
Toward the clarification of the role of whole-brain radiation therapy for brain metastases from non-small cell lung cancer: a comment about the QUARTZ trial
In the September issue of Lancet, Mulvenna et al. reported the results of the QUARTZ trial, a phase 3 randomized clinical trial between supportive care (SC) only and SC plus whole-brain radiation therapy (WBRT) for patients with brain metastases (BMs) from non-small cell lung cancer (NSCLC), which is not indicated for stereotactic radiosurgery (SRS). The primary outcome measure was quality-adjusted life years (QALYs) and the second outcome measures include overall survival (OS). Mulvenna et al. found no significant difference in QALYs or OS between the two arms, and they concluded that “WBRT provides little additional clinically significant benefit for this patient group”. Mulvenna et al. should be lauded because the QUARTZ trial was the first sufficiently powered randomized clinical trial assessing the role of WBRT in addition to SC. However, we suspect that this categorical statement might be misleading and does not represent important findings which are not described in the report’s abstract. In order to thoroughly consider all of the important information in that report, we need to read it carefully step-by-step.
First, we need to consider the reason why no significant difference in OS or QALYs was observed. Patients with poor performance status were enrolled in the trial; as many as 38% of the patients had a KPS <70. As a result, the median survival time (MST) of each group was as short as 8 weeks. In practice, physicians would not use any treatment routinely except SC for this population. These patients usually suffer from progressive systemic disease, which presents a preferential risk of death or poor systemic status as opposed to intracranial progression. Moreover, it usually takes several weeks in order for the tumor effect of WBRT to translate into symptomatic benefit. It is thus reasonable to consider that in the QUARTZ trial, there was not enough time left, nor enough surviving patients for the quality of life (QOL) benefit to manifest. This finding indicates simply that no routine use of WBRT is necessary for severely ill patients.
We find a similar example in a series of three RCTs of WBRT with/without surgery for patients with a single brain metastasis. In the first trial, published in 1990, Patchell et al. reported that 48 patients were randomized to WBRT with/without surgery and the patients who underwent both surgery and WBRT showed significantly longer survival compared to the WBRT-only patients (9.2 vs. 3.5 mos, P<0.01) (1). In the next trial reported by Noordijk et al. in 1994, the survival benefit of surgery remained significant with a P value of 0.04 (10 vs. 6 mos) (2). However, in the third trial reported by Mintz et al. in 1996, the MST of the surgery + WBRT and WBRT-alone groups was 5.6 and 6.3 mos, respectively, and the difference was no longer significant (3). This discrepancy is explained by the larger inclusion of patients with active systemic cancer in the latter two trials. The patients’ QOL at their terminal state declines day by day. Therefore, OS and QOL are suboptimal endpoints if patients can expect only short survival.
Second, we feel that it should be emphasized more strongly that Mulvenna et al. identified factors associated with better OS after WBRT. Younger age (<60 years) and number of BMs (≥5) were both significantly associated with improved OS after WBRT. In addition, the use of WBRT marginally improved the OS for patients with a good KPS (≥70), absence of extracranial metastasis, controlled primary cancer, or a better graded prognostic assessment (GPA) score. The diagnosis-specific GPA (DS-GPA) is a prognostic index proposed by Sperduto et al. in 2012 (4). For the DS-GPA index, different scoring systems were prepared for six different primary tumor sites. The significant factors used for scoring were the KPS, age, the presence of extracranial metastases, and the number of BMs for NSCLC and small-cell lung cancer (SCLC); tumor subtype, KPS, and age for breast cancer; KPS only for gastro-intestinal (GI) cancer; and KPS and number of BMs for renal cell cancer and melanoma. A score of 4.0 correlates with the best prognosis, whereas 0.0 correlates with the worst prognosis. The MSTs of the NSCLC or SCLC patients with GPA scores of 0.0–1.0, 1.5–2.0, 2.5–3.0 and 3.5–4.0 were 3.0, 5.5, 9.4 and 14.8 months, respectively.
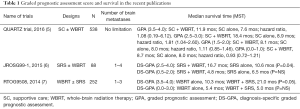
In the QUARTZ trial, the MST of patients with a GPA 2.5–3.0 who received SC + WBRT was 18.4 mos (range, 10.1–23.4 mos) and it was significantly better than the MST of those who received SC alone (MST 8.9 mos, range, 8.0–12.9) with a hazard ratio (HR) of 1.65 [95% confidence interval (CI), 1.04–2.60]. No such survival benefit was observed in the patients with a GPA of 0.0–1.0 or 1.5–2.0 with an HR of 1.11 (0.85–1.46) or 0.93 (0.72–1.21), respectively (Table 1). The lesson here is that the improved intracranial control achieved with WBRT would improve OS in appropriately selected patients. Part of the data supporting this concept for NSCLC patients comes from a secondary analysis of the Japanese Radiation Oncology Study Group (JROSG) 99-1 randomized trial between SRS alone versus SRS + WBRT for 1 to 4 BMs. In the initial analysis of 132 patients in 2006, the authors of that report (8) found no differences in median OS between SRS alone and SRS + WBRT (8.0 vs. 7.5 mos, respectively) but found that WBRT significantly decreased local recurrence from 27% to 11% and distant brain recurrence from 60% to 35%.
