A genomic analysis of large cell neuroendocrine carcinoma versus small cell lung cancer: which is which?
Neuroendocrine tumors are a vastly diverse group of tumors developed by neuroendocrine cells. Neuroendocrine cells are found throughout the whole body, and function in hormone regulation and epithelium repair. In the lung, there are various types of neuroendocrine tumors, one being large cell neuroendocrine carcinoma (LCNEC). LCNEC is a rare and aggressive subtype of non-small cell lung cancer (NSCLC) and is usually treated as a type of NSCLC (1-4). However, in recent years, it has been shown that LCNEC shares similar histological, immunohistochemical (IHC), and molecular characteristics with small cell lung cancer (SCLC), despite the different characterization of the size of the cells (5). Consequently, there have been recent studies testing various combination therapies on both LCNEC and SCLC, but have resulted in somewhat poorer outcome amongst LCNEC patients than patients with SCLC (6). This highlights the ongoing ambiguity and lack of optimal clinical treatment of LCNEC versus SCLC, and motivates further genomic investigation of these two types of neoplasms. There are currently no approved targeted therapies specifically for LCNEC or SCLC; chemotherapy is presently the only therapeutic option (2).
Miyoshi and colleagues examined a Japanese patient cohort consisting of a total of 78 formalin-fixed paraffin-embedded (FFPE) LCNEC samples by using a 244 cancer-related gene targeted exon next-generation sequencing approach to discover genomic alterations. This cohort comprised of 55 surgically resected LCNEC, 13 advanced-stage LCNEC biopsies, and 10 combined LCNEC with NSCLC components. The vast majority of the patients were ever smokers (97% and 98% in LCNEC and SCLC, respectively). They then compared the LCNEC genomic profile to 141 SCLC patients’ genomic alterations: 90 biopsy samples; 50 surgically resected samples and one advanced SCLC sample from Miyoshi et al. previous data (7). Of these SCLC samples, 12 were of a combined type; however, it was not specified which SCLC was of a combined form. Comparison of the LCNEC and SCLC genetic alteration data was used to produce a molecular profile of LCNEC to predict molecular targeted therapies and cancer progression (8).
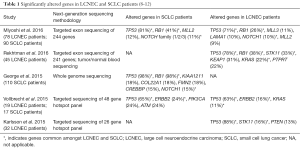
Miyoshi and colleagues identified a high prevalence of mutations in TP53 and RB1 genes in LCNEC; however, SCLC had a much higher frequency of RB1 mutations when compared to LCNEC (Table 1). In addition, they identified targetable activating mutations in KIT, EGFR, ERBB2, and FGFR1 genes, and found a higher copy number gain in ERBB2 and SETBP1 genes in LCNEC when compared to SCLC. Other mutated genes which were significantly more frequent in LCNEC included LAMA1, PCLO, MEGF8, and RICTOR. Yet, overall, Miyoshi and colleagues concluded that LCNEC and SCLC have similar genomic profiles. The majority of the genetic alterations were related to the PI3K/AKT/mTOR pathway, which could be a potential target pathway in LCNEC tumor formation and progression. In patients with LCNEC combined with adenocarcinoma, Miyoshi and colleagues found known oncogenic mutations within both cell components in the genes EGFR (E746_A750 del, exon 19) and KRAS (G12V), while a patient with LCNEC combined with squamous cell carcinoma had a PIK3CA gene activating mutation in both cell components (8).
