
Advances on immunotherapy in breast cancer
Introduction
Since its inception in the 1940s (1), chemotherapy has evolved to be a cornerstone in the treatment of many cancers. One of the major disadvantages to chemotherapy has been the considerable toxicity. This has led scientists to discover newer, targeted methods of cancer treatment, such as immunotherapy.
Immunotherapy uses biologic agents to control the signals that dictate cell growth and bolster the natural immune response to malignancy (2). Although breast tumors have historically been deemed immunologically silent, some subtypes have shown interactions with the immune system, the modulation of which may result in effective antitumor activity (3,4). The role of immunotherapy in breast cancer, the mechanism of action of immunotherapeutic agents, and their clinical relevance is discussed in this review article.
Effect of tumor cells on the immune system
In order to prevent autoimmunity, regulatory cells, such as myeloid derived suppressor cells [MDSC] and CD4+CD25hiFoxP3+ T cells [Tregs] exist to suppress self-recognition of T-cells. Tumor cells are able to evade the immune system by differentiating these regulatory cells and increasing their levels (5). In addition to enhancing immunosuppression through Treg cells and MDSCs, tumor cells also escape the immune system by decreasing the levels of antigen presenting cells and increasing the expression of proteins such as anti-apoptotic proteins (survivin, BCL-XL), metastatic proteins (VEGF, MMPs) and proliferation factors (EGFR, c-Myc) (6).
Checkpoint inhibitors, adoptive T cell therapy, and therapeutic vaccines are immunotherapeutic agents that are able to counteract this tumor-induced immunosuppression.
Immunotherapy and breast cancer
Recent studies have identified the presence of tumor infiltrating lymphocytes (TILs) in breast tumor tissue to be a prognostic factor for the pathological complete response (pCR) to neoadjuvant chemotherapy (NAC) (7). With 1,058 patient biopsies, Dushyanthen et al., demonstrated higher post-NAC pCR rates in TIL+ tumors than TIL- tumors (40–42% vs. 3–7%) (7). In this study, more than 60% TILs were present in either the stromal or intratumoral component of the tissue. This response has also been documented in triple negative and HER-2 positive breast cancers.
In addition to the chemotherapeutic agents like taxanes and anthracyclines, some studies have also demonstrated the correlation between TIL and trastuzumab. Loi et al., randomized 232 patients with HER-2 positive disease to either trastuzumab in combination with chemotherapy or chemotherapy alone (8). Results showed a decrease in distant recurrence with each 10% increase in TILs in the combination arm. Salgado et al. also reported similar data with higher pCR rates with TILs higher than 5% and a 3% decrease in an event for every 1% increase in TILs (9). Here the patients were randomized to one of three groups: trastuzumab, lapatinib, or the combination for 6 weeks followed by the addition of weekly paclitaxel for 12 weeks, and 3 cycles of fluorouracil, epirubicin, and cyclophosphamide after surgery. Although the correlation between TILs and pCR was seen in all breast cancer subtypes, the correlation between TILs and disease free endpoints was only seen in triple negative and HER 2 positive subtypes (7). These results have not only identified new prognostic markers for certain breast cancer subtypes but have also highlighted the immunological activity in a cancer that was originally deemed immunologically silent.
Ali et al. conducted one of the largest breast cancer immunotherapy studies where 12,439 breast cancer cells were tested for CD8 and FOX3 immune markers. Breast cancer tissue with CD8+ T cells showed a 28% reduction in hazard of breast cancer-specific mortality in ER-negative tumors (n=2,402), 27% reduction of breast cancer-specific mortality in ER-positive/HER 2-positive tumors (n=483), but no difference in survival in the ER-positive tumors (n=5,956) (10). The study concluded that some subgroups, such as ER-negative tumors and ER-positive/HER 2-positive tumors, could benefit from immune modulation (10).
