
Unraveling the hurdles in the development of HER2-targeted agents for metastatic gastro-esophageal cancer patients
Gastric cancer (GC) is one of the most lethal cancers, representing the third leading cause of cancer-related deaths worldwide (1). In fact, more than two thirds of the cases of GC present metastatic widespread at diagnosis. Despite the efforts done in Western countries for improving more radical approaches, such as perioperative strategies (2) and adjuvant chemo-radiation (3), 50% of resected GC patients will inevitably develop metastatic disease. Systemic chemotherapy remains the mainstay therapeutic option for these patients, with objective responses ranging between 30–40% and overall survival (OS) rates of 12 months at most (4). Considering this discouraging panorama, the identification of the biologic role of the epidermal growth factor receptor 2 (ERBB2 or HER2) and the promising results of clinical trials with HER2-directed agents among breast cancer patients, highlighted the possibility of further categorizing other tumor subtypes in search of similar therapeutic targets (5). Thus, GC emerged as the ideal candidate for evaluating trastuzumab, a monoclonal HER2-antibody, as part of the armamentarium against the 20% of GC patients where HER2 overexpression is described as a frequent molecular aberration (6).
In 2010, a phase 3 randomized study assessing trastuzumab in combination with a doublet of fluoropyrimidines-cisplatinum chemotherapy (ToGA trial, NCT01041404), met its primary endpoint of improving OS rates among HER2-positive GC patients (7). Following the results of this study, trastuzumab was licensed in combination with chemotherapy as an optimal first-line therapy for this subset of GC patients, and in parallel, led to the establishment of an algorithm-based diagnosis using a companion tool of combined immunohistochemistry (IHC) plus fluorescent in situ hybridization (FISH). To date, HER2-positivity is defined with an IHC 3+ or IHC 2+/FISH HER2:CEP17 ratio ≥2 (8), since these patients whose tumors presented higher levels of HER2 protein expression (IHC 2+ or 3+) were the ones who achieved the greatest benefit from treatment with cisplatinum-fluoropyrimidine-trastuzumab (OS of 16 months). However, no other HER2 biological compounds have been approved for this molecularly selected population of HER2-positive GC patients. Over the last decade, other HER2-directed agents have been also evaluated, such as lapatinib, a small molecule acting as a dual inhibitor of the epidermal growth factor receptor (EGFR) and HER2 tyrosine kinases (2,9), and trastuzumab emtansine—formerly known as T-DM1, an antibody-drug conjugate comprised by trastuzumab linked to a tubulin inhibitor (10). Despite promising preclinical data and encouraging initial results, three statistically powered studies have failed to demonstrate their primary endpoints of improved efficacy when assessed versus standard chemotherapy.
The TRIO-013/LOGIC study (NCT00680901) evaluated in previously untreated HER2-positive GC patients the efficacy of adding lapatinib to capecitabine and oxaliplatin (CAPOX). Median OS in the experimental arm was 12.2 and 10.5 months in the CAPOX arm, which was not significantly different (hazard ratio of 0.91; 95% confidence interval: 0.73 to 1.12). The exploratory pre-planned analysis showed differences in the lapatinib arm depending on the geographical region and the age of patients, but no clear correlation between the degree of HER2 overexpression and OS was detected (9). Furthermore, a phase III study evaluated lapatinib versus paclitaxel monotherapy as second-line strategy in a HER2-positive Asian population (TyTAN trial, NCT00486954). In the case of this study, lapatinib plus paclitaxel showed activity among patients with IHC 3+/FISH-positive tumors, although did not significantly improve OS in the intention-to-treat population (2). Of note, both trials assessing lapatinib enrolled GC considered as HER2-positive only based on FISH-positive results (HER2:CEP17 ratio ≥2) performed in a local or central laboratory. The later analysis of HER2 protein overexpression demonstrated that a high proportion of these HER2-amplified patients presented in reality low protein levels, with 35% of patients presenting IHC of 0 or 1+ in the TyTAN study. The GATSBY study (NCT01641939) evaluated T-DM1 against taxanes, either paclitaxel or docetaxel, for previously treated with at least a platinum-fluoropyrimidine agent HER2-positive GC patients. Patients were considered eligible based on centrally tested primary or metastatic tumors, by