In a recent report, Rekhtman et al. compared the genomic profiles of LCNEC and NSCLC. In agreement with Miyoshi and colleagues’ data, Rekhtman et al. also found TP53 and RB1 genes to be the two most commonly mutated genes in LCNEC. In the Rekhtman et al. whole LCNEC cohort, they included additional genes STK11, KEAP1, and KRAS to be among the next most commonly mutated genes in LCNEC; however, in the SCLC-like LCNEC subset, (defined as LCNEC with co-altered inactivation of RB1 and TP53), there was a complete absence of STK11 and KRAS mutations, and an enriched existence of MYCL, SOX2, and FGFR1 amplifications. They also identified the PI3K/AKT/mTOR pathway to be among the most frequently altered gene family/functional group. Furthermore, Rekhtman et al. discovered about 30% of the NSCLC-like LCNEC to have a distinct mutation profile, mostly consisting of loss-of-function mutations in the NOTCH family genes, which are key regulators of neuroendocrine differentiation. The most prominent alteration in SCLC-like LCNEC versus SCLC was an increased frequency of KEAP1-NFE2L2 aberrations, which rarely occur in traditional SCLC patients, but are known to be prevalent in STK11/KRAS wildtype squamous cell carcinomas (9).
A small percentage of neuroendocrine tumors may display combined histologies (i.e., SCLC with NSCLC components, and LCNEC with other NSCLC components). In their study, Miyoshi and colleagues included 10 combined LCNEC and 12 combined SCLC. The combined forms clearly indicate the heterogeneity of these tumors and investigating their genetics my offer clues to their potential different cells of origin. However, often the different components of combined forms are tightly intermixed and it may be challenging separating them; in this case sophisticated technology such as laser capture microdissection may be necessary. Unfortunately Miyoshi and colleagues apparently only used coring of tissue blocks and light microscopy, which may not have adequately separated the two components and therefore yielded inconclusive results of this sub-analysis.
The best recognized combined forms of neuroendocrine tumors with non-neuroendocrine tumors in the mixed SCLC-NSCLC histologies, which have been found in a variable number of cases, range from less than 1% to up to 28%. This variability may depend of the availability of tumor tissue and small biopsies do not allow the opportunity to study the tumor in their entirety (13). According to different reports from George et al. and Swanton et al., loss of the tumor suppressor genes, TP53 and RB1, is obligatory in SCLC, and inactivating mutations in the NOTCH family genes occur in 25% of human SCLC (10,14). There has been more comprehensive reports examining LCNEC combined NSCLC or SCLC components. In an older report from Wagner et al. in 2009, loss of heterozygosity (LOH) analysis was used, which showed similar genetic abnormalities in the individual components of the combined SCLC cases (15). In addition, Buys et al. investigated a patient with combined small cell carcinoma with two different NSCLC components. They used a whole genome analysis by tiling-path array comparative genomic hybridization to evaluate the clonal relationship, which resulted in divergent clonal evolution (16). The analysis for combined LCNEC genomic alteration in this article indicated, five in ten LCNECs with other NSCLC components harbored the same key driver mutations in both components. For combined LCNEC, the median number of genetic mutations was 3.5 and 4 in LCNEC and NSCLC component respectively. The median concordance rate between LCNEC and associated NSCLC components was 71% (range, 60% to 100%).
Considering these data, LCNEC combined with NSCLC components may behave and respond more like their NSCLC component, suggesting tumor heterogeneity and early evolution of the combined LCNEC. Because it is suggested that they perform like their NSCLC counterpart, examination of the two separate types of LCNEC combined NSCLC components could provide more insight. Further investigation of the KEAP1/NFE2L2, PIK3CA genes in LCNEC combined squamous cell carcinoma, and the EGFR, KRAS, and NOTCH family genes in LCNEC combined adenocarcinoma may offer a more targeted approach to the treatment of LCNEC. Together with Rekhtman et al. data, the combined mutation profiles could be used as markers to differentiate the different subtypes within LCNECs and advance targeted treatment for patients.
A case study by De Pas et al. in 2011 reported a never smoker patient with LCNEC harboring an activating mutation on the EGFR gene (L747_A755>AT, exon 19). This patient was treated with gefitinib, an approved drug for specific EGFR mutated NSCLC. After 2 months of therapy, the patient showed dramatic response to the treatment, and after 5 months, the patient showed complete response of the lung primary lesions (17). This suggests LCNEC carrying activating EGFR gene mutations could be treated with gefitinib with positive effects.
