the positioning accuracy and dosimetry of ART under the premise of automatic gray registration and under the guidance of CBCT, which is summarized, as follows.
Methods
Subject information
In the present study, 30 patients with breast cancer, who were treated in the Affiliated Cancer Hospital of Xinjiang Medical University from October 2017 to April 2018, were divided into three groups, according to the random number table (n=10, each group): automatic grayscale registration group (group A), automatic bony marker registration group (group B), and automatic grayscale registration group combined with manual bony marker registration group (group C). The standard registration box of the X-ray volumetric imaging (XVI) system was selected for the registration range of all patients. In addition, 13 patients with left breast cancer after breast conserving surgery were selected. Automatic bone registration was first performed. Then, deformation registration was used (group D).
Inclusion criteria: patients with stage I-II breast cancer after breast conserving surgery and required accurate whole breast radiotherapy after breast conserving surgery; patients whose primary tumors were breast cancers, and the mode of operation was total breast IMRT; patients who received breast conserving chemotherapy. These patients had no ventilatory dysfunction, and no chronic cardiopulmonary disease. Furthermore, their pulmonary function was basically normal, and the upper limb lift and abduction function of all patients were good, which could meet the requirements of arm support and grip.
All subjects provided a signed informed consent form, and were approved by the Hospital Ethics Committee. The age of these subjects ranged within 25–82 years old, with a median age of 53 years old. There were six patients with left breast cancer and four patients with right breast cancer in group A, four patients with left breast cancer and six patients with right breast cancer in group B, and six patients with left breast cancer and four patients with right breast cancer in group C. There was no statistical significance in the general data analysis.
Positioning methods and equipment
The patient initially lied on their back on the breast bracket and raised their upper limb of the affected side, showing an abduction shape. This ensures that after the ipsilateral breast is fully exposed, the three-dimensional laser line is collimated to the middle line and the left and right sides of the patient’s body, and the positioning reference lead point is placed at the same time. The bracket values of patients with breast bracket location were recorded. Then, the thermoplastic film was soaked in hot water at 70 °C until the mask was transparent, a towel was used to suck out the water droplets, and this was quickly and gently pulled into the head, neck and chest of patients in the three groups. At the same time, the breast was completely wrapped in the lower boundary until the thermoplastic film cooled and formed.
Next, using the large aperture computed tomography (CT) as the auxiliary tool, the spiral scanning operation was completed, the layer thickness was set to 5 mm, and the image resolution was set to 1,024×1,024. Then, the large aperture screw was used as the auxiliary tool to complete the spiral scanning operation. After the calm breathing state was scanned according to the target area, the image data was transmitted to the Eclipse 11.0 treatment planning system (Varian) through a computer network. Then, the Deputy Chief Physician drew the target area, and the Chief Physician modified and confirmed the target area.
IMRT plan design
The 6MV-X line of the Eclipse 11.0 system was selected, and a 95% isodose line was wrapped around the planning target volume (PTV), in order to design the IMRT plan as far as possible and make the treatment plan center consistent with the location center as far as possible. Each organ should meet the following conditions: heart V25 <10%, V30 <5%; bilateral lung V20 <14%, affected lung V30 <10%, V20 <25%, PTV D95 =50 Gy, V53.50 <10.00%, V55 <5.00%, contralateral breast maximum dose received by 1% of CTV/PTV (Dmax) <8 Gy, and the mean dose received by 1% of CTV/PTV (Dmean) <1 Gy. These patients were treated with whole breast IMRT for 25 times, with a dose of DT 50 Gy at 2 Gy per day, for five times a week.
Image registration and ART plan design
The treatment plan was transferred to the Varian Clinac Trilogy RapidArc Accelerator 4 DTC OBI workstation. Before the implementation of the radiotherapy plan, each patient entered the computer room for positioning verification, which was conducted by two radiotherapy therapists, a clinician and a physicist. According to relevant standards, the positioning error was within the allowable ±5 mm, and the CBCT images were collected. The reconstructed CBCT image and planned CT image were registered by means of automatic grayscale registration, automatic bone marker registration, automatic grayscale registration, and manual bone marker registration. Before the first radiotherapy, the images were registered by means of automatic grayscale registration, automatic bony marker registration, automatic grayscale registration, and manual bony marker registration. Then, the verification images were taken once a week for comparative verification, with a total of 150 groups of data. The displacement values of X (left and right direction), Y (head and foot direction), and Z (ventral back direction) were recorded.
