
Successful removal of a giant hemolymphangioma of the duodenum and the head of pancreas in a 15-year-old male patient with pancreatoduodenectomy: a case report and literature review
Introduction
Hemolymphangioma on duodenum and pancreas is a rare benign cystic tumor. Only a few “single case” reports were found describing hemolymphangioma originated from pancreas in the published literature (1-6), and even fewer cases with tumor affecting also the duodenum. Cystic vascular tumors of the pancreas accounted for 0.1% of all pancreatic tumors (7). There is no distinguishing symptom in patients with hemolymphangioma, until a substantial tumor mass has grown in the abdominal cavity that is usually accompanied with epigastric discomfort/pain. In this case report, we presented a case of hemolymphangioma of duodenum and pancreatic head in a 15-year-old male patient.
Case presentation
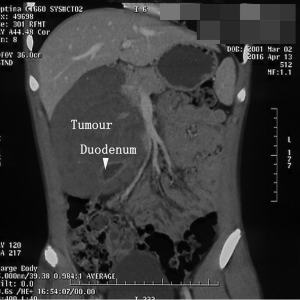
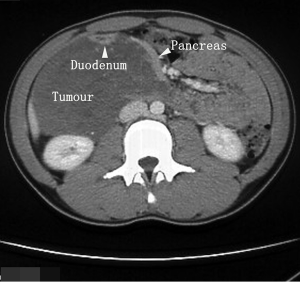
A 15-year-old male patient was hospitalized on the April 26, 2016 who complained of intermittent epigastric pain/dull discomfort for approximately 2 weeks. The patient was generally in good condition with no vomiting, stomachache, or jaundice. Physical examination detected a large abdominal mass in the right upper quarter. Abdominal enhanced computed tomography (CT) showed that the lower end of common bile duct and the duodenum were surrounded and compressed by a polycystic retroperitoneal tumor which had extended to the back of the celiac artery and the head of pancreas (Figures 1,2). Laboratory tests for both carcinoembryonic antigen (CEA) and cancer antigen 19-9 (CA19-9) were negative. During laparotomy, a dark-blue cystic, retroperitoneal tumor was found extending from the descending (vertical) second division of the duodenum to the pancreatic caput and part of pancreas (into the duodenal loop). The tumor infiltrated to the lower part of the common bile duct, pylorus; and tightly adhered to the duodenum and the head of the pancreas. Due to its highly integrated nature with affected organs, a mass of 16×11×8 cm3 along the surface of the duodenum and the neck of the pancreas was removed by pancreatoduodenectomy (PD) (Figure 3). The alimentary continuance was rebuilt with modified Child procedure. The patient had no severe peri-operative complications, and was discharged at 14 days after surgery.
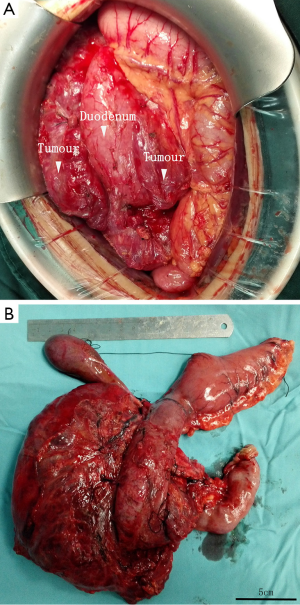
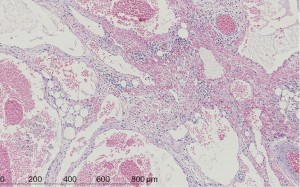
The tumor was polycystic filled with bloody fluid. Under microscope (Figure 4), the tumor showed a tissue consisting of lymphatic and blood vessels with polycystic spaces. Part of the duodenum wall and the parenchyma of the head of pancreas were infiltrated by neoplasia of duodenum wall cells. Histology confirmed the diagnosis as hemolymphangioma with the origin from the wall of duodenum and the pancreas.
Discussion
Hemolymphangioma originated from retroperitoneal organs is a very rare benign lesion that can be caused by congenital malformation of the vascular system. The obstruction of the venolymphatic communication between dysembrioplastic vascular tissue and the systemic circulation could be the major mechanism of tumorigenesis (5). These lesions may also arise from the pancreatic parenchyma (5). Tumors arising from the pancreas are usually large in size with a diameter of more than 10 cm, and can be most commonly found at the caput of pancreas. Generally, the tumor is a large soft cystic neoplasm with a thin or thick wall, having multiple thin septa with various sizes cyst cavities containing bloody fluid and sometimes clear lymphatic fluid. Microscopically, the tumor consists of abnormal lymphatic and blood vessels with polycystic spaces. These cysts have connective septa covered by endothelium.
