Prognostic value of TTF-1 expression in patients with non-small cell lung cancer: a meta-analysis
Introduction
Lung cancer remains the most lethal cancer worldwide, despite improvements in diagnostic and therapeutic techniques. Its incidence has not peaked in many parts of world, particularly in China, which has become a major public health challenge all the world (1). The prognosis for lung cancer patients is generally poor, with an overall 5 year survival rate of approximately 15%, and it has shown little improvement in recent decades (2,3). Several independent prognostic factors for survival have been identified: performance status (PS), disease stage, age, sex and amount of weight lost (4). Some of these factors are useful when choosing treatment options for an individual, principally disease stage and PS. However, the discriminant value of most potential prognostic biological markers is insufficient to predict the optimal therapeutic course for an individual (5,6).
Thyroid transcription factor 1 (TTF-1), also known as Nkx2.1 or thyroid-specific enhancer-binding protein, is a 38-kDa nuclear protein encoded by a gene located on chromosome 14q13. TTF1 is a master regulatory transcription factor for tissue-specific genes (7). TTF-1 is expressed in the thyroid, the lung and the diencephalon during embryogenesis. In normal lung, TTF1 plays a decisive role in the maintenance of the functions of terminal respiratory unit cells, where it regulates the expression of surfactant protein A (8), B (9), and C (10) and Clara cell secretory protein (11). Although the role of TTF1 as a lineage marker for terminal respiratory unit cells has been well documented (12), its role in carcinogenesis remains unclear.
The association between TTF-1 overexpression and survival in lung cancer patients has been studied for over a decade. However, no consensus has been reached; conflicting results have been reported from different laboratories. We therefore carried out a meta-analysis of data from published studies to quantitatively review the effect of TTF-1 overexpression in tumor tissue on survival in patients with non-small-cell lung cancer (NSCLC).
Materials and methods
Search strategy and study selection
The electronic databases PubMed, Embase, and CNKI (China National Knowledge Infrastructure) were searched for studies to include in our meta-analysis. An upper date limit of Jan 31, 2012 was applied; we used no lower date limit. Searches included the terms “lung cancer”, “TTF-1”, “thyroid transcription factor 1”, and “prognosis”. We also reviewed the Cochrane Library for relevant articles. The references reported in the identified studies were also used to complete the search.
Studies eligible for inclusion in this meta-analysis met the following criteria: (I) measure TTF-1 expression in the primary lung cancer tissue with IHC (immunohistochemistry) or other methods; (II) provide information on survival (studies investigating response rates only were excluded); (III) have a follow up time exceeding 5 years; and (IV) When the same author reported results obtained from the same patient population in more than one publication, only the most recent report, or the most complete one, was included in the analysis. Two reviewers (PZ and QQ) independently determined study eligibility. Disagreements were resolved by consensus.
Data extraction and quality assessment
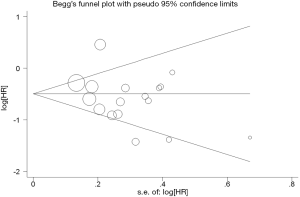
The final articles included were assessed independently by two reviewers (PZ and QQ). Data retrieved from the reports included first author, publication year, patient source, histology, disease stage, test method, TTF-1 positive and survival data (Table 1). If data from any of the above categories were not reported in the primary study, items were treated as “not applicable”. We did not contact the author of the primary study to request the information.
Full table
Statistical methods
For the quantitative aggregation of the survival results, hazard ratios (HR) and their 95% confidence intervals (CIs) were combined to give the effective value. When these statistical variables were not given explicitly in an article, they were calculated from available numerical data using methods reported by Parmar et al. (13).
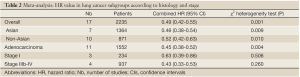
Heterogeneity of the individual HRs was calculated with Chi-squared tests according to Peto’s method (14). Meanwhile, Heterogeneity test with I2 statistic and Q statistic was performed. All the studies included were categorized by patient race, histology, disease stage. Individual meta-analysis was conducted in each subgroup. If HRs were found to have fine homogeneity, a fixed effect model was used for secondary analysis; if not, a random-effect model was used. In this meta-analysis, DerSimonian-Laird random effects analysis (15) was used to estimate the effect of TTF-1 overexpression on survival. By convention, an observed HR >1 implies worse survival for the group with TTF-1 overexpression. The impact of TTF-1 on survival was considered to be statistically significant if the 95% confidence interval (CI) did not overlap with 1. Horizontal lines represent 95% CIs. Each box represents the HR point estimate, and its area is proportional to the weight of the study. The diamond (and broken line) represents the overall summary estimate, with CI represented by its width. The unbroken vertical line is set at the null value (HR =1.0).
