Tips of laparoscopic pancreaticoduodenectomy for borderline resectable pancreatic cancer: “easy first” approach
Authors’ introduction
First author: Weiwei Jin (Figure 1) is currently on the way to get MD degree following Dr. Yiping Mou in Zhejiang University. Her research interest is focused on pancreatic disease and pancreatic surgery, especially the laparoscopic pancreaticoduodenectomy.
Corresponding author: Dr. Yiping Mou (Figure 2), MD, FACS, Professor, Chairman at Department of General Surgery, Zhejiang Provincial People’s Hospital, Hangzhou, China. Dr. Mou is expert in hepatopancreatobiliarysurgery and is pioneering in the field of laparoscopic pancreatectomy, laparoscopic gastrectomy and laparoscopic hernia repair in China. He is also the academic leader of the Major Science ‘Minimally Invasive Pancreatic and Gastric Surgery’. His interest is focused on three areas: (I) to explore the individual and minimally invasive treatment for pancreatic cancer, and try to make laparocopicpancreaticoduodenectomy routine in high volume of pancreatic centers in China; (II) to spread laparoscopic distal gastrectomy and total gastrectomy widely; (III) to improve the life quality of patients with hernia via laparoscopic approach.
Pancreatic cancer was the 7th cause of death in China in 2013 and the 4th cause of death in US and the incidence has been increasing (1). Radical resection is the only way currently available to get cure for these patients. Minimal invasive surgery has been proven with the advantages of less blood loss (2), early recovery, better cosmesis and even longer progression-free survival (3). Laparoscopic pancreaticoduodenectomy (LPD) has been achieved by several pioneering surgeons with encouraging results and more and more surgeons make attempts to perform LPD on highly selected patients successfully (2-6).
However, approximately 80% of pancreatic cancer is metastatic or locally advanced (7). It has not been known whether patients with borderline resectable pancreatic cancer (BRPC) after major vascular resection have benefit from resection or not, but the procedure for margin control has become common in many centers with similar results to that after pancreaticoduodenectomy without major venous resection though some margins are negative (8,9). There are few surgeons who are able to perform laparoscopic major vascular resection (5).
As the different view under laparoscopy, surgical steps need be changed to be more achievable, with the goal of better outcomes. This article aims to suggest a laparoscopic approach that can be applied in BRPC.
A laparoscopic procedure was selected (Figure 3) (10). The patient was a 56-year-old male with jaundice. The tumor was located in pancreatic uncinate process abutted the portal vein and superior mesenteric vein (PV/SMV) with distortion. Percutaneous transhepatic cholangial drainage (PTCD) was undergone to release jaundice.

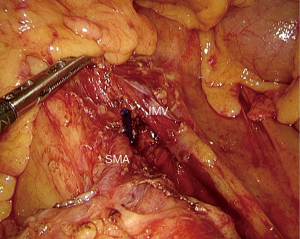
Five trocars are placed in ‘V’ shape described before. Firstly, laparoscopic exploration is carried out to exclude any peritoneal, liver or any other organ metastases. If needed, a biopsy is taken for pathological diagnosis and can help in guiding early chemotherapy. In absence of metastases, lymph nodes surrounding common hepatic artery are harvested and sent for frozen section. The common hepatic artery is then freed revealing the gastroduodenal artery (GDA) which is in turn ligated and cut off. In some cases, GDA is encased, so that the transaction of the artery is delayed until the time during the resection of uncinate process. However, no retropancreatic tunnel is created at this time as the abutment of PV/SMV. The hepatoduodenal ligament is then dissected, common hepatic artery freed from the surrounding, the gall bladder is resected and the common bile duct is freed and left suspended. The main PV and SMV at the lower edge of the pancreas need to be sure without involvement. Next, Treitz ligament is divided to indentify the superior mesenteric artery (SMA) to exclude the involvement (Figure 4). Then, transection of organs is begun.