Because the PI3K/AKT/mTOR pathway was emphasized in Miyoshi and colleagues’ discussion, perhaps the dual PIK3CA/mTOR inhibitor, PI-103, could be a potential targeted therapy for LCNEC carrying a PIK3CA mutation. This drug has been tested and was shown to be active in NSCLC cell lines with activating PIK3CA mutations (18). Patients with PIK3CA and EGFR-mutated lung cancers may not respond to EGFR targeted therapies like gefitinib because of the double mutation. All these factors should be taken into consideration when evaluating the complex molecular profile of LCNEC for targeted therapy selection.
Miyoshi and colleagues have demonstrated the power of next-generation sequencing, and this proposal supports the ongoing movement of genomics delivering a “personalized” treatment approach by assessing the patient’s tumor mutations and selecting the appropriate therapy for an improved response, subsequently increasing overall survival (19-21). Although the study was not a complete, comprehensive investigation of LCNEC, Miyoshi and colleagues provided valuable data in the advancement of LCNEC analysis, diagnosis, and treatment. Because of the distinct molecular characteristics compared to other lung cancer types, LCNEC should be treated as a separate group and not lumped into traditional NSCLC or SCLC treatments. Moreover, smoking patients need to be taken into consideration; it is known that NSCLC patients who have smoked have a 10-fold higher mutational load than never-smokers, and C>A/G>T transversions predominantly occur in NSCLC tobacco users, whereas C>T/G>A transitions most frequently occur in NSCLC never-smokers (22). It seems that LCNEC do not have distinct, targetable genes or mutations (Table 1), similar to other cancers such as pancreatic (23). Nonetheless, possible future studies with more refined methodologies or technologies, such as laser capture microdissection or tissue macrodissection instead of tissue block coring, tumor/normal (blood) pair sequencing, or using single cell or droplet digital PCR, could minimize tumor component/normal cell contamination and dissect tumor heterogeneity. In addition, the authors did not specify the sequencing mean read depth of coverage; a higher read depth of coverage will provide higher accuracy and detection of true somatic mutations. We believe further investigation within a larger and more diverse cohort comparing LCNEC to SCLC and NSCLC would be beneficial. The Cancer Genome Atlas (TCGA) project has only sequenced lung adenocarcinoma and squamous cell carcinoma cases (585 and 504, respectively), but no SCLC cases, mainly because of difficult collection of large, resected material (24). Since LCNEC are treated more like NSCLC based on morphology, perhaps there is potential to obtain more LCNEC surgical samples more easily for genomic analysis, based on this presumption. Furthermore, using RNA sequencing, whole exome or whole genome sequencing would provide a stronger interpretation of the LCNEC genomic landscape.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Shaohua Cui (Department of Pulmonary Medicine, Shanghai Chest Hospital, Shanghai Jiao Tong University, Shanghai, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.11.19). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rekhtman N. Neuroendocrine tumors of the lung: an update. Arch Pathol Lab Med 2010;134:1628-38. [PubMed]
- Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol 2015;10:1243-60. [Crossref] [PubMed]
- Asamura H, Kameya T, Matsuno Y, et al. Neuroendocrine neoplasms of the lung: a prognostic spectrum. J Clin Oncol 2006;24:70-6. [Crossref] [PubMed]
- Battafarano RJ, Fernandez FG, Ritter J, et al. Large cell neuroendocrine carcinoma: an aggressive form of non-small cell lung cancer. J Thorac Cardiovasc Surg 2005;130:166-72. [Crossref] [PubMed]