Checkpoint inhibitors
Immune checkpoints, in the normal physiological state, cause T cell inactivation thus allowing self-tolerance (1). Tumor cells manipulate this mechanism to escape recognition by the immune system (1). Checkpoint inhibitors targeting CTLA-4, PD-1 and PD-L1 prevent this T cell inactivation.
CTLA-4 antibodies have shown mixed responses. Negative results were reported with the use of CTLA-4 antibodies in breast cancer cell lines, TSA, 4T1 and SM1 (11) which are poorly immunogenic. A partial response was however achieved with EMT6 cell line (11). In a small study, tremelimumab, a monoclonal antibody against CTLA-4, in combination with exemestane, an aromatase inhibitor, resulted in stable disease for at least 12 weeks in 42% of patients (12). Further studies showed that responses may be limited to moderately immunogenic cell lines. CTLA-4 blockers have also been studied in combination with radiation and have shown enhanced tumor response at the primary site and growth inhibition at sites outside the radiation field. This study is discussed further under adjunctive immunotherapy.
A large 2016 study involving 111 triple negative breast cancer patients tested the antitumor activity of the PD-1 inhibitor, Pembrolizumab (13). Among the 27 patients that were evaluable, 18.5% demonstrated antitumor activity based on RECIST v1.1 and the median time to response was 17.9 weeks (13). Adams et al. reported promising results with atezolizumab (an anti-PD-L1 inhibitor) in combination with nab-paclitaxel in metastatic triple negative breast cancer (mTNBC). Of the 24 evaluable patients, 7 out of 9 patients with 1 lesion, 6 out of 8 with 2 lesions, and 3 out of 7 with 3 or more lesions showed partial response. A total of 5 patients showed stable disease (14). All patients received ≤3 prior lines of therapy. A clinical trial with atezolizumab plus nab-paclitaxel in the first line setting for mTNBC is ongoing with Progression Free Survival and Overall Survival as primary endpoints.
The combination of CTLA-4 inhibitors and PD-1 inhibitors is currently being tested in various settings such as Nivolumab and Ipilimumab in advanced or metastatic HER2-negative breast cancer (NCT02453620), Durvalumab and Tremelimumab in advanced tumors, including triple negative breast cancer (NCT02527434) and Durvalumab and Tremelimumab in patients with metastatic HER 2-negative breast cancer (NCT02536794). A comprehensive list of all check point inhibitor studies in breast cancer can be found in Table 1.

Full table
Adoptive T cell therapy
Adoptive T cell therapy, also referred to as passive immunization, involves the isolation and ex vivo expansion of tumor specific T cells (14). T cell priming with cancer vaccines (active immunization) prior to isolating the T cells from the patient’s blood has shown great success in expanding the T cell population (15). Adoptive T cell therapy using tumor-infiltrating lymphocytes (TIL), cytotoxic T lymphocytes (CTL), Th cells, Tregs and genetically engineered T cells have shown promising results in melanoma (15). These studies have now been expanded to other cancer types including breast cancer.
The Tumor Vaccine Group at the University of Washington, identified Th1 cells to be superior to CTLs due to their ability to activate antigen-specific effector cells, recruit macrophages and dendritic cells to assist in antigen presentation, directly and indirectly (through cytokines like IL-2) activate CTLs, produce opsonizing antibodies that enhance the uptake of tumor cells into APC, and most importantly initiate epitope spreading (15). In a clinical trial with 16 metastatic breast cancer patients, Domschke et al. identified high levels of tumor-reactive memory T cells in the bone marrow that could have therapeutic effect once re-stimulated ex vivo (16). Tumor-reactive memory T cells in the peripheral blood were induced in 7 out of 16 patients (44%) after the adoptive cell transfer of bone marrow T cells. These patients were deemed responders. Patients with an immunologic response in the peripheral blood had a significantly longer median survival than non-responders (median survival 58.6 vs. 13.6 months; P=0.009). This positive response was only seen in patients without bone metastasis.