At early stage patient could be asymptomatic for a long time because of the relative small size of the tumor. At later stage, abdominal pain and awareness of abdominal mass are the most common symptoms that brought patients to the clinic. Other symptoms such as vomiting and nausea may present at a later stage when tumor becomes bigger. Even though it’s very rare, tumor compression of the common bile duct may cause jaundice.
Usually the tumor is non-invasive, however, there is one report of tumor invasion into duodenum by a Japanese group, resulting in internal bleeding and severe anemia (6). Similarly in our case, the tumor was found invasive that it infiltrated into the second and the third part of the duodenum, and tightly adhered to the caput of the pancreas, which made it difficult to distinguish the tumor origin from the duodenum or/and the pancreas.
Diagnosis of hemolymphangioma of the duodenum and the pancreas can be complicated by its rarity and the absence of clinical manifestation. A careful differentiation diagnosis should be considered with some other rare lesions before surgery (7,8). Laboratory tests are frequently normal although slight increases of alkaline phosphatase and gamma-glutamyl transferase were reported (4). Serum CEA and CA19-9 are always within normal limits. Before surgery, imaging techniques such as ultrasonography, abdominal CT, and magnetic resonance imaging are commonly applied for assessment of tumor’s size, relationship between lesions and affected organs, and a clinical diagnosis. Correct differential diagnosis for histological type of the tumor should be achieved peri- or post-operationally, considering with other similar lesions including pseudocyst, lymphangioma, serous mucinous tumors, sarcoma, enteric duplication cyst, and other cystic tumors (8). The final diagnosis should be based on a combination of clinical, radiological, and histopathological findings. In the period of postoperative follow-up, ultrasonography may be sufficient for recurrence assessment.
Surgical treatment including local resection of this tumor is a definitive modality, and the operative principal should be that the tumor be enucleated with the affected section of the related organ excised. In most cases, local resection is usually sufficient due to its benign nature. In our case, however, PD was performed since the tumor was too tightly adhered to the duodenum and the head of the pancreas to be separated. With careful perioperative assessment and correct postoperative management all cases treated with PD in the literature demonstrated good prognosis as it did in our case (9). After a complete excision of the lesion, the chance of recurrence seems extremely low. In this case, the patient is tumor free at the 6-month follow-up. However, a careful and long-term follow-up should always be offered by the surgeon (10).
Conclusions
Hemolymphangioma originated from the pancreas and duodenum in youth and adults is a rare benign tumor, and our case was the first one with the tumor affected the duodenum and pancreas at the same time. Because of its low incidence, awareness of the tumor is important for a correct preoperative and perioperative management. PD could be an option for a complete resection of tumor and affected organ when necessary.
Acknowledgments
Funding: This work was supported by The Capital Health Research and Development of Special (No. 2016-2-2053); Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support, Code: ZYLX201612.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.12.12). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Couinaud Jouan. Hemolymphangioma of the head of the pancreas. Mem Acad Chir (Paris) 1966;92:152-5. [PubMed]
- Couinaud C. A rare tumor of the head of the pancreas. (Hemolymphangioma weighing 1,500 kg.). Presse Med 1967;75:1955-6. [PubMed]
- Montete P, Marmuse JP, Claude R, et al. Hemolymphangioma of the pancreas. J Chir (Paris) 1985;122:659-63. [PubMed]
- Banchini E, Bonati L, Villani LG. A case of hemolymphangioma of the pancreas. Minerva Chir 1987;42:807-13. [PubMed]
- Balderramo DC, Di Tada C, de Ditter AB, et al. Hemolymphangioma of the pancreas: case report and review of the literature. Pancreas 2003;27:197-9. [Crossref] [PubMed]
- Toyoki Y, Hakamada K, Narumi S, et al. A case of invasive hemolymphangioma of the pancreas. World J Gastroenterol 2008;14:2932-4. [Crossref] [PubMed]
- Veerankutty FH, Yeldho V, Tu SA, et al. Hepatoid carcinoma of the pancreas combined with serous cystadenoma: a case report and review of the literature. Hepatobiliary Surg Nutr 2015;4:354-62. [PubMed]
- Le Borgne J, de Calan L, Partensky C. Cystadenomas and cystadenocarcinomas of the pancreas: a multiinstitutional retrospective study of 398 cases. French Surgical Association. Ann Surg 1999;230:152-61. [Crossref] [PubMed]
- Sato N, Tamura T, Minagawa N, et al. Preoperative body mass index-to-prognostic nutritional index ratio predicts pancreatic fistula after pancreaticoduodenectomy. Hepatobiliary Surg Nutr 2016;5:256-62. [Crossref] [PubMed]
- Xu EX. Professor Ho-Seong Han: enjoy being a surgeon. Hepatobiliary Surg Nutr 2016;5:88-9. [PubMed]


