
How are lung cancer risk perceptions and cigarette smoking related?—testing an accuracy hypothesis
Introduction
Subjective risk perception, defined as “one’s belief about the likelihood or probability of harm, namely the probability that a health problem will be experienced if no precautions or behavioral changes occur (1)”, is an important theoretical construct in the field of cancer prevention and control. Subjective risk perception is often measured by absolute risk perception and relative (comparative) risk perception. The former examines a person’s perception of the likelihood that he or she will get a certain disease within a defined time period; the latter assesses how a person compares the likelihood that he or she will get a certain disease to the likelihood that similar others will get the disease over a defined time period (2-6).
Although the relationship between subjective risk perception and health behavior in general has widely been researched, the association between risk perception of acquiring lung cancer and cigarette smoking is unclear. Studies have suggested causal relationships between lung cancer risk perception and cigarette-smoking behaviors in positive, negative, and no significant directions (7-11). Moreover, instead of causality relations, some studies have simply reported a positive correlation between lung cancer risk perception and smoking probability (12-16), whereas other studies found different associations (17,18).
Such inconsistent and mixed findings may confuse researchers about the relationship between lung cancer risk perception and smoking behaviors. We propose that these mixed data may be due to readers’ possible misinterpretations of the association between lung cancer risk perception and smoking behaviors in literature. This may also have resulted from discrepancies between study designs and the tested risk perception-risk behavior hypotheses as well as from differences in the hypothesized underlying associations between risk perception and behaviors among studies.
To elucidate the association between lung cancer subjective risk perception and smoking behaviors, it is important to understand three primary types of hypotheses that have been used to evaluate risk perception-risk behavior relationships: the behavior motivation hypothesis, the risk reappraisals hypothesis, and the accuracy hypothesis (10,19). Because these three risk perception-risk behavior hypotheses are based on different types of theories, testing each of them requires different study designs and statistical techniques. In particular, the behavior motivation hypothesis, comparable to the concepts of most health behavior theories (20), suggests that if people perceive that their risk of getting a disease is high, they will be more likely to adopt subsequent healthy behaviors. A longitudinal design is required to test the causal nature of this hypothesis. In contrast to the behavior motivation hypothesis, the risk reappraisals hypothesis is similar to emotion-based theories (21). It states that if people take or intend to take a protective behavior, they will further reduce risk perception. Due to causal relationships, assessing this hypothesis also needs a longitudinal design to collect both risk perception and health behavior data at multiple time points. Finally, the accuracy hypothesis solely tests the correlation between risk perception and risk behaviors. This hypothesis tests whether individuals’ risk perception accurately reflects risk behaviors at the same time point (e.g., people who smoke have a heightened risk perception of getting lung cancer). Thus, researchers can employ a cross-sectional design to collect and evaluate both risk perception and protective behaviors data at the same single time point (10,19,22).
Given that most prior studies, which assessed the relations between lung cancer subjective risk perception and smoking behaviors, have adopted a cross-sectional design, assessing the accuracy hypothesis is the most appropriate approach for examining this kind of data and concluding the findings. Nevertheless, researchers have sometimes drawn implications from their data based on causal risk perception-risk behavior hypotheses (i.e., the behavior motivation hypothesis and the risk reappraisals hypothesis). As an initial step to address this issue, we demonstrated the examination of the accuracy hypothesis by analyzing a large national dataset—the 2005 U.S. Health Information National Trends Survey [HINTS 2005] dataset.
Our study will contribute to existing cancer prevention and control research not only by matching the hypothesis to the type of data, but also by helping better understand how individuals view the relationship between their perceived lung cancer risk and cigarette smoking. Moreover, compared to past research that restricted their samples to certain groups and measured one type of risk perception and a single smoking behavior, our study expands existing literature by analyzing a large sample drawn from the general public and by using multiple measures for both risk perceptions and smoking behavior. Specifically, previous studies have often restricted their samples to smokers, cancer patients, or other specific groups. This study examined a large and nationally representative sample of U.S. adults (18 years of age or older). Furthermore, we tested both absolute and relative risk perceptions to better capture the subjective risk perception. Lastly, we not only examined the most commonly used variable to assess smoking behaviors (i.e., having smoked at least 100 cigarettes in lifetime), but also evaluated two other variables related to the amount of cigarette use (i.e., both the frequency of smoking and number of cigarettes smoked).
