
Immune checkpoint inhibitors in non-small cell lung cancer: is simultaneous blockade better?
Immunotherapy has proven to be a major breakthrough in the treatment of a variety of cancers, having been called the major oncologic achievement in 2015 by the American Society of Clinic Oncology. Two immune checkpoint inhibitors, antibodies to the programmed cell death protein-1 receptor (PD-1), received FDA approval in 2015 for the treatment of advanced non-small cell lung cancer, and others similar agents are actively being studied. Advancements in the treatment of lung cancer have been desperately needed as treatment strategies utilizing platinum-based doublet therapy result in modest improvements in overall survival with a median of 8–10 months and 2-year survival rates of 10–15% in patients with metastatic disease (1). The benefit of immune checkpoint inhibitors as monotherapy after progression on platinum-based chemotherapy is significant in that durable responses can be achieved. Despite this, a number of important questions remain about the optimal utilization of immune checkpoint inhibitors in lung cancer. The feasibility of combined immune checkpoint blockade, namely inhibition of the PD-1/programmed cell death ligand-1 (PD-L1) pathway together with inhibition of the cytotoxic T-lymphocyte antigen (CTLA-4), has been proven in malignant melanoma and is now being tested in non-small cell lung cancer (2).
Cancer cells have multiple mechanisms to evade the immune system. As the understanding of the complex relationship between the immune system and cancer continues to be defined, immune checkpoint inhibitors can mediate reversal of T cell exhaustion, that is caused by the activation of PD-1 pathway. In the normal function of the immune system, T-cell activity is modulated by a balance of interplaying stimulatory and inhibitory signals (3,4). Immune checkpoints are responsible for controlling the intensity of the T-cell response by serving as inhibitory signals, maintaining homeostatic balance and preventing autoimmunity. Two of these important checkpoints are CTLA-4 and the PD-1 receptor. CTLA-4 is an inhibitory T-cell receptor that is involved in regulating T-cell activation, acting in the lymphoid compartment during the initial stages of the immune response. It competes with the co-stimulatory T-cell receptor, CD28, for binding to ligands on antigen presenting cells, thereby halting T-cell activation. Additionally, it serves an important role in the function of regulatory T-cells. The PD-1 receptor works in the tumor microenvironment to regulate T-cell response. It is expressed on the cell surface of activated T-cells and has two ligands, PD-L1 and programmed cell death ligand-2 (PD-L2). When bound to these ligands, the inhibitory signal leads to reduced cytokine production and suppression of proliferation. Cancer cells use these checkpoints to evade the anticancer effects of the immune system by increasing the activity of these two inhibitory pathways. Cancer cells also up regulate PD-L1 expression, further increasing the inhibitory signal after interacting with PD-1 on T-cells. Antibodies to these immune checkpoints, inhibitors of CTLA-4 and the PD-1/PD-L1 pathway, unleash these inhibitory signals and allow the generation of a T-cell antitumor response, enabling the patient’s immune system to recognize and kill cancer cells.