As isolation of tumor specific T cells is difficult, genetically engineered or redirected T cells have been of interest in recent times as a form of adoptive T cell therapy. Genes that encode T cell receptors are used to generate tumor specific T cells. This is done using either the alpha or beta chain of the T cell receptor or using chimeric antigen receptors (CAR) (17). CARs are composed of an extracellular domain derived from tumor-specific antibody, linked to an intracellular signaling domain. Plasmid transfection, and mRNA or viral vector transduction are used to introduce these genes into T cells to generate tumor specific T cells. These genetically modified and activated T cells are then reintroduced into the patient’s blood to target specific tumor proteins.
CAR T cell technology in solid tumors is still largely in the preclinical phase with Tumor Associated Antigen (TAA) identification posing the greatest challenge. Neoantigens, which are products of tumor mutations, have been of particular interest as their expression is restricted to only tumor cells (18). In a preclinical study, Tchou et al. tested the CAR technique in triple negative breast cancer tissue. 67% of triple negative breast cancer samples showed overexpression of mesothelin, a glycoprotein (19). An in vitro killing assay was done to assess the cytotoxicity of genetically modified T cells expressing CAR for mesothelin versus a non-transduced T cell. About 31.7% cytotoxicity was observed by the mesoCAR T cells, as opposed to 8.7% cytotoxicity for non-transduced T cells (19). A 2016 study by Song et al. identified the folate receptor alpha (FRα) to be a promising target (20). It was found that FRα specific CAR T cells in the setting of TNBC showed significant tumor growth inhibition in immunodeficient mice bearing MDA-MB-231 tumor xenograft (20).
Most CARs incorporate the T cell receptor CD3ζ signaling chain to cause cytotoxicity (21). A study was conducted where CD28 mediated signaling aimed at T cell proliferation and IL-2 production was incorporated to study the benefit of complimentary CAR T cells (22). These cells were then engineered to co express ErbB2- and MUC1 and tested in breast cancer. Results showed efficient proliferation of T cells and destruction of ErbB2 positive tumor cells and confirmed the benefit of the dual target approach using CAR T cells. A unique approach of combining PD-1 inhibitors with CAR T cells to enhance the therapeutic outcome is also being tested using mouse models.
A list of ongoing CAR T cell clinical trials in breast cancer can be found in Table 2.
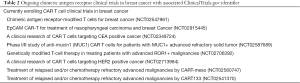
Full table
Vaccines
The success of vaccines for viral diseases has provided the frame work for developing vaccines for cancers. Cancer has been associated with T cell deletion and T cell anergy causing defective memory (23). The aim of vaccines has been to prepare naïve T cells and transform the existing memory T cells into effective combatants of the tumor cells. In order to prepare naïve T cells, tumor antigens have to be presented using MHC class 1 and 2 (23). With dendritic cells being the most efficient antigen presenting cells, many clinical trials have employed plasmacytoid dendritic cell vaccines and conventional dendritic cell vaccines (23). Plasmacytoid dendritic cells (pDCs), in addition to being antigen presenting cells, can also alter the tumor microenvironment and have shown IFN-1 dependent tumor regression through TLR7 ligand and IFN-1 independent tumor regression through TLR9 ligation (23).