Methods
Dataset and study design
We analyzed the HINTS 2005 dataset, which was collected by the National Cancer Institute in the United States. Using a list-assisted random-digit-dial method to initially draw a random sample of telephone numbers from U.S. households, HINTS 2005 data were collected via both telephone interview and web-based survey. Hispanics and African Americans were oversampled. To adjust for the complex sampling method, data were weighted, and 5,586 U.S. adults (age ≥18 years) comprised the nationally representative sample. The adjusted response rate was 20.83% (23) (for details about the dataset, see the NCI’s website—http://hints.cancer.gov/). In this study, we first excluded respondents with a personal history of lung cancer and those who were unable to respond to the survey in English, yielding a sample size of 5,105 respondents. Additionally, because one-third of the sample population was randomly selected to answer both subjective risk perception questions, only those selected respondents were included in the analyses. The final sample size consisted of 1,680 participants. This exempt secondary data study was approved by the research team’s institutional review boards.
Measures
Subjective (absolute and relative) risk perceptions
Two items assessed respondents’ subjective perceived risk of developing lung cancer. The absolute risk perception item asked: “How likely do you think it is that you will develop lung cancer in the future (very low, somewhat low, moderate, somewhat high, and very high)?” The relative risk perception item asked: “Compared to the average person your age, would you say that you are more likely, about as likely, or less likely to get lung cancer?”
Cigarette-smoking behaviors
We selected three questions from HINTS 2005 related to respondents’ cigarette-smoking behaviors. The first question was whether participants had smoked at least 100 cigarettes in their entire lives. Those answering “yes” were asked a second question concerning how often they smoked cigarettes (every day, some days, or not at all). Those who reported smoking every day were then asked how many cigarettes they smoked per day on average.
Covariates
We selected covariates to test for inclusion in our models based on existing risk perception literature (24). These included age, gender, race/ethnicity, marital status, educational level, household income, family history of lung cancer, perceived health status, health care coverage, and use of health communication channels (e.g., frequency of reading health information in newspapers/magazines).
Statistical analyses
SUDAAN software Version 9.0 was used to perform all statistical analyses incorporating the dataset replicate sampling weights. We first examined descriptive statistics for all variables, including weighted frequencies and 95% confidence intervals. Binary logistic regression models were built to examine the associations between risk perceptions (i.e., absolute risk perception and relative risk perception) and whether participants had smoked at least 100 cigarettes in their entire lifetimes (yes vs. no). A chi-square test was used to determine statistical significance at an alpha level of less than 0.05. Because frequency of cigarette smoking was coded as more than two categories (i.e., every day, some days, and not at all), we used multinomial logistic regression with the Wald F test to assess the association between this variable and subjective risk perception. We utilized multivariate linear regression models to examine the relationship between risk perception and the continuous variable of number of cigarettes smoked per day. To construct the final regression models, we used Hosmer and Lemeshow’s forward checking and backward elimination methods to select significant covariates based on the P<0.20 criterion (25-27).
Results
Sample characteristics
Table 1 shows the characteristics of the respondents. Among the 1,680 participants in the final sample, the mean age was 46.3 years (standard error =0.5). Respondents were mostly White, non-Hispanic (weighted percentage =77.2%), married/living with a partner (64.3%), had some health care coverage (89.0%), and about half (56.1%) were women. Less than half of the respondents rated their health status as being very good or excellent (39.5%). The majority of participants had a college-level education or greater (57.2%) and reported an annual household income of at least $50,000 (53.4%). One-fifth of respondents (20.0%) reported that they had a family history of lung cancer.
