
EGFR mutation status and brain metastases in non-small cell lung cancer: an understudied problem
Metastases to the central nervous system (CNS) in patients with non-small cell lung cancer (NSCLC) often herald a poor prognosis and a significant decrement in quality of life. Despite the substantial number of NSCLC patients who develop CNS metastases, there are few trials specifically addressing outcomes in these patients (1); many NSCLC trials studying systemic treatment exclude patients with active brain metastases. Dr. Welsh and colleagues recently published an article addressing this understudied population. They enrolled 40 NSCLC patients with brain metastases who went on to receive WBRT with concurrent administration of the epidermal growth factor receptor tyrosine kinase inhibitor (EGFR-TKI), erlotinib (2). The results indicate that the combination is feasible and tolerable with an excellent median overall survival (OS) of 19.1 months and median CNS progression free survival (PFS) of 12.3 months.
Though the survival data for concurrent therapy appear impressive compared to cited historical controls (3-6 months), they need to be interpreted in the context of data that has become available since Dr. Welch’s trial began enrollment. Multiple studies have now demonstrated the substantial progression free survival benefit of EGFR-TKIs compared with conventional chemotherapy in the first-line treatment of patients whose tumors contain EGFR activating mutations (3,4). Longitudinal studies in patients tested for EGFR mutations indicate that patients with EGFR mutations may have prolonged OS after diagnosis of brain metastases whether treated with surgical resection, WBRT and/or stereotactic radiosurgery (SRS): 14.5 months for EGFR mutations, 7.6 months for EGFR wild-type and 11.7 months total in one published study (5), suggesting that patients with EGFR mutated tumors may survive longer independent of treatment strategy.
Patients in this study were enrolled regardless of tumor EGFR mutation status. Nine of seventeen patients (53%) with available EGFR mutation testing had tumors harboring an EGFR activating mutation, much higher than what is expected in a random sample of NCSLC patients. The authors hypothesize that the over-representation of EGFR activating mutations in their sample may indicate CNS tropism of EGFR mutated tumors. Though this is an intriguing hypothesis that deserves future exploration, selection bias in this trial is a more likely explanation for the high percentage of patients enrolled with EGFR activating mutations. Trial demographics include a younger age, higher percentage of women and higher percentage of never smokers than what is typically seen in metastatic NSCLC trials - all factors that predict for an increased percentage of EGFR activating mutations (6). OS and CNS PFS were numerically higher, and cumulative incidence of CNS progression numerically lower in the patients with EGFR mutations (though underpowered and not statistically significant) highlighting the preferential activity of erlotinib in EGFR mutated tumors.
There is growing evidence that erlotinib alone has CNS activity in NSCLC patients with EGFR activating mutations. As early as 2006, there were reports of patients with brain metastases from NSCLC who had complete CNS responses after receiving erlotinib alone. In 2012, two small studies reported CNS responses comparable to those reported by Welch et al. (Table 1). This raises a very important question: can using erlotinib in EGFR-activated patients delay or obviate the need for WBRT, thereby avoiding the potential development of neurocognitive side effects from brain radiation (9)? The recently published LANDSCAPE trial attempted to answer a similar question in patients with brain metastases from Her2+ breast cancer, with promising results: a high CNS response rate (65.9%) was seen with the combination of capecitabine and lapatinib (an anti-Her2 TKI) (10).
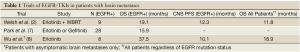
Full table
In this trial, patients with EGFR wild-type or EGFR unknown tumors had numerically inferior outcomes compared to patients with EGFR mutated tumors; but overall survival (OS) and CNS progression free survival (PFS) in these patients was still better than the authors cited historical controls. The authors highlight previously published in vitro research that shows EGFR TKIs can radiosensitize EGFR-wild type tumors. Overexpression of tumor EGFR has been hypothesized to contribute to tumor resistance to radiotherapy and reduced local control (11,12). Interestingly, EGFR blockade has not shown benefit in primary CNS tumors with increased expression of EGFR, such as glioblastoma multiforme (13). Though this trial suggests erlotinib may be active in EGFR wild-type and unknown status patients, it is important to note that the number of EGFR mutants in this study was much higher than one would expect. Without definitive knowledge of the mutational status of the “unknown” group, the benefit of concurrent erlotinib and WBRT in these patients remains unclear.