Under the premise of automatic bone registration and deformation registration, the planned CT images and CBCT images were registered, and the tissue contours were transmitted to the Eclipse 11.0 treatment planning system (Varian). Then, the fusion image was transferred to the planned CT image, the CBCT plan was compared with the CT plan angle, field shape and number of machine hop, and the fractionation radiotherapy plan was obtained. The prescription dose for the PTV reached 10 Gy for 95% PTV each time. A total dose plan, that is, the ART cumulative dose plan, was obtained using the plan sum function of the Eclipse 11.0 planning system for the CBCT plan.
Observation indicators
The positioning errors in the X, Y and Z directions of patients in groups A, B and C were compared: the percentages of the Dmax, the minimum dose received by 1% of CTV/PTV (Dmin), Dmean, D90 and D95 in group D (V90, V95 and V100); the PTV homogeneity index (HI) and conformity index (CI). The evaluation parameters of endangered organs included the V5, V10, V20 and V30 of the affected lung and bilateral lungs, the V5, V10, V20 and V30 of the heart, the V5, V10, V20 and V30 of the mean dose, the Dmean, V5, V10 and Dmax of the contralateral mammary gland, and the HI of the PTV in the evaluated target area. HI = D5/D95, target fitness index (CI), CI = (Vt,ref/Vt) × (Vt,ref/Vref), in which Vt is the target volume, Vt,ref is the target volume of the reference isodose bread, and Vref is the volume of all areas enclosed by the reference isodose surface.
Statistical analysis
The SPSS 20.0 software was used for the analysis. Data were presented as mean ± standard deviation (SD). T-test was performed for normally distributed data, while Wilcoxon signed rank test was performed for non-normally distributed data. P<0.05 (9,10) was considered statistically significant.
Results
Comparison of the mean and standard deviations of positioning errors in the X, Y and Z directions of the three groups
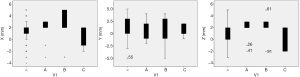
The mean and standard deviation of positioning error in the X, Y and Z directions for group A was 1.60±1.55, 1.24±1.86 and 1.08±1.92 mm, respectively. The mean and standard deviation of positioning error in the X, Y and Z directions for group B was 2.12±2.18, 1.88±2.78 and 1.64±2.39 mm, respectively. The mean and standard deviation of positioning error in the X, Y and Z directions for group C was 0.50±1.50, 0.52±1.18 and 0.38±1.51 mm, respectively. The details are presented in Table 1. Figure 1A,B,C present box diagrams of the positioning errors in the X, Y and Z directions in groups A, B and C, respectively.
Table 1
| Groups | Cases | Displacement in X-direction | Displacement in Y-direction | Displacement in Z-direction |
|---|---|---|---|---|
| Group A | 10 | 1.60±1.55 | 1.24±1.86 | 1.08±1.92 |
| Group B | 10 | 2.12±2.18 | 1.88±2.78 | 1.64±2.39 |
| Group C | 10 | 0.50±1.50 | 0.52±1.18 | 0.38±1.51 |
Statistical analysis of positioning errors in the X, Y and Z directions in the three groups of patients
There was a significant difference between group A and group B in the X direction (Z=−2.100, P=0.036), but there was no significant difference in the Y and Z direction (Z=−1.775, P=0.076; Z=−1.734, P=0.083). The details are presented in Table 2. There was a significant difference between group A and group C in the X and Y direction (Z=−3.306, P=0.001; Z=−2.339, P=0.019). In the X and Y direction, there was a significant difference in placement error between group B and group C (Z=−3.777, P<0.001; Z=−3.016, P=0.003), and there was significant difference in placement error between group B and group C (Z=−2.789, P=0.005).