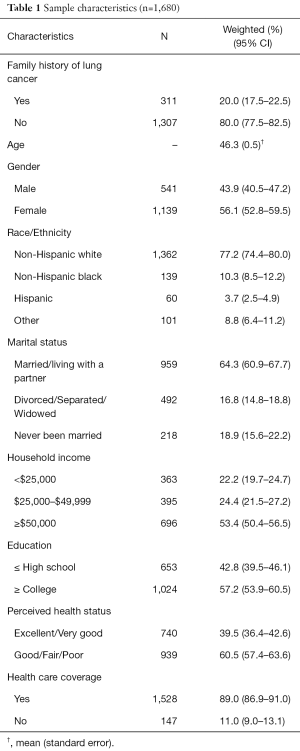
Full table
Subjective (absolute and relative) risk perceptions of lung cancer
Respondents generally had a low absolute risk perception of developing lung cancer. As shown in Table 2, 47% rated their risk as being very low with 22.6% as somewhat low and 18.4% as moderate. Only 12.1% of respondents rated their risk of getting lung cancer as being somewhat high or very high. Participants had a fairly low relative perceived risk of developing lung cancer. Almost 60% of respondents reported that they were less likely to get lung cancer compared to the average person their age, and 28.9% rated their risk as being similar to that of other people of the same age. Only 11.8% of respondents felt their risk of developing lung cancer was higher than others their age.
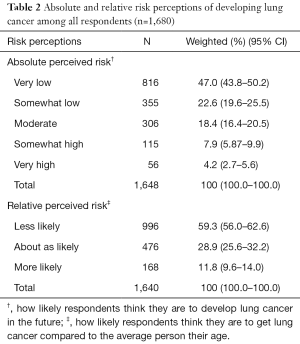
Full table
Cigarette-smoking behaviors
Nearly half (48.8%, n=822) of the respondents had smoked at least 100 cigarettes in their lifetimes. Among those people, 38.2% smoked every day, 9.8% smoked some days, and 52.0% reported that they did not smoke at all. Those who smoked every day (n=235) were subsequently asked the average number of cigarettes they smoked per day; the mean value was 16.5 cigarettes (SE =0.80, range, 1–60).
Relationships between subjective (absolute and relative) risk perceptions and cigarette-smoking behaviors
After controlling covariates in regression models, our study showed that having higher (both absolute and relative) risk perceptions of getting lung cancer was associated with a higher likelihood of having smoked at least 100 cigarettes in participants’ lifetime (OR =2.82; 95% CI, 2.39–3.35 for absolute risk perception; OR =4.40; 95% CI, 3.38–5.73 for relative risk perception; see Table 3). Additionally, absolute risk perception was positively associated with the frequency of cigarette smoking among ever smokers (OR =3.94; 95% CI, 2.74–5.66 for smoking every day versus not smoking; OR =2.27; 95% CI, 1.63–3.15 for smoking some days versus not smoking). Similarly, there was a positive relationship between relative perception and the frequency of cigarette smoking among ever smokers (OR =3.65; 95% CI, 2.47–5.40 smoking every day versus not smoking; OR =2.04; 95% CI, 1.38–3.02 smoking some days versus not smoking).
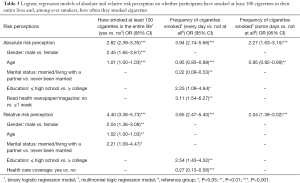
Full table
For the association between subjective (absolute and relative) risk perceptions and the number of cigarettes respondents smoked per day among current smokers, however, the positive relationship was statistically significant for absolute risk perception (β=0.21; SE =0.06; 95% CI, 0.09–0.34), but not for relative risk perception (β=0.08; SE =0.06; 95% CI, –0.04–0.19) in multivariate models (Table 4).