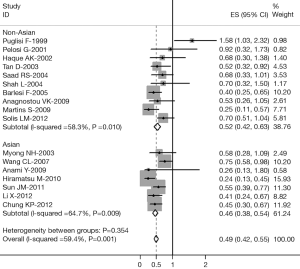
Evidence of publication bias was sought using the methods of Egger et al. (16) and of Begg et al. (17). Moreover, contour-enhanced funnel plot (18) was performed to aid in interpreting the funnel plot. If studies appear to be missing in areas of low statistical significance, then it is possible that the asymmetry is due to publication bias. If studies appear to be missing in areas of high statistical significance, then publication bias is a less likely cause of the funnel asymmetry. Intercept significance was determined by the t-test suggested by Egger (P<0.05 was considered representative of statistically significant publication bias). All calculations were performed using STATA version 11.0 (Stata Corporation, College Station, TX).
Results
Study selection and characteristics
Seventeen studies (19-35) published between 1999 and 2012 were eligible for this systematic review with meta-analysis. All reported the prognostic value of TTF-1 status for survival in NSCLC patients. The total number of patients included was 2,235, ranging from 57 to 496 patients per study (median 106). The major characteristics of the 17 eligible publications are reported in Table 1.
These publications followed several different patient cohorts. The NSCLC studies considered either all lung cancer subtypes (n=17) and adenocarcinomas (n=11). Three studies had information for stages I, 4 for stage IIIb-IV disease. All 17 studies used immunohistochemistry (IHC) to evaluate TTF-1 expression in NSCLC. Among the 17 studies evaluating TTF-1 expression in NSCLC, 7 studies (1,364 patients: 61%) were performed in Asian populations, and the remaining 10 studies (871 patients: 39%) followed European or American patients. Only one of the 17 studies identified TTF-1 overexpression as an indicator of poor prognosis, 4 studies showed no statistically significant impact of VEGF overexpression on survival, and the other 12 studies showed for favorable significance. The proportion of patients exhibiting TTF-1 overexpression in individual studies ranged from 16% to 89%.
Meta-analysis
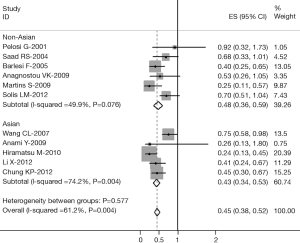
The results of the meta-analysis are reported in Table 2 and Figure 1. Overall, the combined HR for all eligible studies evaluated TTF-1 expression in NSCLC was 0.49 (95% CI: 0.42 to 0.55), indicating that TTF-1 overexpression was an indicator of favorable prognosis for NSCLC patients. However, highly significant heterogeneity was detected among these studies (I2=59.4%, P=0.001). When grouped according to the geographic settings of individual studies, the combined HRs of Asian studies and non-Asian studies were 0.46 (95% CI: 0.38-0.54) and 1.61 (95% CI: 1.49-1.73), respectively (Figure 1).
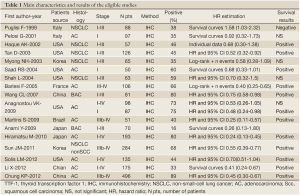
Full table
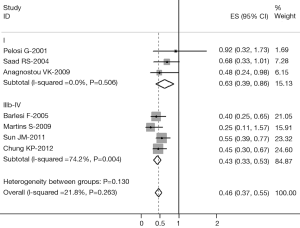
The data extracted were adequate to aggregate the studies of stage I, stage IIIb-IV NSCLC, adenocarcinoma for subgroup analyses. When we aggregated eleven studies that reported results for adenocarcinoma, the combined HR was statistically significant: HR 0.45 (95% CI: 0.38-0.52, I2=61.2%, P=0.004 for heterogeneity) (Figure 2). We also observed a statistically significant effect of TTF-1 expression on survival in stage I patients with an HR of 0.63 (95% CI: 0.39-0.86, I2=0%, P=0.506 for heterogeneity) (Figure 3) and in stage IIIb-IV patients with an HR of 0.43 (95% CI: 0.33-0.53, I2=25.3%, P=0.260 for heterogeneity) (Figure 3). There were not adequate data to aggregate studies of stage II or III NSCLC.