The immune checkpoint inhibitors for the treatment of non-small cell lung cancer that are currently commercially available are nivolumab and pembrolizumab. Others are currently in clinical trials. Nivolumab, a fully human monoclonal antibody against PD-1, was approved by the US Food and Drug Administration (FDA) in 2015 for the treatment of patients with advanced metastatic squamous and non-squamous non-small cell lung cancer who have progressed after platinum-based chemotherapy (5). The approval was based on two Phase 3 clinical trials. The CheckMate 017 trial compared nivolumab to docetaxel in 272 squamous cell lung cancer patients who had disease progression after platinum-based chemotherapy (6). Median overall survival, the primary endpoint, was significantly improved to 9.2 months with nivolumab compared to 6 months with docetaxel (HR =0.59). One year overall survival was also higher with nivolumab (42% vs. 24%). Nivolumab also led to improvements in median progression-free survival (3.5 vs. 2.8 months, HR =0.62) and increase in objective response rate (20% vs. 9%). Nivolumab was also evaluated in 582 non-squamous non-small cell lung cancer (NSCLC) patients in the CheckMate 057 trial, a trial that mirrored CheckMate 017 in design (7). Nivolumab also proved effective is in this group showing improvements in median overall survival of 12.2 vs. 9.4 months with docetaxel (HR =0.73). Median progression-free survival (PFS) was similar between the groups (2.3 vs. 4.2 months, HR =0.92), but 1 year PFS was greater with nivolumab (18.5% vs. 8.1%). The objective response rate (ORR) was also improved with nivolumab (19.2% vs. 12.4%). Pembrolizumab, a humanized IgG4 monoclonal antibody to PD-L1, has received accelerated approval by the FDA for the treatment of advanced non-small cell lung cancer after progression on platinum-based chemotherapy (8). The Phase 1 KEYNOTE-001 study included 495 NSCLC patients who received pembrolizumab at 2 or 10 mg/kg (9). The ORR was 19.4% with a median duration of response of 12.5 months (median follow-up 10.9 months). A randomized study that included approximately 1,000 patients confirmed the superiority of pembrolizumab over docetaxel in PDL-1 expressing patients with advanced stage NSCLC. In this study, KEYNOTE-010, pembrolizumab significantly improved both median overall and progression-free survival compared to docetaxel (10). Median overall survival was 10.4 and 12.7 months, respectively, with pembrolizumab 2 and 10 mg/kg vs. 8.5 months with docetaxel. Pembrolizumab further increased overall survival among patients with at least 50% PD-L1 expression; median overall survival was 8.2 months with docetaxel compared to 14.9 months with pembrolizumab 2 mg/kg (HR =0.54) and 17.3 months with pembrolizumab 10 mg/kg (HR =0.50). While median PFS with the two therapies was similar among the entire cohort, pembrolizumab led to improved median PFS in patients with at least 50% PD-L1 expression (pembrolizumab 2 mg/kg: 5 months, pembrolizumab 10 mg/kg: 5.2 months, docetaxel 4.1 months) (Table 1).
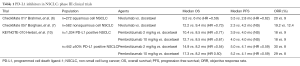
Full table
In NSCLC, immune checkpoint inhibitor monotherapy targeting the PD-1/PD-L1 pathway has shown remarkable results with improvements in OS, PFS and with ORR of 15–25% with some patients achieving durable responses lasting years. Agents blocking the PD-1/PD-L1 pathway work in the tumor microenvironment regulating the T-cell response, while CTLA-4 inhibitors provide a different mechanism targeting T-cell activation in the lymphoid compartment. Simultaneous blockade of these two pathways may provide greater antitumor activity and lead to improved outcomes in non-small cell lung cancer patients. The results of an early phase 1b trial evaluating the combination of durvalumab, an anti-PD-L1 antibody, and tremelimumab, an anti-CTLA-4 antibody, was recently published by Antonia et al. (11). This multicenter, non-randomized, open-label study enrolled 102 immunotherapy-naïve patients with locally advanced or metastatic non-small cell lung cancer. Varying dosing combinations were examined, including durvalumab at doses 3 to 20 mg/kg every 4 weeks for 13 doses, or 10 mg/kg every 2 weeks for 26 doses. Tremelimumab was administered at doses of 1, 3, or 5 mg/kg every 4 weeks for six doses followed by every 12 weeks for three doses. In 84 evaluable patients, the overall response rate was 25% across all cohorts.
Lung cancer patients are often advanced in age with many co-morbidities and limited performance status, thus tolerability to any therapy is of upmost importance. Anti-PD-1/PD-L1 therapy has been shown to be well tolerated. In the Checkmate trials, the rate of grade 3 or 4 adverse events was 7–10% with nivolumab versus 53–55% with docetaxel. There are however risks for severe life-threatening immune-related adverse events requiring close monitoring and early intervention. In the durvalumab/tremelimumab combination study by Antonia et al., adverse events resulted in 28% of patients discontinuing therapy. The maximum tolerated dose was exceeded in the cohort receiving durvalumab 20 mg/kg every 4 weeks with tremelimumab 3 mg/kg with 30% of patients (2 of 6 patients) experiencing dose-limiting toxicity. The most common grade 3 or 4 toxicities were diarrhea (11%), colitis (9%) and increased lipase (8%). Durvalumab 20 mg/kg with tremelimumab 1 mg/kg had a manageable tolerability profile and will be used as the dose moving forward in Phase 3 studies.
