
Stereotactic conformal radiation therapy in the treatment of benign and low-grade brain tumors
Benign and low-grade brain tumors are a heterogeneous group characterized by long-term survivorship and the potential for late effects from tumor and treatment. These tumors account for one-third to one-half of all central nervous system tumors in pediatrics (1).
The primary treatment strategy of benign and low-grade brain tumors is surgical resection (2). However, gross total resection is not always possible and alternative treatment methods including chemotherapy and/or radiation therapy (RT) are often recommended for recurrence or progression after subtotal resection (3). RT is an effective non-surgical treatment for pediatric low-grade brain tumors with 5-year progression-free survival estimates exceeding 80% (4). However, the long-term sequelae of RT include neurocognitive (NC) and neuroendocrine (NE) dysfunction, secondary malignancies, and vascular events as a result of normal tissue toxicity (5). New RT techniques to improve the conformality and precision of the radiation dose deposited, and thus minimize radiation exposure to the normal tissues. This has led to a reduction in the long-term effects of radiation in this population (6).
Types of RT used for pediatric benign and low-grade brain tumors
Reducing the dose deposited in normal tissue should be a primary goal when administering RT (7). Historically, conventional RT has been used in management with rates of local control between 75% and 90% (8). However, large volumes were treated due to the technologic uncertainties of tumor and radiation dose localization, often resulting in significant morbidity (9). With the advent of computed tomography, magnetic resonance imaging, and three-dimensional RT planning and delivery, disease control and functional outcomes improved (4,5).
These advances allowed improved target localization and focused, conformal radiation treatments. Stereotactic RT, a technique using highly precise localization methods, is particularly promising within pediatric brain tumors due the ability to minimize the amount of normal tissue treated without compromising tumor control (1,4). This technique can use head fixation devices and modifications to standard linear accelerators (1). The accuracy and precision of stereotactic RT allows for a smaller margin of normal tissue to receive the prescribed dose and reduction of the entry doses per beam.
In general, high-precision conformal techniques, such as stereotactic radiosurgery and radiotherapy, intensity-modulated RT, and particle (i.e., proton) therapy, have been incorporated into routine clinical practice without data supported by randomized controlled trials (6). Various smaller prospective trials have evaluated the efficacy of stereotactic RT for childhood brain tumors considered to be well-controlled with conventional RT and demonstrated excellent local control (1,10).
Long-term NC and NE dysfunction after intracranial RT
As above, the long-term sequelae of RT in the brain of young children include NC and NE dysfunction, as well as vascular events and secondary malignancies. These vary in severity depending on the age of the child, the radiation dose, and the size and location of the radiation field (8). Of note, a large percent of these patients have baseline NC and NE dysfunction prior to RT (5,8).
NC dysfunction in pediatric patients treated with RT is well established (9). This can present as impairment of global cognitive functioning [intelligence quotient (IQ)], memory and attention, executive function, and psychomotor skills (11). The mechanisms of RT-induced NC dysfunction involve white matter injury, necrosis, inflammation, angiogenesis, and cell death to progenitor cells, inflammatory and stromal cells, and the vasculature (12). Several additional factors that impact intelligence in this treated population include age, sex, presence of hydrocephalus, number of surgical interventions, and dose-volumes to the brain. Severe mental impairment has historically been noted in 17% to 40% of patients (9). For patients treated with stereotactic conformal RT, more than one third of patients showed a >10% decline in full-scale IQ (FSIQ). Younger age and RT to the left temporal lobe may be predictive of NC decline (8). These factors should be considered when treating this population.
NE dysfunction primarily involves hormonal deficits caused by disturbance of the hypothalamic-pituitary-adrenal (HPA) axis. This affects secretion of growth hormone, gonadotropins, TSH and adrenocorticotropic hormone (13). As radiation is a local therapy, tumor location plays a critical role in identifying patients at high risk for NE dysfunction; those with centrally located tumors are at higher risk of HPA disturbance (5,14) and RT-associated impairment of the HPA that can result in life-long hormone replacement therapy (14). The average time to pituitary dysfunction is 5 years but the actuarial risk continues over the patient’s lifetime.
Randomized phase 3 trial—stereotactic conformal RT vs. conventional RT
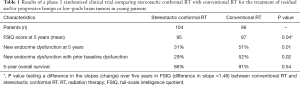
Jalali et al. conducted a phase 3 randomized clinical trial that compared stereotactic conformal RT with conventional RT for the treatment of residual and/or progressive benign or low-grade brain tumors in young patients (6). Their primary end points were incidence and magnitude of NC and NE dysfunctions; assessments included Wechsler intelligence score chart, Wechsler memory scale, anxiety scores, depression scores, growth metrics, puberty metrics (sexual maturity rating and follicle-stimulating hormone and luteinizing hormone levels), thyroid performance (T4 levels and clinical hypothyroidism), and steroid levels (basal cortisol and clinical hypocortisolism). The secondary end point was overall survival. A total of 200 patients with low-grade and benign residual and/or progressive brain tumors were randomized to stereotactic conformal RT or conventional RT. Patient characteristics were well matched with respect to demographic variables, tumor factors, and clinical characteristics at baseline.