Table 2
| Groups | X direction | Y direction | Z direction | |||||
|---|---|---|---|---|---|---|---|---|
| Z value | P value | Z value | P value | Z value | P value | |||
| Group A and Group B | −2.100 | 0.036 | −1.775 | 0.076 | −1.734 | 0.083 | ||
| Group A and Group C | −3.306 | 0.001 | −2.339 | 0.019 | −1.783 | 0.075 | ||
| Group B and Group C | −3.777 | <0.001 | −3.016 | 0.003 | −2.789 | 0.005 | ||
Comparison of PTV dosage, fitness and uniformity between ART and CT
The ART plan was better than the original CT plan in terms of PTV dosage, fitness and uniformity. Compared with the original plan, the ART plan was better in terms of Dmax, Dmean, D90, V90, V100, V95, HI and CI (t=−3.20, P=0.008; t=3.95, P=0.002; Z=−3.18, P=0.001; t=4.62, P=0.001; t=11.74, P<0.001; Z=−3.19, P=0.001; t=−7.41, P<0.001; Z=−2.60, P=0.009), and the difference was statistically significant. Compared with the original plan, the ART plan has not significantly difference in terms of the Dmin and D95 (t=−0.14, P=0.89; Z=−1.08, P=0.28) of PTV. The specific results are presented in Table 3.
Table 3
| PTV parameter | ART plan | Original CT plan | t/Z value (a is t value) | P value |
|---|---|---|---|---|
| Dmax (Gy) | 5,368.92±26.16 | 5,385.00±19.32 | −3.20a | 0.008 |
| Dmin (Gy) | 3,650.62±91.34 | 3,655.15±58.26 | −0.14a | 0.89 |
| Dmean (Gy) | 5,083.46±7.54 | 5,066.62±12.71 | 3.95a | 0.002 |
| D90 (Gy) | 5,042.46±16.25 | 5,022.15±14.83 | −3.18 | 0.001 |
| D95 (Gy) | 4,930.54±45.26 | 4,916.15±45.23 | −1.08 | 0.28 |
| V90 (%) | 99.36±0.41 | 98.77±0.35 | 4.62a | 0.001 |
| V100 (%) | 97.36±0.34 | 96.25±0.30 | 11.74a | <0.001 |
| V95 (%) | 98.44±0.29 | 97.39±0.23 | −3.19 | 0.001 |
| HI | 1.07±0.03 | 1.09±0.03 | −7.41a | <0.001 |
| CI | 0.83±0.01 | 0.81±0.02 | −2.60 | 0.009 |
PTV, planning target volume; ART, adaptive radiation therapy.
Dosimetry of endangered organs between the ART plan and original CT plan
The ART plan was lower than the original CT plan in terms of the Dmean, V5, V10, V20 and V30 of the affected lung, the Dmean, V5, V10, V20 and V30 of the double lung, the Dmean, V5, V10, V20 and V30 of the heart, and the Dmax, V5 and V10 of the contralateral breast. Compared with the original plan, the ART plan was lower in terms of the Dmean, V5, V10, V20 and V30 of the affected lung, and the Dmax, V5 and V10 of the contralateral breast, and the differences were statistically significant. The specific results are presented in Table 4.
Table 4
| Parameter | ART plan | Original CT plan | t/Z value (a is t value) | P value |
|---|---|---|---|---|
| Affected lung Dmean (Gy) | 1,203.46±35.92 | 1,476.62±39.07 | −18.06a | <0.001 |
| Double lung Dmean (Gy) | 824.69±11.10 | 837.69±14.31 | −6.67 a | <0.001 |
| Heart Dmean (Gy) | 658.67±10.12 | 668.37±13.03 | −3.11 | 0.002 |
| Contralateral breast Dmax (Gy) | 2,636.15±36.18 | 2,679.85±63.32 | −3.18 | 0.001 |
| Affected lung V5 (%) | 53.45±2.05 | 56.29±1.73 | −5.97a | <0.001 |
| Affected lung V10 (%) | 32.97±1.62 | 35.60±1.69 | −6.36a | <0.001 |
| Affected lung V20 (%) | 16.34±1.16 | 33.85±54.95 | −3.18 | 0.001 |
| Affected lung V30 (%) | 13.29±0.68 | 14.29±1.45 | −3.00a | 0.011 |
| Double lung V5 (%) | 39.97±0.98 | 41.46±0.89 | −8.80a | <0.001 |
| Double lung V10 (%) | 22.38±0.47 | 23.02±0.47 | −7.71a | <0.001 |
| Double lung V20 (%) | 9.19±0.64 | 9.55±0.58 | −8.37a | <0.001 |
| Double lung V30 (%) | 6.03±0.30 | 6.35±0.21 | −2.99 | 0.003 |
| Heart V5 (%) | 34.66±1.17 | 36.76±1.19 | −9.25a | <0.001 |
| Heart V10 (%) | 14.03±0.85 | 15.26±0.81 | −7.74a | <0.001 |
| Heart V20 (%) | 7.49±0.61 | 8.48±0.70 | −7.88a | <0.001 |
| Heart V30 (%) | 4.92±0.23 | 5.22±0.24 | −7.35a | <0.001 |
| Contralateral breast V5 (%) | 29.25±1.93 | 31.50±2.32 | −8.28a | <0.001 |
| Contralateral breast V10 (%) | 11.79±0.46 | 12.61±0.51 | −7.57a | <0.001 |
ART, adaptive radiation therapy.