standard IHC/ISH criteria (IHC 2+ and ISH-positive results or IHC 3+ regardless of ISH status) (10). Again, this study also failed to show any OS superiority, and neither clinical nor biomarker subgroups were identified for benefitting from the experimental arm. Noteworthy, most of the enrolled patients were selected after having previously received trastuzumab and on the basis of the results of archival GC HER2 status at any disease stage. Taking into account the evidence of clonal evolution and changes in the molecular profile across the innate tumoral evolution (11,12), it seems evident that HER2 expression might have been altered or lost during the progression (13). In addition, it is well recognized the heterogeneous and/or focal expression of HER2 protein over the polarized membrane of the gastric cell, which may in turn have limited the degree of activity of the immune-conjugate [e.g., reduced HER2 recognition by the trastuzumab-antibody portion of T-DM1, therefore decreased cleavage of the linker and emtansine molecules, limiting the subsequent bystander effect (14)]. Furthermore, there is increasing evidence of several mechanisms that may confer acquired resistance to HER2-guided therapies, such as co-amplification of HER3/EGFR, heterodimerization of HER2-HER3 or HER3 mutations, co-amplification of cMET or FGFR autocrine loops among others (15). Further characterization of these resistance mechanisms will certainly help in better understanding why T-DM1 may have failed in this promising setting. Table 1 depicts the main characteristics of these mentioned clinical trials testing HER2 agents in GC. The disappointing results of these studies reflect, in the background, a poor pre-selection strategy for finding the most suitable candidates for participating in these trials, which may have obscured the real HER2-positive GC population that could have benefitted from the HER2-blockade therapy.
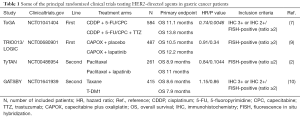
Full table
In the article by Press et al. (16) published in Molecular Cancer Therapeutics, the authors report the results of a retrospective study of the HER2 status (gene amplification and protein overexpression) among the gastro-esophageal cancer patients evaluated for enrolment in the TRIO-013/LOGIC trial. The aim of this analysis was to explore and assess the potential correlation between levels of HER2 gene amplification and protein expression levels with responsiveness to the experimental arm combining CAPOX plus lapatinib. As mentioned before, patients could be enrolled into the TRIO-013/LOGIC trial according to local determination of HER2-amplification, in which case required central confirmation for inclusion in the primary efficacy population. In this study, five hundred forty-five patients were accrued (4.4% esophageal, 8.3% gastro-esophageal junction, 87.3% gastric), and 89% were centrally confirmed for FISH-positivity. Of note, the concordance between central and local HER2 FISH testing was 83%. Although the study did not meet its primary endpoint, Asian and younger patients (<60 years) presented an improvement in progression-free survival rates (PFS). One may wonder, why these differential results in only this subset of patients? Interestingly, among patients analyzed in this dataset, there were no cases IHC3+/FISH-negative, while some of the initially considered HER2-amplified patients by FISH did not express high levels of HER2 protein as expected. Precisely, among the 81 cases included with HER2-amplification by FISH but only IH 0/1+ for HER2 protein, PFS was not statistically significant (HR =1.12, P value =0.65), as also happened in the TyTAN study. This detailed analysis highlights that the efficacy to HER2 blockade seems to correlate better with high HER2 gene amplification, but because this translates into higher HER2 protein expression levels: 91% of patients who had the highest HER2 protein distribution (IHC3+) presented FISH ratios with >10-fold HER2 gene amplification. The inclusion of HER2-amplified but not HER2-overexpressed patients may account as one of the reasons why the TRIO-013/LOGIC trial was unsuccessful. Also, this retrospective analysis draws the attention to the fact that there is certain lack of concordance between the HER2 testing results performed in local versus central laboratories, and a marked inter-pathologist variability associated to the partially subjective interpretation of the IHC results. These discrepancies are even more remarkable when comparing the IHC assays (agreement less than 58%) compared to the FISH techniques (agreement of 87%).