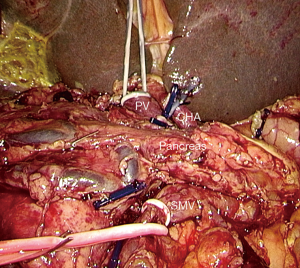
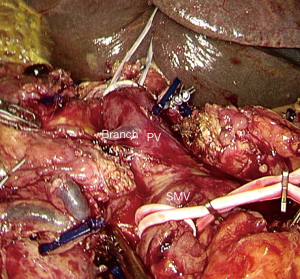
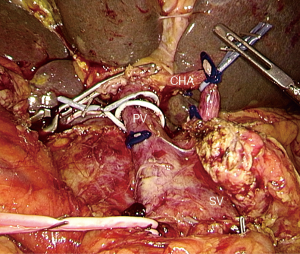
Based on the principle of “easy first”, proximal jejunum, distal stomach and common bile duct are transected. A Kocher maneuver is then performed. At this time, there is only the pancreatic neck and uncinate process that should be resected. To decrease the risk of bleeding, tapes are placed at the portal trunk, SMA and splenic vein to clamp as needed (Figure 5). Then, pancreatic neck is transected, and the PV/SMV is detached from the pancreas carefully and the veins to SMV/PV are indentified (Figure 6). If the PV/SMV could not be detached, the uncinate process is transected first. The first jejunal artery (FJA) and inferior pancreaticoduodenal artery (IPDA) are indentified and ligated. The tissue in the back of SMA is divided completely to achieve total mesopancreas excision (TMpE) from caudad to cephalad, keeping the arterial sheath intact (Figure 7). If the major vein is involved or the margin is positive, laparoscopic major vascular resection and reconstruction is needed to get R0 margin.
Discussion
Laparoscopic technique has surged in a variety of complex surgical procedures during the last 15 years. LPD has been reported as feasible and safe, and has the similar oncological outcomes for pancreatic cancer with open surgery, while the operative time may still is longer than that in open pancreaticoduodenectomy (2,3,11). With the different view under laparoscopy, some surgeons made attempts to change the surgical steps to shorten the operative or improve the outcomes (12). Our early experience for standard LPD has showed that an appropriate approach may shorten the operative time (13).
As the poor results of pancreatic cancer, aggressive surgery is performed on the patients with advanced pancreatic cancer considered unresectable previously, including major vascular resection with pancreaticoduodenectomy. Thus, the term ‘BRPC’ is used now to describe the disease that is not in the latest stage. The preoperative evaluation for BRPC is mostly based on computed tomorgraphy (CT), and the definition of BRPC is CT shows (14): (I) venous involvement of the SMV/PV allowing safe resection and reconstruction; (II) encasement of the gastroduodenal artery up to the hepatic artery without extension to the celiac axis; (III) abutment of the SMA with no more than 180 of the wall circumference.
BRPC located in the head of pancreas are always abutted the PV/SMV. Major vascular resection should be performed to get negative margin. In some cases, the abutment is inflammatory infiltration other than tumor infiltration. Some approaches have been suggested for BRPC with open pancreaticoduodenectomy to indentified the stage and make dissection easier (15-18). These approaches may be not suitable for laparoscopic surgery as the different view. The visual field is “below-up” around the axis of the mesenteric-PV in regards that laparoscope is inserted through the infraumbilical trocar. An approach with surgical steps different from those in open surgery and standard LPD may be more appropriate for BRCP.
Our approach is based on the principle “easy first”. Firstly, exploration is made to exclude the metastasis and determine the respectability. Secondly, the resection of tissues easy to perform is done. At last, pancreatic neck and uncinate process are dissected with or without the PV/SMV. Tapes are placed at the veins before resection to clamp in case. We detect the SMA in the early time to make sure the non-infiltration of the artery. ‘Easy first’ is designed to decrease the risk of bleeding, and make smaller incision in the case that conversion to open surgery is needed when resecting the pancreatic neck or uncinate process. So as the placement of tapes, all the details are to control the injury.
In most centers, involvement of the PV/SMV is considered as a contraindication for LPD because laparoscopic major vascular resection (LMVR) is a very difficult technique now. The first report with 11 cases was published in 2011 (19), suggesting that LMVR was safe and beneficial in experienced hands both open pancreaticoduodenctomy and LPD. The other comparative research showed that LMVR could achieve similar outcomes with the open surgery (3).