Publication bias
Begg’s funnel plot and Egger’s test were performed to assess the publication bias in the literature. All 17 eligible studies investigating NSCLC patients yielded a Begg’s test score of P=0.154 and an Egger’s test score of P=0.126, meanwhile according to the contour-enhanced funnel plot (Figure 4), the absence of publication bias was found in all 17 studies. These results suggest that there is no publication bias at work.
Discussion
TTF-1 is a tissue-specific transcription factor expressed mainly in the epithelial cells of the lungs and thyroid. Identification and differential diagnosis of primary lung adenocarcinoma is sometimes difficult, and TTF-1 is most commonly used to distinguish primary lung adenocarcinoma from other sources that have metastasized to the lung (36). TTF-1 has also been a useful marker for differentiating primary lung adenocarcinoma from pleural mesothelioma (37). Positive TTF-1 staining by IHC has been described in as few as 25% to as many as 80% of primary adenocarcinomas, depending on the techniques used. However, the vast majority of squamous cell carcinomas and most extrapulmonary tumors (except for thyroid) lack TTF1 expression (38-40).
TTF-1 has been investigated as a potential prognostic indicator in NSCLC with conflicting results. Seventeen studies assessing the relationship between TTF-1 and survival have been published so far, only one (19) demonstrating a negative impact, four no impact of TTF-1 on survival (20,23,24,28), others positive impact. Pelosi et al. (20) showed that TTF-1 expression did not correlate with survival; however, a trend toward better outcome was observed for patients with tumors with more than 75% immunoreactive cells. However, Saad et al. (25) showed that moderate or strong TTF-1 expression was seen in 30 (60%) of 50 patients with conventional adenocarcinoma and was associated with significantly better survival compared with patients with weak or negative staining.
In the present meta-analysis, we have combined 17 published studies including 2,235 patients with NSCLC to yield summary statistics that indicate that TTF-1 overexpression has a significant correlation with favorable survival in NSCLC and AC patients. This correlation was observed in both Asian and non-Asian study populations. When analysis was restricted to stage I and stage IIIb-IV NSCLC, we observed a statistically significant effect of TTF-1 on favorable survival, suggesting that this good prognostic factor could be of importance not only in early-stage NSCLC but also in advanced staged NSCLC. Data were not sufficient to determine the prognostic value of VEGF expression in squamous cell carcinoma.
The effect of TTF-1 was more prominent in early and locally advanced disease (stages I-III) and in lung adenocarcinomas. The previous meta-analysis also observed that high TTF-1 protein expression is associated with better survival in NSCLC, mainly in early-stage NSCLC (41). The studies with early-stage NSCLC demonstrated that TTF1 can be a prognostic factor because most patients did not receive any adjuvant therapy, and subsequently survival was less likely to be affected by other treatments, as compared with surgical resection. In addition, 4 studies (26,30,32,35) of Stage IIIb-IV NSCLC included for our meta-analysis. When analysis was restricted to stage IIIb-IV NSCLC, we found that the combined HR (0.43) was lower than the combined HR (0.63) for studies of stages I NSCLC, suggesting that TTF-1 expression could be an important favorable prognostic factor for advanced-stage NSCLC.
Recently, several systematic reviews (42-50) with meta-analyses on other biological prognostic factors for NSCLC had been reported. P53, microvessel density, HER-2, Ki-67 and RAS might be poor prognostic factors for survival in NSCLC, however, Bcl-2 might be better prognostic factor for survival in NSCLC. In order to clarify the prognostic impact of other biological factors in lung cancer, our group has performed several systematic reviews of the literature with meta-analyses. We found that VEGF (51), E-cadherin (52) and matrix metalloproteinase 2 (53) might be poor prognostic factor in NSCLC, COX-2 (54) might be poor prognostic factor for stage I NSCLC, the ground glass opacity (GGO) area (55) had a favorable prognostic value of overall survival and relapse-free survival in small lung adenocarcinoma.
Our data were consistent with the results of a previous meta-analysis (41) published in 2006 that showed an association between TTF-1 overexpression and good survival of patients with NSCLC. This analysis included only 10 studies, and the data were insufficient to determine the prognostic value in lung adenocarcinoma, disease stage. In addition, that meta-analysis did not determine the combined HR for subgroups divided according to patient ethnicity, histology, disease stage. We have improved upon that previous meta-analysis by including more recent related studies and by generally using a more comprehensive search strategy. Screening and study selection were performed independently and reproducibly by two reviewers. We also explored heterogeneity and potential publication bias in accordance with published guidelines.