Full table
In the secondary analysis in 2015, 88 NSCLC BM patients were extracted from the original JROSG 99-1 trial and post-stratified according to DS-GPA; the analysis revealed that among the subgroup of 88 patients with NSCLC and 1–4 BMs (6), the patients with higher DS-GPA scores (2.5–4.0) had significantly longer median OS when treated with SRS + WBRT compared with SRS alone (16.7 vs. 10.6 mos, HR: 1.92, P=0.04), whereas there was no OS difference among the NSCLC patients with lower DS-GPA scores (P=0.86). This observation implies that improved brain control with WBRT, which has been demonstrated in every SRS + WBRT trial, may translate into an OS advantage specifically among high DS-GPA patients because they do not die as rapidly from extracranial progression.
In this context, we note that Sperduto et al. published in 2014 the results of a secondary analysis of Radiation Therapy Oncology Group (RTOG) 9508, which is an RCT comparing WBRT alone and WBRT + SRS for patients with 1 to 3 BMs (9). The initial report showed that patients had a survival benefit in a post hoc analysis if they had solitary metastasis (7). In the secondary analysis, patients were post-stratified according to the DS-GPA. It is of note that NSCLC became more dominant in the secondary report (84%) than in the initial report (64%). Sperduto et al. found that there was no survival difference between treatments when they analyzed the overall group; however, the patients with a DS-GPA of 3.5–4.0 had better OS when treated with WBRT + SRS (MST 21.0 mos) than with WBRT alone (MST 10.3 mos, P=0.05) (9). Again, these observations imply that the dose-intensification could potentially translate to a survival benefit for patients who can expect a favorable prognosis and could reinforce the potential value of WBRT for enhancing survival.
Third, the finding that WBRT provided survival benefit when the number of BMs was 5 or more should be considered. In this regard, a recent prospective observational study of 1,194 patients with 1–10 BMs treated with SRS alone reported survival results as a function of the number of lesions: the MSTs were 13.9, 10.8, and 10.8 months for patients with 1, 2–4, and 5–10 BMs, leading the report’s authors to conclude that SRS alone is appropriate therapy for patients with 5–10 BMs (10) It should be noted however that that study set an upper limit in the total cumulative tumor volume of BMs of <15 cc, and therefore, the intracranial tumor burden was relatively low even when the number of BMs was as much as 5–10.
It is now considered that the volume, but not the number, of metastases may be the driver in determining patients’ survival. One such example is a retrospective study from the University of Pittsburgh that evaluated the outcomes in 205 patients with ≥4 BMs who underwent SRS. A multivariate analysis revealed the total volume of BMs, rather than the number of metastases, as a significant prognostic factor (11). Although there was no limitation in the cumulative tumor volume in the QUARTZ trial, it is natural to consider that the number of metastases roughly correlates with the total cumulative tumor volume. Therefore, for this population, the administration of WBRT reduces the likelihood of dying from neurologic death.
In conclusion, the QUARTZ trial provided important information toward the clarification of the role of WBRT for patients with BMs from NSCLC. For patients who have (I) a favorable prognosis as determined by GPA; or (II) a large cumulative tumor burden of BMs (i.e., ≥5 metastases), WBRT should be considered to provide a survival benefit conferred by intracranial tumor control. However, for patients expecting only a poor prognosis, the routine use of WBRT is not appropriate.
Acknowledgments
Funding: This work was partially supported by Japan Society for Promotion Science (JSPS) KAKENHI (grant No. 15H04903).
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Ming-Hui Zhang (Department of Medical Oncology, Harbin Medical University Cancer Hospital, Harbin, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.12.71). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 1990;322:494-500. [Crossref] [PubMed]
- Noordijk EM, Vecht CJ, Haaxma-Reiche H, et al. The choice of treatment of single brain metastasis should be based on extracranial tumor activity and age. Int J Radiat Oncol Biol Phys 1994;29:711-7. [Crossref] [PubMed]
- Mintz AH, Kestle J, Rathbone MP, et al. A randomized trial to assess the efficacy of surgery in addition to radiotherapy in patients with a single cerebral metastasis. Cancer 1996;78:1470-6. [Crossref] [PubMed]
- Sperduto PW, Kased N, Roberge D, et al. Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol 2012;30:419-25. [Crossref] [PubMed]
- Mulvenna P, Nankivell M, Barton R, et al. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): results from a phase 3, non-inferiority, randomised trial. Lancet 2016;388:2004-14. [Crossref] [PubMed]
- Aoyama H, Tago M, Shirato H, et al. Stereotactic Radiosurgery With or Without Whole-Brain Radiotherapy for Brain Metastases: Secondary Analysis of the JROSG 99-1 Randomized Clinical Trial. JAMA Oncol 2015;1:457-64. [Crossref] [PubMed]
- Andrews DW, Scott CB, Sperduto PW, et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 2004;363:1665-72. [Crossref] [PubMed]
- Aoyama H, Shirato H, Tago M, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 2006;295:2483-91. [Crossref] [PubMed]
- Sperduto PW, Shanley R, Luo X, et al. Secondary analysis of RTOG 9508, a phase 3 randomized trial of whole-brain radiation therapy versus WBRT plus stereotactic radiosurgery in patients with 1-3 brain metastases; poststratified by the graded prognostic assessment (GPA). Int J Radiat Oncol Biol Phys 2014;90:526-31. [Crossref] [PubMed]
- Yamamoto M, Serizawa T, Shuto T, et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 2014;15:387-95. [Crossref] [PubMed]
- Bhatnagar AK, Flickinger JC, Kondziolka D, et al. Stereotactic radiosurgery for four or more intracranial metastases. Int J Radiat Oncol Biol Phys 2006;64:898-903. [Crossref] [PubMed]