Dr. Welsh and colleagues provide a welcome focus on NSCLC patients with CNS metastases - an understudied population of NSCLC patients. Though the trial is intriguing, it is limited by small sample size, selection bias and changes in the standard of care in the patients who derived the most benefit from the combination - patients whose tumors harbor EGFR activating mutations. Since recent papers suggest that erlotinib alone can effectively treat brain metastases, we believe the best use of concurrent erlotinib and WBRT is in patients with EGFR activated tumors who have active systemic disease needing treatment and have brain metastases that are either too symptomatic to wait for a potential CNS response from erlotinib or too numerous to be amenable to stereotactic radiosurgery. This trial shows combination erlotinib and WBRT can be feasible, safe and effective.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.3978/j.issn.2218-676X.2013.02.06). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Barnholtz-Sloan JS, Sloan AE, Davis FG, et al. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol 2004;22:2865-72. [PubMed]
- Welsh JW, Komaki R, Amini A, et al. Phase II trial of erlotinib plus concurrent whole-brain radiation therapy for patients with brain metastases from non-small-cell lung cancer. J Clin Oncol 2013;31:895-902. [PubMed]
- Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009;361:947-57. [PubMed]
- Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012;13:239-46. [PubMed]
- Eichler AF, Kahle KT, Wang DL, et al. EGFR mutation status and survival after diagnosis of brain metastasis in nonsmall cell lung cancer. Neuro Oncol 2010;12:1193-9. [PubMed]
- Rosell R, Moran T, Queralt C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med 2009;361:958-67. [PubMed]
- Park SJ, Kim HT, Lee DH, et al. Efficacy of epidermal growth factor receptor tyrosine kinase inhibitors for brain metastasis in non-small cell lung cancer patients harboring either exon 19 or 21 mutation. Lung Cancer 2012;77:556-60. [PubMed]
- Wu YL, Zhou C, Cheng Y, et al. Erlotinib as second-line treatment in patients with advanced non-small-cell lung cancer and asymptomatic brain metastases: a phase II study (CTONG-0803). Ann Oncol 2013;24:993-9. [PubMed]
- Togashi Y, Masago K, Fukudo M, et al. Cerebrospinal fluid concentration of erlotinib and its active metabolite OSI-420 in patients with central nervous system metastases of non-small cell lung cancer. J Thorac Oncol 2010;5:950-5. [PubMed]
- Bachelot T, Romieu G, Campone M, et al. Lapatinib plus capecitabine in patients with previously untreated brain metastases from HER2-positive metastatic breast cancer (LANDSCAPE): a single-group phase 2 study. Lancet Oncol 2013;14:64-71. [PubMed]
- Chinnaiyan P, Huang S, Vallabhaneni G, et al. Mechanisms of enhanced radiation response following epidermal growth factor receptor signaling inhibition by erlotinib (Tarceva). Cancer Res 2005;65:3328-35. [PubMed]
- Akimoto T, Hunter NR, Buchmiller L, et al. Inverse relationship between epidermal growth factor receptor expression and radiocurability of murine carcinomas. Clin Cancer Res 1999;5:2884-90. [PubMed]
- Brown PD, Krishnan S, Sarkaria JN, et al. Phase I/II trial of erlotinib and temozolomide with radiation therapy in the treatment of newly diagnosed glioblastoma multiforme: North Central Cancer Treatment Group Study N0177. J Clin Oncol 2008;26:5603-9. [PubMed]