In conclusion, LPD is feasible and safe, and an appropriate approach is good for achieving the goal with better outcomes. ‘Easy first’ approach is useful in patients with BRPC in case to control the injury.
Acknowledgments
Funding: Zhejiang Key Subject of Medical Science (11-CX-21). Zhejiang Provincial Medical and Health Science and Technology (2015DTA010).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.08.20). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014. CA Cancer J Clin 2014;64:9-29. [Crossref] [PubMed]
- Nigri G, Petrucciani N, La Torre M, et al. Duodenopancreatectomy: open or minimally invasive approach? Surgeon 2014;12:227-34. [Crossref] [PubMed]
- Croome KP, Farnell MB, Que FG, et al. Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg 2014;260:633-8; discussion 638-40. [Crossref] [PubMed]
- Kim SC, Song KB, Jung YS, et al. Short-term clinical outcomes for 100 consecutive cases of laparoscopic pylorus-preserving pancreatoduodenectomy: improvement with surgical experience. Surg Endosc 2013;27:95-103. [Crossref] [PubMed]
- Croome KP, Farnell MB, Que FG, et al. Pancreaticoduodenectomy with major vascular resection: a comparison of laparoscopic versus open approaches. J Gastrointest Surg 2015;19:189-94; discussion 194. [Crossref] [PubMed]
- Asbun HJ, Stauffer JA. Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg 2012;215:810-9. [Crossref] [PubMed]
- Verbeke CS, Gladhaug IP. Resection margin involvement and tumour origin in pancreatic head cancer. Br J Surg 2012;99:1036-49. [Crossref] [PubMed]
- Al-Haddad M, Martin JK, Nguyen J, et al. Vascular resection and reconstruction for pancreatic malignancy: a single center survival study. J Gastrointest Surg 2007;11:1168-74. [Crossref] [PubMed]
- Riediger H, Makowiec F, Fischer E, et al. Postoperative morbidity and long-term survival after pancreaticoduodenectomy with superior mesenterico-portal vein resection. J Gastrointest Surg 2006;10:1106-15. [Crossref] [PubMed]
- Jin W, Ajoodhea H, Mou Y, et al. A case with a 56-year-old male who presented abdominal pain and jaundice for half a month. PTCD was performed before operation. CT and MR showed pancreatic uncinate process mass with superior mesenteric vein abuntmen. Asvide 2016;3:400. Available online: http://www.asvide.com/articles/1171
- Gumbs AA, Rodriguez Rivera AM, et al. Laparoscopic pancreatoduodenectomy: a review of 285 published cases. Ann Surg Oncol 2011;18:1335-41. [Crossref] [PubMed]
- Asbun HJ, Stauffer JA. Laparoscopic pancreaticoduodenectomies: a word of caution. J Am Coll Surg 2013;216:1218-20. Author reply. [Crossref] [PubMed]
- Zhang MZ, Xu XW, Mou YP, et al. Resection of a cholangiocarcinoma via laparoscopic hepatopancreato- duodenectomy: a case report. World J Gastroenterol 2014;20:17260-4. [Crossref] [PubMed]
- National Comprehensive Cancer Network. NCCN practice guidelines for pancreatic cancer, version 2. Available online: http://www.nccn.org/professionals/physician_gls/recently_updated.asp
- Kurosaki I, Minagawa M, Takano K, et al. Left posterior approach to the superior mesenteric vascular pedicle in pancreaticoduodenectomy for cancer of the pancreatic head. JOP 2011;12:220-9. [PubMed]
- Weitz J, Rahbari N, Koch M, et al. The "artery first" approach for resection of pancreatic head cancer. J Am Coll Surg 2010;210:e1-4. [Crossref] [PubMed]
- Pessaux P, Varma D, Arnaud JP. Pancreaticoduodenectomy: superior mesenteric artery first approach. J Gastrointest Surg 2006;10:607-11. [Crossref] [PubMed]
- Sanjay P, Takaori K, Govil S, et al. 'Artery-first' approaches to pancreatoduodenectomy. Br J Surg 2012;99:1027-35. [Crossref] [PubMed]
- Kendrick ML, Sclabas GM. Major venous resection during total laparoscopic pancreaticoduodenectomy. HPB (Oxford) 2011;13:454-8. [Crossref] [PubMed]