This systematic review with meta-analysis was complicated by heterogeneity issues. We found highly significant heterogeneity among 17 studies of NSCLC. When the analysis was limited to 3 stage I studies of NSCLC and 4 studies of stage IIIb-IV NSCLC, but heterogeneity was detected. Therefore, disease stage was not a major source of heterogeneity.
Another potential source of bias is related to the method of HR and 95% CI extrapolation. If these statistics were not reported by the authors, we calculated them from the data available in the article. If this was not possible, we extrapolated them from the survival curves, necessarily making assumptions about the censoring process. Data for multivariate survival analysis reported in the article were included in the present systematic review with meta-analysis; if these data were not available, data calculated from survival curves by univariate analysis were included. These results should be confirmed by an adequately designed prospective study. Furthermore, the exact value of TTF-1 overexpression status needs to be determined by appropriate multivariate analysis. Unfortunately, few prospectively designed prognostic studies concerning biomarkers have been reported; thus, our collection of many retrospective studies revealed more significance.
Publication bias (56) is a major concern for all forms of meta-analysis; positive results tend to be accepted by journals, while negative results are often rejected or not even submitted. The present analysis does not support publication bias; the obtained summary statistics likely approximate the actual average. However, it should be noted that our meta-analysis could not completely exclude biases. For example, the study was restricted to papers published in English and Chinese, which probably introduced bias.
In conclusion, TTF-1 overexpression is associated with a favorable prognosis in patients with NSCLC in present meta-analysis, but there is a high heterogeneity between the studies. Interestingly, our meta-analysis suggests that TTF-1 is a favorable prognostic factor in stage I and stage IIIb-IV NSCLC and lung AC patients. These results should be confirmed by an adequately designed prospective study.
Acknowledgments
Funding: This work was supported in part by a grant from “Twelve-Five Plan” the Major Program of Nanjing Medical Science and Technique Development Foundation (Molecular Mechanism Study on Metastasis and Clinical Efficacy Prediction of Non-small Cell Lung Cancer) (Lk-Yu) and Third Level Training Program of Young Talent Project of Nanjing Health (P-Zhan).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.3978/j.issn.2218-676X.2013.02.08). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin 2010;60:277-300. [PubMed]
- Molina JR, Yang P, Cassivi SD, et al. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc 2008;83:584-94. [PubMed]
- Alberg AJ, Ford JG, Samet JM, et al. Epidemiology of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:29S-55S.
- Paesmans M, Sculier JP, Libert P, et al. Prognostic factors for survival in advanced non-small-cell lung cancer: univariate and multivariate analyses including recursive partitioning and amalgamation algorithms in 1,052 patients. The European Lung Cancer Working Party. J Clin Oncol 1995;13:1221-30. [PubMed]
- Donnem T, Bremnes RM, Busund LT, et al. Gene expression assays as prognostic and predictive markers in early stage non-small cell lung cancer. J Thorac Dis 2012;4:212-3. [PubMed]
- Osarogiagbon RU. Predicting survival of patients with resectable non-small cell lung cancer: Beyond TNM. J Thorac Dis 2012;4:214-6. [PubMed]
- Guazzi S, Price M, De Felice M, et al. Thyroid nuclear factor 1 (TTF-1) contains a homeodomain and displays a novel DNA binding specificity. EMBO J 1990;9:3631-9. [PubMed]
- Bruno MD, Bohinski RJ, Huelsman KM, et al. Lung cell-specific expression of the murine surfactant protein A (SP-A) gene is mediated by interactions between the SP-A promoter and thyroid transcription factor-1. J Biol Chem 1995;270:6531-6. [PubMed]
- Yan C, Sever Z, Whitsett JA. Upstream enhancer activity in the human surfactant protein B gene is mediated by thyroid transcription factor 1. J Biol Chem 1995;270:24852-7. [PubMed]
- Kelly SE, Bachurski CJ, Burhans MS, et al. Transcription of the lung-specific surfactant protein C gene is mediated by thyroid transcription factor 1. J Biol Chem 1996;271:6881-8. [PubMed]
- Zhang L, Whitsett JA, Stripp BR. Regulation of Clara cell secretory protein gene transcription by thyroid transcription factor-1. Biochim Biophys Acta 1997;1350:359-67. [PubMed]
- Yatabe Y, Mitsudomi T, Takahashi T. TTF-1 expression in pulmonary adenocarcinomas. Am J Surg Pathol 2002;26:767-73. [PubMed]
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 1998;17:2815-34. [PubMed]
- Yusuf S, Peto R, Lewis J, et al. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 1985;27:335-71. [PubMed]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [PubMed]
- Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [PubMed]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-101. [PubMed]
- Palmer TM, Peters JL, Sutton AJ, et al. Contour-enhanced funnel plots for meta-analysis. The Stata Journal 2008;8:242-54.