These results are in light with the findings previously reported by Gomez-Martin et al. (17), who were among the first in demonstrating that the level of HER gene amplification predicts sensitivity to trastuzumab-based therapy among GC patients. Noteworthy, it seems that this gene amplification-efficacy correlation is tightly related to the subjacent HER2 overexpression, suggesting that the protein levels may serve as a stronger predictive biomarker of response. The long-term gained experience in testing HER2 by IHC should help us to improve this HER2 assessment and interpretation, in order to ensure that the GC patients who can really benefit are identified and accordingly treated. Only by learning from our previous mistakes we will be able to widen the horizon towards new and precise assessments methods. With this regards, it has to be considered that GC exhibits unique immunostaining characteristics compared with other tumors, such as breast cancer: a remarkable intratumoral heterogeneity and the possibility of incomplete staining of GC cells due to the innate gland-forming structure of these tumors. These particularities may explain why some GC patients are considered positive by IHC, whilst they only present basolateral or lateral staining, instead of complete membrane involvement. This trait does not only account for HER expression (18), but also for other molecular alterations described in GC, such as FGFR2 (19) or PIK3CA (12). In light of these results, new approaches have been developed in order to improve the assessment of HER2 protein overexpression (20). It is in this context where the previously mentioned proteomic analysis should begin to be considered (21).
The assessment of HER2 status in GC remains a controversial field, where recent efforts for integrating the different molecular classifications have added another layer of complexity (22-24). Novel combinations evaluating promising therapeutic options, such as the double blockade of the HER2/HER3 pathway by combining trastuzumab and pertuzumab are ongoing (JACOB study—NCT01774786—in metastatic setting and INNOVATION study—NCT02205047—in the neoadjuvant setting), but new strategies are certainly warranted to further improve the selection of those patients more likely to respond to this anti-HER2 strategies. Rational integration of the innate intratumoral heterogeneity of GC tumors seems mandatory, in order to design accurate pre-selection strategies for ensuring the success of future biomarker-driven trials. Only by adopting a multidisciplinary approach, combining a deeper understanding of the tumor biology, the increasing genomic data and the development of accurate and reproducible HER2 tests, we will be able to guide the successful development of new targeted agents for GC patients (25).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Hongcheng Zhu (Department of Radiation Oncology, the First Affiliated Hospital of Nanjing Medical University, Nanjing, China).
Conflicts of Interest: J Tabernero has participated in advisory activities for Amgen, Bayer, Boehringer Ingelheim, Celgene, Chugai, Eli Lilly, MSD, Merck Serono, Novartis, Pfizer, Roche, Sanofi, Symphogen, Taiho and Takeda. C Hierro and M Alsina have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- International Agency for Research on Cancer (IARC) WHOW. GLOBOCAN 2012, Section of Cancer Surveillance. Available online: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx
- Satoh T, Xu RH, Chung HC, et al. Lapatinib plus paclitaxel versus paclitaxel alone in the second-line treatment of HER2-amplified advanced gastric cancer in Asian populations: TyTAN--a randomized, phase III study. J Clin Oncol 2014;32:2039-49. [Crossref] [PubMed]
- Macdonald JS, Smalley SR, Benedetti J, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med 2001;345:725-30. [Crossref] [PubMed]
- Okines AF, Norman AR, McCloud P, et al. Meta-analysis of the REAL-2 and ML17032 trials: evaluating capecitabine-based combination chemotherapy and infused 5-fluorouracil-based combination chemotherapy for the treatment of advanced oesophago-gastric cancer. Ann Oncol 2009;20:1529-34. [Crossref] [PubMed]