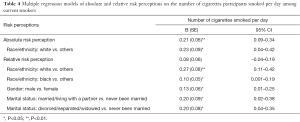
Full table
Discussion
This study examined the association between lung cancer subjective (both absolute and relative) risk perceptions and cigarette-smoking behaviors among a large and nationally representative sample of U.S. adults, including both smokers and non-smokers. As an initial step, this study contributes to the cancer prevention and control field by clarifying how individuals interpret the relation between perceived lung cancer risk and their cigarette-smoking behaviors. In addition, it demonstrates how to appropriately identify and examine a risk perception-risk behavior hypothesis for cross-sectional survey data. Specifically, our results reveal the presence of a positive correlation between both absolute and relative risk perceptions and various cigarette-smoking behaviors. Because this is a correlation analysis, we could only test the accuracy hypothesis. Our findings support the accuracy hypothesis—people who smoke are generally aware that they have an increased risk of getting lung cancer. It is important to keep in mind that these data cannot be extrapolated to suggest causal relationships—either that higher lung cancer risk perception would lead to more smoking activities, or that engaging in smoking behavior leads to higher risk perception of getting lung cancer.
The findings reported here are consistent with those from prior research showing positive associations between absolute risk perception of acquiring lung cancer and smoking behaviors. For instance, Weinstein et al. (12) found a positive correlation between absolute risk perception and number of cigarettes smoked per day in a sample of 1,245 smokers. Dillard and Klein (13) used the same dataset, limiting their sample to current smokers with valid objective and subjective lung cancer risk data (n=377), and also observed that absolute risk perception was positively related to the number of cigarettes smoked per day. Our study extends previous work by examining more than one type of subjective risk perceptions and multiple cigarette-smoking behaviors (i.e., having smoked at least 100 cigarettes in entire lifetime, the frequency of smoking, and the number of cigarettes smoked). In addition, our sample consisted of a nationally representative sample of U.S. adults, including both smokers and non-smokers.
In this study, we found that individuals currently engaging in cigarette-smoking behaviors at the time perceived their risk of developing lung cancer as being increased. This finding suggests that lay people may generally be aware of the lung cancer health hazard message of cigarette smoking disseminated through widespread anti-smoking efforts by the U.S. government, mass media, and other non-profit organizations. Thus, health promotion strategies other than those focused on risk perception for lung cancer (e.g., programs to educate the risk of other types of cancers and diseases related to smoking, nicotine replacement therapy, behavioral treatments, and other medical aids) may be needed to increase the success of smoking prevention and control programs.
Furthermore, our findings suggest some differences between absolute and relative risk perceptions related to smoking behaviors. While both absolute and relative risk perceptions were associated with smoking at least 100 cigarettes during respondents’ lifetimes and the frequency of their cigarette smoking, only absolute risk perception was related to the number of cigarettes that current smokers smoked per day. These findings suggest that absolute risk perception, rather than relative risk perception, might be a more sensitive index with which to measure perceived lung cancer risk. A potential explanation for these findings is that although both absolute and relative risk perceptions are types of subjective risk perceptions, these constructs are somewhat different. Past research, for instance, has indicated that absolute and relative risk perceptions explain different types of cancer worries and healthy behaviors (3,28). A previous study also found that relative risk perception was not correlated with the number of cigarettes an individual smoked per day (12). Future studies are needed to explore why absolute risk perception might better capture associations with smoking behaviors and via which mechanism.
Given that this study was a secondary data analysis; our results are limited by the measurement of subjective risk perception in the HINTS 2005 dataset. Only one-third of the sample was randomly selected to answer questions related to subjective risk perceptions of getting lung cancer. Moreover, HINTS 2005 asked people to rate their lung cancer risk based on verbal scales (e.g., very low, somewhat low, moderate, somewhat high, and very high for absolute risk perception), which may yield different results than numerical scales (28,29). Additionally, the assessment of absolute risk perception was based on a 5-point scale, while a 3-point scale was utilized to assess relative risk perception. Although this difference might have affected the findings of this study, we found a similar pattern between these two different types of risk perceptions. The other limitation of this study is that we used the HINTS dataset from 2005. While using the latest HINTS dataset is desirable, the latest versions do not include questions regarding subjective risk perceptions of getting lung cancer. Given that the purpose of this study is to test an accuracy hypothesis, HINTS 2005 provides a national, representative sample with which we were able to examine our hypothesis.