Discussion
IGRT is a new radiotherapy technology for tumors, which can locate the target area and position patients through a series of imaging systems. Accurate positioning is an important guarantee for precise radiotherapy. A positioning error can cause changes in the target dose. Errors caused by positioning, including positioning scanning errors, mechanical errors and accelerator mechanical errors, have regularity and repeatability. For a patient, these errors are constant throughout the treatment process. Radiotherapy plays an important role in breast conserving surgery for breast cancer (2,11-14). IMRI is a dominant mode in the whole breast radiotherapy of breast conserving surgery for breast cancer patients, but the positioning error and change in breast volume and shape can have a key influence on the displacement of the breast target area. In order to improve these methods, and considering the advantages in CBCT in three-dimensional imaging function, CBCT was applied for positioning verification before the breast cancer radiotherapy. This provides important help for the improvement of radiotherapy accuracy and the protection of normal tissues (15).
In the preset study, it was found that the IMRI random errors after breast conserving surgery, especially the placement errors, are bound to be affected by different registration methods. In the human structure, the rib is the bone tissue closest to the breast tissue. Therefore, in the process of breathing, the rib may produce varying degrees of displacement close to the breast tissue side (16). In the present study, automatic gray registration, automatic bone marker registration, automatic gray-level registration and manual bone marker registration were used for the matching and comparison of the three-dimensional directions. Among these, automatic bone registration is usually used to calculate the skeletal gray scale registration. The advantage of automatic bone registration is that it is fast, but time-consuming, and that it is suitable for regions with relatively abundant peripheral bone tissues. The automatic gray registration criterion is calculated through the different gray scales of all images in the registration frame. The object of calculation is usually the coincidence of the CBCT images and planned images. At the same time, this registration method can also be used to correct rotation errors. In the present study, the results revealed that under different registration methods, there was a significant difference in X-direction placement errors between the automatic gray-level registration and automatic bone marker registration. This indicates that automatic gray-level registration is better than automatic bone marker registration when choosing the registration method after breast conserving surgery for breast cancer. That is, automatic gray-level registration is better than automatic bone marker registration. Compared with the placement errors in the X and Y directions of the automatic gray-scale registration and manual bone marker registration, the differences were statistically significant. The difference in placement errors in the X and Y directions of the automatic bone marker registration and automatic gray-scale registration, combined with manual bone marker registration, were statistically significant, indicating that the difference in CBCT after breast conserving surgery for breast cancer was statistically significant. The accuracy and stability of the automatic gray level registration, combined with manual bone markers in left and right directions and head and foot directions, were better than those of the automatic gray level registration and automatic bone marker registration. In the process of the actual registration, and based on the characteristics of abundant soft tissues and the relative lack of bone tissue in the breast region, the present study suggests that automatic gray registration should be the preferred method for CBCT verification, and that manual adjustment combined with the surrounding bone tissue is better. In addition, the present study revealed that the selection of automatic bone registration plus deformation registration for the ART target area is more suitable, and that the dose of the protective device tube is lower, making it more conducive for the realization of precise radiotherapy in clinic. In the present study, the standard registration frame of the XVI system was used to select the registration range, which completely covered the whole radiotherapy target area and surrounding tissues. This not only improved the registration accuracy, but also prevented the disadvantage of having a very small registration range. Since the breast is a non-rigid organ, patients should cooperate with guidance in CBCT to fully expose the breast tissue to the radiation field, while effectively ensuring the morphological tension of breast tissues. In the course of the radiotherapy, enough attention should be given to factors, such as muscle tension and skin fat thickness, in order to prevent adverse effects on the positioning error (4).