- Hudis CA. Trastuzumab--mechanism of action and use in clinical practice. N Engl J Med 2007;357:39-51. [Crossref] [PubMed]
- Gravalos C, Jimeno A. HER2 in gastric cancer: a new prognostic factor and a novel therapeutic target. Ann Oncol 2008;19:1523-9. [Crossref] [PubMed]
- Bang YJ, Van Cutsem E, Feyereislova A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 2010;376:687-97. [Crossref] [PubMed]
- Bartley AN, Washington MK, Colasacco C, et al. HER2 Testing and Clinical Decision Making in Gastroesophageal Adenocarcinoma: Guideline From the College of American Pathologists, American Society for Clinical Pathology, and the American Society of Clinical Oncology. J Clin Oncol 2017;35:446-64. [Crossref] [PubMed]
- Hecht JR, Bang YJ, Qin SK, et al. Lapatinib in Combination With Capecitabine Plus Oxaliplatin in Human Epidermal Growth Factor Receptor 2-Positive Advanced or Metastatic Gastric, Esophageal, or Gastroesophageal Adenocarcinoma:TRIO-013/LOGiC--A Randomized Phase III Trial. J Clin Oncol 2016;34:443-51. [Crossref] [PubMed]
- Thuss-Patience PC, Shah MA, Ohtsu A, et al. Trastuzumab emtansine versus taxane use for previously treated HER2-positive locally advanced or metastatic gastric or gastro-oesophageal junction adenocarcinoma (GATSBY): an international randomised, open-label, adaptive, phase 2/3 study. Lancet Oncol 2017;18:640-53. [Crossref] [PubMed]
- Burrell RA, McGranahan N, Bartek J, et al. The causes and consequences of genetic heterogeneity in cancer evolution. Nature 2013;501:338-45. [Crossref] [PubMed]
- Alsina M, Gullo I, Carneiro F. Intratumoral heterogeneity in gastric cancer: a new challenge to face. Ann Oncol 2017;28:912-3. [Crossref] [PubMed]
- Pietrantonio F, Caporale M, Morano F, et al. HER2 loss in HER2-positive gastric or gastroesophageal cancer after trastuzumab therapy: Implication for further clinical research. Int J Cancer 2016;139:2859-64. [Crossref] [PubMed]
- Sau S, Alsaab HO, Kashaw SK, et al. Advances in antibody-drug conjugates: A new era of targeted cancer therapy. Drug Discov Today 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Shi H, Zhang W, Zhi Q, et al. Lapatinib resistance in HER2+ cancers: latest findings and new concepts on molecular mechanisms. Tumour Biol 2016; [Epub ahead of print]. [Crossref] [PubMed]
- Press MF, Ellis CE, Gagnon RC, et al. HER2 Status in Advanced or Metastatic Gastric, Esophageal, or Gastroesophageal Adenocarcinoma for Entry to the TRIO-013/LOGiC Trial of Lapatinib. Mol Cancer Ther 2017;16:228-38. [Crossref] [PubMed]
- Gomez-Martin C, Plaza JC, Pazo-Cid R, et al. Level of HER2 gene amplification predicts response and overall survival in HER2-positive advanced gastric cancer treated with trastuzumab. J Clin Oncol 2013;31:4445-52. [Crossref] [PubMed]
- Stahl P, Seeschaaf C, Lebok P, et al. Heterogeneity of amplification of HER2, EGFR, CCND1 and MYC in gastric cancer. BMC Gastroenterol 2015;15:7. [Crossref] [PubMed]
- Hierro C, Alsina M, Sanchez M, et al. Targeting the fibroblast growth factor receptor 2 in gastric cancer: promise or pitfall? Ann Oncol 2017;28:1207-16. [Crossref] [PubMed]
- Nuciforo P, Radosevic-Robin N, Ng T, et al. Quantification of HER family receptors in breast cancer. Breast Cancer Res 2015;17:53. [Crossref] [PubMed]
- An E, Ock CY, Kim TY, et al. Quantitative proteomic analysis of HER2 expression in the selection of gastric cancer patients for trastuzumab treatment. Ann Oncol 2017;28:110-5. [PubMed]
- Lei Z, Tan IB, Das K, et al. Identification of molecular subtypes of gastric cancer with different responses to PI3-kinase inhibitors and 5-fluorouracil. Gastroenterology 2013;145:554-65. [Crossref] [PubMed]
- Cancer Genome Atlas Research Network. Comprehensive molecular characterization of gastric adenocarcinoma. Nature 2014;513:202-9. [Crossref] [PubMed]
- Cristescu R, Lee J, Nebozhyn M, et al. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat Med 2015;21:449-56. [Crossref] [PubMed]
- Nuciforo PG. The search for simplicity: is this compatible with precision medicine? Ann Oncol 2017;28:10-2. [PubMed]