Conclusions
In conclusion, our findings contributed to translational cancer research from a methodological perspective. When reading and interpreting scientific literature regarding risk perception and cigarette-smoking behaviors, researchers need to keep in mind (I) which hypotheses (i.e., the behavior motivation hypothesis, the risk reappraisals hypothesis, and the accuracy hypothesis) the studies examined, (II) which study designs (i.e., cross-sectional and longitudinal designs) the studies used, and (III) whether or not the hypothesis matched the research design. Based on the findings of this study, we propose a number of future research directions and recommendations. First, although our data support the accuracy hypothesis, longitudinal research with long-term data is needed to investigate other risk perception-risk behavior hypotheses, such as behavior motivation and risk reappraisals, among nationally representative samples to further examine the direction of causation for the association between risk perception and smoking behavior. Second, a systematic review or meta-analysis is particularly needed to provide an evidence-based understanding of the relationship between risk perception and cigarette smoking. Such systematic review or meta-analysis can help develop evidence-based cancer prevention and intervention programs. Third, in our study, we only focused on cigarette-smoking behaviors. Future research could examine risk perception and the use of different types of cigarettes people smoke (e.g., light and “natural” cigarettes, snus, snuff, dissolvables, cigars, and little cigars). Lastly, we examined risk perception for lung cancer because smoking is commonly linked to lung cancer; however, it may be useful to evaluate individuals’ risk perception regarding other types of cancers and diseases.
Acknowledgments
Funding: This research was supported by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health. We thank Julie Williams and Sonju Harris at Abt Associates Inc. for offering statistical support and consultations for this study.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Translational Cancer Research for the series “Social Behavioral and Genetic Risk factors for Cancer”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.10.75). The series “Social Behavioral and Genetic Risk factors for Cancer” was commissioned by the editorial office without any funding or sponsorship. TST served as the unpaid Guest Editor of the series. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the research team’s institutional review boards (No. 07-135).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Katapodi MC, Lee KA, Facione NC, et al. Predictors of perceived breast cancer risk and the relation between perceived risk and breast cancer screening: a meta-analytic review. Prev Med 2004;38:388-402. [Crossref] [PubMed]
- Lipkus IM, Kuchibhatla M, McBride CM, et al. Relationships among breast cancer perceived absolute risk, comparative risk, and worries. Cancer Epidemiol Biomarkers Prev 2000;9:973-5. [PubMed]
- Zajac LE, Klein WM, McCaul KD. Absolute and comparative risk perceptions as predictors of cancer worry: moderating effects of gender and psychological distress. J Health Commun 2006;11:37-49. [Crossref] [PubMed]
- Rose JP, Nagel B. Relation between comparative risk, absolute risk, and worry: the role of handedness strength. J Health Psychol 2013;18:866-74. [Crossref] [PubMed]
- Zhao X, Nan X. The Influence of Absolute and Comparative Risk Perceptions on Cervical Cancer Screening and the Mediating Role of Cancer Worry. J Health Commun 2016;21:100-8. [Crossref] [PubMed]