Although the mouse models have shown positive results using activated pDC in the setting of melanoma and sarcoma tumors, dendritic cell involvement in human cells did not show a favorable outcome. T cell and dendritic cell infiltration into human breast cancer cells was assessed in 152 patients with invasive non-metastatic breast cancer using DC migration markers (MIP-3a/CCL20, MIP-3b/CCL19, and 6Ckine/CCL21), CD1a (T cell), CD3 (T cell), CD68 (Macrophages), CD123 (plasmacytoid Dendritic cells), CD207/Langerin (immature dendritic cells), and CD208/DC-LAMP (mature dendritic) expression (24). CD 123 infiltration in the tumor was associated with shorter overall survival (93% versus 58% at 60 months) and relapse free survival (90% vs. 37% at 60 months) (24). CD208/DC-LAMP positive DC (56%) and CD3 positive T cells (82%) strongly correlated with lymph node involvement (24). The mechanism behind this negative effect on human breast cancer cells was studied using 60 human breast cancer biopsies where increased tumor associated pDC (TApDC) were seen in aggressive cancer cells. TApDC expressed very low levels of interferon alpha which caused FOX3p+ Treg expansion leading to the immune tolerance (25). With interferon alpha being a strong immunomodulator and FOX3p+ Treg having immunosuppressive qualities, the negative response in human breast cancer cells was justified.
Knowing the poor immunogenic quality of breast cancer cells, Abe et al. identified a subpopulation of the 4T1 mouse breast cancer cell line, 4T1-Sapporo (4T1-S), which showed immunogenic properties when used to vaccinate mice (26). The mice were vaccinated with 4T1-S prior to receiving injections with the same cell line and showed significant enlargement of draining lymph nodes and increased frequencies of activated CD8 T cells (26). This mouse model helped in identifying the benefit of cancer vaccines after enhancement of the immunogenic properties of breast cancer cells.
In a clinical trial, 22 patients with Stage 4 HER2/neu positive breast cancer received HER2/neu T-helper peptide-based vaccine in addition to Trastuzumab which resulted in epitope spreading within HER2/neu and other proteins. The T cell response was also inversely proportional to the level of transforming growth factor beta (a promoter of tumor growth and metastasis) (27). A phase 1–2 clinical trial was conducted to assess the clinical benefit of E75 vaccine (a human leukocyte antigen (HLA) A2/A3-restricted HER2/neu (HER2) peptide, and granulocyte-macrophage colony-stimulating factor) on patients with HER2/neu positive breast cancer that either were lymph node positive or were high risk. Only HLA-A2/A3(+) patients were vaccinated. Out of 195, 182 patients were evaluable. Disease free survival was 94.3% in the vaccinated group and 86.8% in the control group (P=0.08) (28). A booster dose was also initiated and none of the patients who received the booster dose had a recurrence (28). The scope for booster treatments due to its low toxicity profile has shown a promising future for cancer vaccines.
Certain cytokines have proven to have synergy with cancer vaccines. Low levels of TNF- alpha production has been seen in breast cancer patients in comparison to healthy individuals (29). It has been found that DC infiltration is dependent on TNF alpha production and low levels of TNF alpha impair their ability to recruit naïve T cells (29). Other studies have shown an increase in the apoptosis of tumor cells with the co administration of TNF alpha and DC (29). It has also been reported that DCs which have been activated by pro-inflammatory cytokines produce TNF-alpha, leading to apoptosis in breast cancer cells (29).
Adjunctive immunotherapy
Although most chemotherapies cause immunosuppression, some drugs help in increasing the tumor immunogenicity and can be coupled with other immunomodulators, such as immunostimulatory cytokines, to achieve the maximum antitumor effect. Doxorubicin, for example, upregulates MHC class 1 and Fas expression and increases sensitivity to Cytotoxic T Lymphocyte killing (30). Other anthracyclines and platinum salts release high-mobility group box 1 (HMGB1) and adenosine triphosphate (ATP) which result in the release of IL-1β and activation of Toll ligand receptor 4 (TLR4) on the infiltrating dendritic cell (31). The activated TLR4 then stimulates innate immunity while IL-1β takes part in cell proliferation, differentiation and apoptosis (31). Taxanes have shown to increase the lymphocyte infiltration when given neoadjuvantly and also increase the Th1 associated cytokines when given in the metastatic setting (30).