- Fasano M, Della Corte CM, Papaccio F, et al. Pulmonary Large-Cell Neuroendocrine Carcinoma: From Epidemiology to Therapy. J Thorac Oncol 2015;10:1133-41. [Crossref] [PubMed]
- Niho S, Kenmotsu H, Sekine I, et al. Combination chemotherapy with irinotecan and cisplatin for large-cell neuroendocrine carcinoma of the lung: a multicenter phase II study. J Thorac Oncol 2013;8:980-4. [Crossref] [PubMed]
- Umemura S, Mimaki S, Makinoshima H, et al. Therapeutic priority of the PI3K/AKT/mTOR pathway in small cell lung cancers as revealed by a comprehensive genomic analysis. J Thorac Oncol 2014;9:1324-31. [Crossref] [PubMed]
- Miyoshi T, Umemura S, Matsumura Y, et al. Genomic profiling of large-cell neuroendocrine carcinoma of the lung. Clin Cancer Res 2016; [Epub ahead of print]. [Crossref] [PubMed]
- Rekhtman N, Pietanza MC, Hellmann MD, et al. Next-Generation Sequencing of Pulmonary Large Cell Neuroendocrine Carcinoma Reveals Small Cell Carcinoma-like and Non-Small Cell Carcinoma-like Subsets. Clin Cancer Res 2016;22:3618-29. [Crossref] [PubMed]
- George J, Lim JS, Jang SJ, et al. Comprehensive genomic profiles of small cell lung cancer. Nature 2015;524:47-53. [Crossref] [PubMed]
- Vollbrecht C, Werner R, Walter RF, et al. Mutational analysis of pulmonary tumours with neuroendocrine features using targeted massive parallel sequencing: a comparison of a neglected tumour group. Br J Cancer 2015;113:1704-11. [Crossref] [PubMed]
- Karlsson A, Brunnström H, Lindquist KE, et al. Mutational and gene fusion analyses of primary large cell and large cell neuroendocrine lung cancer. Oncotarget 2015;6:22028-37. [Crossref] [PubMed]
- Nicholson SA, Beasley MB, Brambilla E, et al. Small cell lung carcinoma (SCLC): a clinicopathologic study of 100 cases with surgical specimens. Am J Surg Pathol 2002;26:1184-97. [Crossref] [PubMed]
- Swanton C, Govindan R. Clinical Implications of Genomic Discoveries in Lung Cancer. N Engl J Med 2016;374:1864-73. [Crossref] [PubMed]
- Wagner PL, Kitabayashi N, Chen YT, et al. Combined small cell lung carcinomas: genotypic and immunophenotypic analysis of the separate morphologic components. Am J Clin Pathol 2009;131:376-82. [Crossref] [PubMed]
- Buys TP, Aviel-Ronen S, Waddell TK, et al. Defining genomic alteration boundaries for a combined small cell and non-small cell lung carcinoma. J Thorac Oncol 2009;4:227-39. [Crossref] [PubMed]
- De Pas TM, Giovannini M, Manzotti M, et al. Large-cell neuroendocrine carcinoma of the lung harboring EGFR mutation and responding to gefitinib. J Clin Oncol 2011;29:e819-22. [Crossref] [PubMed]
- Zou ZQ, Zhang XH, Wang F, et al. A novel dual PI3Kalpha/mTOR inhibitor PI-103 with high antitumor activity in non-small cell lung cancer cells. Int J Mol Med 2009;24:97-101. [PubMed]
- Cayer DM, Nazor KL, Schork NJ. Mission critical: the need for proteomics in the era of next-generation sequencing and precision medicine. Hum Mol Genet 2016;25:R182-R189. [Crossref] [PubMed]
- Friedman AA, Letai A, Fisher DE, et al. Precision medicine for cancer with next-generation functional diagnostics. Nat Rev Cancer 2015;15:747-56. [Crossref] [PubMed]
- Jones S, Anagnostou V, Lytle K, et al. Personalized genomic analyses for cancer mutation discovery and interpretation. Sci Transl Med 2015;7:283ra53 [Crossref] [PubMed]
- Govindan R, Ding L, Griffith M, et al. Genomic landscape of non-small cell lung cancer in smokers and never-smokers. Cell 2012;150:1121-34. [Crossref] [PubMed]
- Bryant KL, Mancias JD, Kimmelman AC, et al. KRAS: feeding pancreatic cancer proliferation. Trends Biochem Sci 2014;39:91-100. [Crossref] [PubMed]
- Grossman RL, Heath AP, Ferretti V, et al. Toward a Shared Vision for Cancer Genomic Data. N Engl J Med 2016;375:1109-12. [Crossref] [PubMed]