- Ranby KW, Aiken LS, Gerend MA, et al. Perceived susceptibility measures are not interchangeable: absolute, direct comparative, and indirect comparative risk. Health Psychol 2010;29:20-8. [Crossref] [PubMed]
- Lundborg P, Lindgren B. Do They Know What They are Doing? Risk Perceptions and Smoking Behaviour Among Swedish Teenagers. J Risk Uncertainty 2004;28:261-86. [Crossref]
- Viscusi WK. Do Smokers Underestimate Risks? J Polit Econ 1990;98:1253-69. [Crossref]
- Viscusi WK. Age Variations in Risk Perceptions and Smoking Decisions. Rev Econ Stat 1991;73:577-88. [Crossref]
- Hay JL, Ostroff J, Burkhalter J, et al. Changes in cancer-related risk perception and smoking across time in newly-diagnosed cancer patients. J Behav Med 2007;30:131-42. [Crossref] [PubMed]
- Finney Rutten LJ, Blake KD, Hesse BW, et al. Illness representations of lung cancer, lung cancer worry, and perceptions of risk by smoking status. J Cancer Educ 2011;26:747-53. [Crossref] [PubMed]
- Weinstein ND, Marcus SE, Moser RP. Smokers' unrealistic optimism about their risk. Tob Control 2005;14:55-9. [Crossref] [PubMed]
- Dillard AJ, McCaul KD, Klein WM. Unrealistic optimism in smokers: implications for smoking myth endorsement and self-protective motivation. J Health Commun 2006;11:93-102. [Crossref] [PubMed]
- Hahn EJ, Rayens MK, Hopenhayn C, et al. Perceived risk and interest in screening for lung cancer among current and former smokers. Res Nurs Health 2006;29:359-70. [Crossref] [PubMed]
- Park ER, Ostroff JS, Rakowski W, et al. Risk perceptions among participants undergoing lung cancer screening: baseline results from the National Lung Screening Trial. Ann Behav Med 2009;37:268-79. [Crossref] [PubMed]
- Helweg-Larsen M, Nielsen GA. Smoking cross-culturally: risk perceptions among young adults in Denmark and the United States. Psychol Health 2009;24:81-93. [Crossref] [PubMed]
- Liu JT, Hsieh CR. Risk perception and smoking behavior: Empirical evidence from Taiwan. J Risk Uncertainty 1995;11:139-57. [Crossref]
- Helweg-Larsen M, Stancioff LM. Acculturation matters: risk perceptions of smoking among Bosnian refugees living in the United States. J Immigr Minor Health 2008;10:423-8. [Crossref] [PubMed]
- Brewer NT, Weinstein ND, Cuite CL, et al. Risk perceptions and their relation to risk behavior. Ann Behav Med 2004;27:125-30. [Crossref] [PubMed]
- Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. San Francisco: John Wiley & Sons, 2008.
- Witte K, Meyer G, Martell D. Effective health risk messages: A step-by-step guide. Thousand Oaks: Sage Publications, 2001.
- Renner B, Schüz B, Sniehotta FF. Preventive health behavior and adaptive accuracy of risk perceptions. Risk Anal 2008;28:741-8. [Crossref] [PubMed]
- National Cancer Institute. HINTS Available online: http://hints.cancer.gov, accessed August 1st 2016.
- Chen LS, Kaphingst KA. Risk perceptions and family history of lung cancer: differences by smoking status. Public Health Genomics 2011;14:26-34. [Crossref] [PubMed]
- Hosmer Jr DW, Lemeshow S, Sturdivant RX. Applied logistic regression. San Francisco: John Wiley & Sons, 2013.
- Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol 1993;138:923-36. [PubMed]
- Budtz-Jørgensen E, Keiding N, Grandjean P, et al. Confounder selection in environmental epidemiology: assessment of health effects of prenatal mercury exposure. Ann Epidemiol 2007;17:27-35. [Crossref] [PubMed]
- Dillard AJ, Ferrer RA, Ubel PA, et al. Risk perception measures' associations with behavior intentions, affect, and cognition following colon cancer screening messages. Health Psychol 2012;31:106-13. [Crossref] [PubMed]
- Weinstein ND, Atwood K, Puleo E, et al. Colon cancer: risk perceptions and risk communication. J Health Commun 2004;9:53-65. [Crossref] [PubMed]