IL-18 is one immunostimulatory cytokine that has demonstrated the ability to enhance the production of IFN-γ by the T cells and natural killer cells, act synergistically with IL-12 to induce IFN-γ production, augment the cytolytic activity of natural killer cells and CTLs, promote the differentiation of activated CD4 T cells into helper effector cells, and stimulate Th1 immune responses (32,33). IL-18 is able to augment the activity of phase specific chemotherapeutic drugs that are unable to target resistant tumor cells in a non-vulnerable phase of the cell cycle (34).
Divino et al. used an intrahepatic tumor model of metastatic breast cancer to test the effects of intravenous administration of recombinant adenoviral vector expressing the murine IL-12. Prolongation of long term survival of IL-12 treated animals, with complete tumor rejection in 40% of the animals was reported (35). This study clearly showed the benefit of immunostimulatory cytokines in metastatic breast cancer.
In 2014, a study was conducted on 90 post mastectomy triple negative breast cancer patients where cytokine induced killer (CIK) cell infusion was used in conjunction with chemotherapy (36). CIK adjuvant therapy showed an increase in disease free survival in patients with pathologic grade 3 disease, and increase in overall survival in N1, N2, N3, IIB, III TNM stages as well as pathologic grade 3 disease (36).
Radiation has also shown some immunomodulatory effects causing upregulation of the expression of MHC and the radiation induced tumor epitopes. In the first preclinical study to test Radiation with CTLA-4 inhibitor (Ipilimumab) in a metastatic 4T1 breast cancer model, the inhibitor alone did not show regression of tumor due to poor immunogenicity of breast cancer cells but the combination showed tumor shrinkage and inhibition of lung metastasis (37). Ruocco et al. also demonstrated data showing very little effect in poor immunogenic tumors with anti-CTLA-4 antibodies but reversal of tumor elicited MHC Class 1 dependent arrest with radiation and immunomodulator combination (38).
Ongoing Phase 1 and 2 clinical trials combining radiation and immunotherapy are described in Table 3.

Full table
Conclusions
Immunotherapy has shown a clear but modest benefit as monotherapy and combination therapy in highly immunogenic tumors. Through preliminary data, these agents have also demonstrated some scope in breast cancer and other poorly immunogenic tumors, although with some conflicting results. Identifying methods of initiating interactions between tumor cells and the immune system and augmenting the few existing interactions will determine the success of these agents in breast cancer and other similar cancers.
Acknowledgments
Authors would like to thank Marin Xavier, MD for her support, guidance and expertise.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Marin Feldman Xavier) for the series “Advances on Clinical Immunotherapy” published in Translational Cancer Research. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.01.09). The series “Advances on Clinical Immunotherapy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Weir GM, Liwski RS, Mansour M. Immune modulation by chemotherapy or immunotherapy to enhance cancer vaccines. Cancers (Basel) 2011;3:3114-42. [Crossref] [PubMed]
- Caspi RR. Immunotherapy of autoimmunity and cancer: the penalty for success. Nat Rev Immunol 2008;8:970-6. [Crossref] [PubMed]