- Puglisi F, Barbone F, Damante G, et al. Prognostic value of thyroid transcription factor-1 in primary, resected, non-small cell lung carcinoma. Mod Pathol 1999;12:318-24. [PubMed]
- Pelosi G, Fraggetta F, Pasini F, et al. Immunoreactivity for thyroid transcription factor-1 in stage I non-small cell carcinomas of the lung. Am J Surg Pathol 2001;25:363-72. [PubMed]
- Haque AK, Syed S, Lele SM, et al. Immunohistochemical study of thyroid transcription factor-1 and HER2/neu in non-small cell lung cancer: strong thyroid transcription factor-1 expression predicts better survival. Appl Immunohistochem Mol Morphol 2002;10:103-9. [PubMed]
- Tan D, Li Q, Deeb G, et al. Thyroid transcription factor-1 expression prevalence and its clinical implications in non-small cell lung cancer: a high-throughput tissue microarray and immunohistochemistry study. Hum Pathol 2003;34:597-604. [PubMed]
- Myong NH. Thyroid transcription factor-1 (TTF-1) expression in human lung carcinomas: its prognostic implication and relationship with wxpressions of p53 and Ki-67 proteins. J Korean Med Sci 2003;18:494-500. [PubMed]
- Shah L, Walter KL, Borczuk AC, et al. Expression of syndecan-1 and expression of epidermal growth factor receptor are associated with survival in patients with nonsmall cell lung carcinoma. Cancer 2004;101:1632-8. [PubMed]
- Saad RS, Liu YL, Han H, et al. Prognostic significance of thyroid transcription factor-1 expression in both early-stage conventional adenocarcinoma and bronchioloalveolar carcinoma of the lung. Hum Pathol 2004;35:3-7. [PubMed]
- Barlési F, Pinot D, Legoffic A, et al. Positive thyroid transcription factor 1 staining strongly correlates with survival of patients with adenocarcinoma of the lung. Br J Cancer 2005;93:450-2. [PubMed]
- Wang CL, Yue DS, Zhang ZF, et al. Value of thyroid transcription factor-1 in identification of the prognosis of bronchioloalveolar carcinoma. Zhonghua Yi Xue Za Zhi 2007;87:2350-4. [PubMed]
- Anami Y, Iijima T, Suzuki K, et al. Bronchioloalveolar carcinoma (lepidic growth) component is a more useful prognostic factor than lymph node metastasis. J Thorac Oncol 2009;4:951-8. [PubMed]
- Anagnostou VK, Syrigos KN, Bepler G, et al. Thyroid transcription factor 1 is an independent prognostic factor for patients with stage I lung adenocarcinoma. J Clin Oncol 2009;27:271-8. [PubMed]
- Martins SJ, Takagaki TY, Silva AG, et al. Prognostic relevance of TTF-1 and MMP-9 expression in advanced lung adenocarcinoma. Lung Cancer 2009;64:105-9. [PubMed]
- Hiramatsu M, Ninomiya H, Inamura K, et al. Activation status of receptor tyrosine kinase downstream pathways in primary lung adenocarcinoma with reference of KRAS and EGFR mutations. Lung Cancer 2010;70:94-102. [PubMed]
- Sun JM, Han J, Ahn JS, et al. Significance of thymidylate synthase and thyroid transcription factor 1 expression in patients with nonsquamous non-small cell lung cancer treated with pemetrexed-based chemotherapy. J Thorac Oncol 2011;6:1392-9. [PubMed]
- Solis LM, Behrens C, Raso MG, et al. Histologic patterns and molecular characteristics of lung adenocarcinoma associated with clinical outcome. Cancer 2012;118:2889-99. [PubMed]
- Li X, Wan L, Shen H, et al. Thyroid transcription factor-1 amplification and expressions in lung adenocarcinoma tissues and pleural effusions predict patient survival and prognosis. J Thorac Oncol 2012;7:76-84. [PubMed]
- Chung KP, Huang YT, Chang YL, et al. Clinical significance of thyroid transcription factor-1 in advanced lung adenocarcinoma under epidermal growth factor receptor tyrosine kinase inhibitor treatment. Chest 2012;141:420-8. [PubMed]
- Sheppard MN. Specific markers for pulmonary tumours. Histopathology 2000;36:273-6. [PubMed]