Simultaneous blockade of PD-1/PD-L1 and CTLA-4 has proven effective in melanoma, and the study by Antonia et al. is encouraging for the potential benefit of this strategy in non-small cell lung cancer. Higher response rates were seen relative to those seen with single-agent PD-1/PD-L1 inhibition. The clinical characteristics of many lung cancer patients can lead to poorer tolerability of more intensive therapies. Trial data revealed that doses higher than 1 mg/kg of tremelimumab resulted in greater toxicities with no improved activity; the toxicity associated with inhibition of this pathway may be a limiting factor in the combination approach. Further evaluation of the balance between efficacy and toxicity is needed. The study identified a dose with a reasonable tolerability profile, which should now be studied in larger patient cohorts. Interestingly, the combination was found to improve response rates regardless of PD-L1 status, differing from most trials with PD-1/PD-L1 monotherapy in NSCLC. Further studies will aid in determining if the PD-L1 negative population will receive the greatest benefit from the addition of CTLA-4 inhibition. Further support of the combination strategy comes from early results of CheckMate-012, a multi-arm Phase 1b trial in chemotherapy-naïve advanced non-small cell lung cancer evaluating the combination of the PD-1 inhibitor, nivolumab, and the anti-CTLA-4 antibody, ipilimumab (12). The combination was tested using four different dosing regimens in 148 patients and led to objective response rates of 13% to 39%. Clinical activity was observed regardless of PD-L1 expression. Toxicity was acceptable with 10% of fewer patients discontinuing treatment due to toxicities. The outcomes of Phase 3 studies with combination therapy will further enlighten our understanding of these agents and potentially shape the future of non-small cell lung cancer management.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Shao-Hua Cui (Department of Pulmonary Medicine, Shanghai Chest Hospital, Shanghai Jiao Tong University, Shanghai, China).
Conflicts of Interest: Dr. Ramalingam has served on scientific advisory board meetings and received honoraria from Astra Zeneca, Bristol Myers Squibb, Merck and Genentech. The other author has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Non-small cell lung cancer (version 2016). Available online: https://www.nccn.org/professionals/physician_gls/pdf/nscl_blocks.pdf
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N Engl J Med 2015;373:23-34. [Crossref] [PubMed]
- Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell 2015;27:450-61. [Crossref] [PubMed]
- Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 2012;12:252-64. [Crossref] [PubMed]
- OPDIVO (nivolumab) injection, for intravenous use. Princeton: Bristol-Myers Squibb Company; 2014.
- Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:123-35. [Crossref] [PubMed]
- Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:1627-39. [Crossref] [PubMed]
- Keytruda (pembrolizumab) injection, for intravenous use. Whitehouse Station: Merck & Co., Inc.; 2014.
- Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med 2015;372:2018-28. [Crossref] [PubMed]
- Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 2016;387:1540-50. [Crossref] [PubMed]
- Antonia S, Goldberg SB, Balmanoukian A, et al. Safety and antitumour activity of durvalumab plus tremelimumab in non-small cell lung cancer: a multicentre, phase 1b study. Lancet Oncol 2016;17:299-308. [Crossref] [PubMed]
- Rizvi NA, Gettinger SN, Goldman JW, et al. Abstract 786: Safety and efficacy of first-line nivolumab (NIVO; anti-programmed death-1 [PD-1]) and ipilimumab in non-small cell lung cancer (NSCLC). Presented at the 16th World Conference on Lung Cancer; Sept 6-9, 2015; Denver, USA.