- Cimino-Mathews A, Ye X, Meeker A, et al. Metastatic triple-negative breast cancers at first relapse have fewer tumor-infiltrating lymphocytes than their matched primary breast tumors: a pilot study. Hum Pathol 2013;44:2055-63. [Crossref] [PubMed]
- García-Teijido P, Cabal ML, Fernández IP, et al. Tumor-Infiltrating Lymphocytes in Triple Negative Breast Cancer: The Future of Immune Targeting. Clin Med Insights Oncol 2016;10:31-9. [Crossref] [PubMed]
- Lindau D, Gielen P, Kroesen M, et al. The immunosuppressive tumour network: myeloid-derived suppressor cells, regulatory T cells and natural killer T cells. Immunology 2013;138:105-15. [Crossref] [PubMed]
- Xiong A, Yang Z, Shen Y, et al. Transcription Factor STAT3 as a Novel Molecular Target for Cancer Prevention. Cancers (Basel) 2014;6:926-57. [Crossref] [PubMed]
- Dushyanthen S, Beavis PA, Savas P, et al. Relevance of tumor-infiltrating lymphocytes in breast cancer. BMC Med 2015;13:202. [Crossref] [PubMed]
- Loi S, Michiels S, Salgado R, et al. Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann Oncol 2014;25:1544-50. [Crossref] [PubMed]
- Salgado R, Denkert C, Campbell C, et al. Tumor-Infiltrating Lymphocytes and Associations With Pathological Complete Response and Event-Free Survival in HER2-Positive Early-Stage Breast Cancer Treated With Lapatinib and Trastuzumab: A Secondary Analysis of the NeoALTTO Trial. JAMA Oncol 2015;1:448-54. [Crossref] [PubMed]
- Ali HR, Provenzano E, Dawson SJ, et al. Association between CD8+ T-cell infiltration and breast cancer survival in 12,439 patients. Ann Oncol 2014;25:1536-43. [Crossref] [PubMed]
- Grosso JF, Jure-Kunkel MN. CTLA-4 blockade in tumor models: an overview of preclinical and translational research. Cancer Immun 2013;13:5. [PubMed]
- McArthur HL, Diab A, Page DB, et al. A Pilot Study of Preoperative Single-Dose Ipilimumab and/or Cryoablation in Women with Early-Stage Breast Cancer with Comprehensive Immune Profiling. Clin Cancer Res 2016;22:5729-37. [Crossref] [PubMed]
- Nanda R, Chow LQ, Dees EC, et al. Pembrolizumab in Patients With Advanced Triple-Negative Breast Cancer: Phase Ib KEYNOTE-012 Study. J Clin Oncol 2016;34:2460-7. [Crossref] [PubMed]
- Adams S, Diamond JR, Hamilton EP, et al. Phase Ib trial of atezolizumab in combination with nab-paclitaxel in patients with metastatic triple-negative breast cancer (mTNBC). J Clin Oncol 2016;34:abstr 1009.
Adoptive T Cell Therapy Tumor Vaccine Group - Domschke C, Ge Y, Bernhardt I, et al. Long-term survival after adoptive bone marrow T cell therapy of advanced metastasized breast cancer: follow-up analysis of a clinical pilot trial. Cancer Immunol Immunother 2013;62:1053-60. [Crossref] [PubMed]
- Zhang H, Ye ZL, Yuan ZG, et al. New Strategies for the Treatment of Solid Tumors with CAR-T Cells. Int J Biol Sci 2016;12:718-29. [Crossref] [PubMed]
- Newick K, Moon E, Albelda SM. Chimeric antigen receptor T-cell therapy for solid tumors. Mol Ther Oncolytics 2016;3:16006. [Crossref] [PubMed]
- Tchou J, Wang LC, Selven B, et al. Mesothelin, a novel immunotherapy target for triple negative breast cancer. Breast Cancer Res Treat 2012;133:799-804. [Crossref] [PubMed]
- Song DG, Ye Q, Poussin M, et al. Effective adoptive immunotherapy of triple-negative breast cancer by folate receptor-alpha redirected CAR T cells is influenced by surface antigen expression level. J Hematol Oncol 2016;9:56. [Crossref] [PubMed]
- Bridgeman JS, Ladell K, Sheard VE, et al. CD3ζ-based chimeric antigen receptors mediate T cell activation via cis- and trans-signalling mechanisms: implications for optimization of receptor structure for adoptive cell therapy. Clin Exp Immunol 2014;175:258-67. [Crossref] [PubMed]