With the rapid development of testosterone gel replacement therapy (TGRT) technology, there are increasingly more ways to reduce the placement error after breast conserving surgery for breast cancer. CBCT is one of the typical auxiliary means. In the future, CBCT can be considered as a feasible imaging guidance scheme in breast conserving surgery. It is of great significance to improve the registration accuracy and reduce the positioning error. At the same time, the external situation of the target area, the selection of the appropriate time for reduction, and the re-scanning of the CT to draw up the treatment plan should be fully combined to ensure an optimal treatment effect.
Acknowledgments
Funding:
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2020.04.18). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the declaration of Helsinki (as revised in 2013). This study was conducted with approval from the Ethics Committee of Tumor Hospital Affiliated to Xinjiang Medical University (ID: XJZ-LL-2019-001). A written informed consent was obtained from all participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wu CF, Wu JC, Gu K, et al. Using CBCT to study the lower neck positioning error of breast cancer patients treated with breast bracket fixation and radiotherapy. Corresponding CTV External Boundary. Chinese Radiological Medicine and Protection 2016;36:753-6.
- Yang ZY, Wang JP, Yuan H, et al. The influence of Cone-beam CT on the positioning accuracy of patients with nasopharyngeal carcinoma undergoing intensity-modulated radiotherapy. Medical Equipment 2018;31:49-51.
- Zhao YL, Xie GD, Jin JH, et al. Application of abdominal balloon compression technology with 4DCT in 3D RT of NSCLC. Chinese Journal of Radiation Oncology 2018;5:509-12.
- Wang W, Li JB, Xu M, et al. Self-adaptive prediction and correction of placement errors in cone-beam CT-guided IMRT. Chinese Journal of Oncology 2016;38:197-201. [PubMed]
- Chai CS. Error analysis of two fixed methods in radiotherapy for breast cancer. Medical Frontier 2017;7:183-4.
- Zhong RM, Xiao Q, Zhao JL, et al. CBCT analysis of the change of the labeling position of titanium clip in breast cancer bed after breast conserving surgery. Chinese Journal of Radiation Oncology 2017;26:768-73.
- Zhou MX, Wang F, Dong D, et al. Application of CT-on-rail image guidance technology in radiotherapy of lung cancer. Journal of Anhui Medical University 2016;51:1477-80.
- Ying W, Tang DW, He YA, et al. A comparative study of two image guidance systems in head and neck cancer radiotherapy. Chinese Journal of Radiation Oncology 2016;25:155-7.
- Wang W, Li JB, Ma ZF, et al. Four dimensional radiotherapy based on cone beam CT after breast conserving surgery, intensity modulated radiotherapy before and after on-line correction of the inter temporal displacement law. Chinese Journal of Radiation Medicine and Protection 2014;34:192-5.
- Wang Y, Yu JM. Research status and progress of image-guided radiotherapy. Chongqing Medical College, 2018;47:4205-7.
- Xiao M, Lu LF, Zhou ZY. Clinical characteristics of 100 suspected breast cancer patients with imaging screening and confirmed cases. Chinese Journal of CT and MRI 2017;15:34-7.
- Tang YP, Li LJ. Error analysis of intensity modulated radiation therapy after breast conserving surgery guided by CT imaging. Chinese Medical Equipment 2017;32:87-9.
- Verma V, Choi JI, Sawant A, et al. Use of PET and other functional imaging to guide target delineation in radiation oncology. Semin Radiat Oncol 2018;28:171-7. [Crossref] [PubMed]
- Huang FJ, Ma CS, Wang RZ, et al. Applied study of 4DCT and MR image distortion matching to accurately determine the target area of primary liver cancer radiotherapy. Chinese Journal of Radiation Oncology 2017;26:555-9.
- Yang Y, Li JC, Chen JL, et al. Preliminary study on target motion of esophageal cancer based on 4DCT. Chinese Journal of Radiation Oncology 2018;27:53-7. [Crossref]
- Guo B, Li JB, Wang W, et al. Comparisons of three-dimensional CT and four-dimensional CT extreme phase partial external mammary irradiation radiotherapy plans under free breathing. Chinese Journal of Oncology 2017;39:303-7. [PubMed]