- Ordóñez NG. Value of thyroid transcription factor-1, E-cadherin, BG8, WT1, and CD44S immunostaining in distinguishing epithelial pleural mesothelioma from pulmonary and nonpulmonary adenocarcinoma. Am J Surg Pathol 2000;24:598-606. [PubMed]
- Stenhouse G, Fyfe N, King G, et al. Thyroid transcription factor 1 in pulmonary adenocarcinoma. J Clin Pathol 2004;57:383-7. [PubMed]
- Kaufmann O, Dietel M. Thyroid transcription factor-1 is the superior immunohistochemical marker for pulmonary adenocarcinomas and large cell carcinomas compared to surfactant proteins A and B. Histopathology 2000;36:8-16. [PubMed]
- Di Loreto C, Di Lauro V, Puglisi F, et al. Immunocytochemical expression of tissue specific transcription factor-1 in lung carcinoma. J Clin Pathol 1997;50:30-2. [PubMed]
- Berghmans T, Paesmans M, Mascaux C, et al. Thyroid transcription factor 1--a new prognostic factor in lung cancer: a meta-analysis. Ann Oncol 2006;17:1673-6. [PubMed]
- Steels E, Paesmans M, Berghmans T, et al. Role of p53 as a prognostic factor for survival in lung cancer: a systematic review of the literature with a meta-analysis. Eur Respir J 2001;18:705-19. [PubMed]
- Meert AP, Paesmans M, Martin B, et al. The role of microvessel density on the survival of patients with lung cancer: a systematic review of the literature with meta-analysis. Br J Cancer 2002;87:694-701. [PubMed]
- Meert AP, Martin B, Paesmans M, et al. The role of HER-2/neu expression on the survival of patients with lung cancer: a systematic review of the literature. Br J Cancer 2003;89:959-65. [PubMed]
- Martin B, Paesmans M, Berghmans T, et al. Role of Bcl-2 as a prognostic factor for survival in lung cancer: a systematic review of the literature with meta-analysis. Br J Cancer 2003;89:55-64. [PubMed]
- Martin B, Paesmans M, Mascaux C, et al. Ki-67 expression and patients survival in lung cancer: systematic review of the literature with meta-analysis. Br J Cancer 2004;91:2018-25. [PubMed]
- Mascaux C, Iannino N, Martin B, et al. The role of RAS oncogene in survival of patients with lung cancer: a systematic review of the literature with meta-analysis. Br J Cancer 2005;92:131-9. [PubMed]
- Meert AP, Martin B, Delmotte P, et al. The role of EGF-R expression on patient survival in lung cancer: a systematic review with meta-analysis. Eur Respir J 2002;20:975-81. [PubMed]
- Nakamura H, Kawasaki N, Taguchi M, et al. Survival impact of epidermal growth factor receptor overexpression in patients with non-small cell lung cancer: a meta-analysis. Thorax 2006;61:140-5. [PubMed]
- Fan J, Wang L, Jiang GN, et al. The role of survivin on overall survival of non-small cell lung cancer, a meta-analysis of published literatures. Lung Cancer 2008;61:91-6. [PubMed]
- Zhan P, Wang J, Lv XJ, et al. Prognostic value of vascular endothelial growth factor expression in patients with lung cancer: a systematic review with meta-analysis. J Thorac Oncol 2009;4:1094-103. [PubMed]
- Wu Y, Liu HB, Ding M, et al. The impact of E-cadherin expression on non-small cell lung cancer survival: a meta-analysis. Mol Biol Rep 2012;39:9621-8. [PubMed]
- Qian Q, Wang Q, Zhan P, et al. The role of matrix metalloproteinase 2 on the survival of patients with non-small cell lung cancer: a systematic review with meta-analysis. Cancer Invest 2010;28:661-9. [PubMed]
- Zhan P, Qian Q, Yu LK. Prognostic value of COX-2 expression in patients with non-small cell lung cancer: a systematic review and meta-analysis. J Thorac Dis 2013;5:40-7. [PubMed]
- Miao XH, Yao YW, Yuan DM, et al. Prognostic value of the ratio of ground glass opacity on computed tomography in small lung adenocarcinoma: A meta-analysis. J Thorac Dis 2012;4:265-71. [PubMed]
- Begg CB, Berlin JA. Publication bias: A problem in interpreting medical data. J R Stat Soc A 1988;151:419-63.