- Wilkie S, van Schalkwyk MC, Hobbs S, et al. Dual targeting of ErbB2 and MUC1 in breast cancer using chimeric antigen receptors engineered to provide complementary signaling. J Clin Immunol 2012;32:1059-70. [Crossref] [PubMed]
- Mac Keon S, Ruiz MS, Gazzaniga S, et al. Dendritic cell-based vaccination in cancer: therapeutic implications emerging from murine models. Front Immunol 2015;6:243. [Crossref] [PubMed]
- Treilleux I, Blay JY, Bendriss-Vermare N, et al. Dendritic cell infiltration and prognosis of early stage breast cancer. Clin Cancer Res 2004;10:7466-74. [Crossref] [PubMed]
- Sisirak V, Faget J, Gobert M, et al. Impaired IFN-α production by plasmacytoid dendritic cells favors regulatory T-cell expansion that may contribute to breast cancer progression. Cancer Res 2012;72:5188-97. [Crossref] [PubMed]
- Abe H, Wada H, Baghdadi M, et al. Identification of a highly immunogenic mouse breast cancer sub cell line, 4T1-S. Hum Cell 2016;29:58-66. [Crossref] [PubMed]
- Disis ML, Wallace DR, Gooley TA, et al. Concurrent trastuzumab and HER2/neu-specific vaccination in patients with metastatic breast cancer. J Clin Oncol 2009;27:4685-92. [Crossref] [PubMed]
- Mittendorf EA, Clifton GT, Holmes JP, et al. Clinical trial results of the HER-2/neu (E75) vaccine to prevent breast cancer recurrence in high-risk patients: from US Military Cancer Institute Clinical Trials Group Study I-01 and I-02. Cancer 2012;118:2594-602. [Crossref] [PubMed]
- Rao VS, Dyer CE, Jameel JK, et al. Potential prognostic and therapeutic roles for cytokines in breast cancer Oncol Rep 2006;15:179-85. (Review). [PubMed]
- Alagkiozidis I, Facciabene A, Carpenito C, et al. Increased immunogenicity of surviving tumor cells enables cooperation between liposomal doxorubicin and IL-18. J Transl Med 2009;7:104. [Crossref] [PubMed]
- Apetoh L, Ghiringhelli F, Tesniere A, et al. The interaction between HMGB1 and TLR4 dictates the outcome of anticancer chemotherapy and radiotherapy. Immunol Rev 2007;220:47-59. [Crossref] [PubMed]
- Robertson MJ, Kirkwood JM, Logan TF, et al. A dose-escalation study of recombinant human interleukin-18 using two different schedules of administration in patients with cancer. Clin Cancer Res 2008;14:3462-9. [Crossref] [PubMed]
- Robertson MJ, Mier JW, Logan T, et al. Clinical and biological effects of recombinant human interleukin-18 administered by intravenous infusion to patients with advanced cancer. Clin Cancer Res 2006;12:4265-73. [Crossref] [PubMed]
- Alagkiozidis I, Facciabene A, Tsiatas M, et al. Time-dependent cytotoxic drugs selectively cooperate with IL-18 for cancer chemo-immunotherapy. J Transl Med 2011;9:77. [Crossref] [PubMed]
- Divino CM, Chen SH, Yang W, et al. Anti-tumor immunity induced by interleukin-12 gene therapy in a metastatic model of breast cancer is mediated by natural killer cells. Breast Cancer Res Treat 2000;60:129-34. [Crossref] [PubMed]
- Pan K, Guan XX, Li YQ, et al. Clinical activity of adjuvant cytokine-induced killer cell immunotherapy in patients with post-mastectomy triple-negative breast cancer. Clin Cancer Res 2014;20:3003-11. [Crossref] [PubMed]
- Dewan MZ, Galloway AE, Kawashima N, et al. Fractionated but not single-dose radiotherapy induces an immune-mediated abscopal effect when combined with anti-CTLA-4 antibody. Clin Cancer Res 2009;15:5379-88. [Crossref] [PubMed]
- Ruocco MG, Pilones KA, Kawashima N, et al. Suppressing T cell motility induced by anti-CTLA-4 monotherapy improves antitumor effects. J Clin Invest 2012;122:3718-30. [Crossref] [PubMed]