Mean FSIQ scores of patients in the stereotactic conformal RT arm were either stable or showed an improvement over 5 years compared with patients in the conventional RT arm (difference in slope =1.48; P=0.4). Mean FSIQ scores in the conventional RT arm initially improved in the first 6 months and then gradually declined. NC improvement was more pronounced in performance quotient and memory quotient in the stereotactic conformal RT arm than conventional RT arm. In the verbal quotient (VQ) subdomain, mean scores showed a progressive decline in both arms over 5 years (difference in slope =0.976; P=0.24), although this rate of decline was slower in the stereotactic conformal RT arm than in the conventional RT arm. Subgroup analysis found that stereotactic conformal RT was superior to conventional RT in patients with supratentorial tumors, patients 16 years or younger, patients at a higher baseline neurological performance scale score, and moderate-to-severe hydrocephalus. When compared with baseline, at 5 years, there was reduction in anxiety and depression scores in both stereotactic conformal RT and conventional RT arms, but these reductions were not statistically significant. The cumulative percentage incidence of NE dysfunction over 5 years was significantly lower in the stereotactic conformal RT arm than in the conventional RT arm (difference in slope =0.04; P=0.01) with an absolute difference of 21 percentage points at 5 years. The 5-year tumor control rate for the stereotactic conformal RT arm was 93% [95% confidence interval (CI), 84–98%] versus 92% (95% CI, 83–96%) for the conventional RT arm (P=0.49). For the entire cohort of 200 patients, 5-year rate of overall survival in the stereotactic conformal RT arm was 86% (95% CI, 76–92%) versus 91% (95% CI, 83–95%) for the conventional RT arm (P=0.54). These results are highlighted in the table (Table 1).
Full table
Impact of the study
Radiation treatment for benign and low-grade brain tumors was undergoing rapid technologic advances at the time of this study. Major centers were shifting to more advanced RT techniques, including the implementation of highly precise stereotactic conformal RT, which may minimize the volume of normal tissue receiving high radiation doses (15). This technologic shift occurred based on the proposed dosimetric advantages of stereotactic conformal RT alone, and in the absence of high level evidence demonstrating an improvement in the important endpoints of quality of life, disease control, or survival. As margins become tighter, and dose more conformal, the trade-off between acceptable disease control and the sparing of normal tissue tightens. Jalali et al. showed less NC and NE dysfunction in the stereotactic conformal RT arm compared to conventional RT arm (6) with no difference in local control or overall survival. For the first time, this study provides level 1 evidence (16) demonstrating that with modern technology we can achieve tight radiation margins around the tumor (and thus spare critical normal tissues reducing the risk of developing late radiation-associated toxicities) without sacrificing disease control in this young population. While the use of stereotactic conformal RT requires certain instrumentation that is not always available in radiation oncology centers across the world (17), this study establishes a need for stereotactic conformal RT because of the long-term survivorship in these patients. Referrals to centers that have the ability to deliver these conformal RT are highly recommended.
Next steps
In looking beyond stereotactic conformal RT, other strategies exist or are being developed to further prevent or minimize long-term RT toxicity in patients with benign or low-grade brain tumors. The use of particle therapy and optimal target delineation with better imaging can also be exploited to achieve better functional NC and NE outcomes (11). These efforts are motivated in part by modeling studies that associated an increasing number of radiation fields with a higher risk of secondary cancers; this is a function of the high integral of low-dose radiation exposure to normal tissue when using multiple fields (7).
The physical advantages of particle therapy with protons or heavy ions could be exploited to substantially reduce the radiation dose to normal tissues outside the tumor volume (18). In a retrospective study of 32 pediatric patients with low-grade gliomas (LGG) treated with proton therapy (PT), 12 patients had NC assessment and did not show any significant declines in the FSIQ at a median NC testing interval of 4.5 years. However, subgroup analysis indicated some significant decline in NC outcomes for young children (<7 years of age) and those with significant dose to the left temporal lobe or hippocampus (19). In a phase 2 study of PT for medulloblastoma, there was a decline in FSIQ of 1.5 points per year (95% CI, 0.9–2.1) after a median follow-up of 5.2 years, which was mainly attributable to a decline in processing speed and verbal comprehension. However, perception reasoning and working memory were not affected. A significant decline in FSIQ was again seen in young children (<8 years of age) (20). Furthermore, PT is associated with a lower risk of secondary tumors due to a lower integral dose (7). The initial reports of modern RT techniques and PT are encouraging and deserve continued investigation, particularly now that one is emboldened by this phase III randomized controlled trial demonstrating how improved tumor localization while minimizing dose to normal tissues matters in these benign and low-grade brain tumors.
The use of functional imaging and tractography for RT planning in brain tumors also hold promise in reducing dose to critical areas within the brain. Functional imaging enables mapping of eloquent locations, such as the motor cortex, Broca’s area, Wernicke’s area, and the visual cortex, using various stimuli. In a feasibility study of four patients with low-grade glioma, functional MRI (fMRI)-based 3D conformal planning allowed for a reduction in approximately 50% of radiation dose to the superior and inferior temporal gyrus and the lingual gyrus (21). Tractography is a 3D modeling technique used to visually represent neural tracts using diffusion-weighted imaging data. In one study that evaluated the use of fMRI and tractography in stereotactic radiosurgery of patients with arteriovenous malformation (AVM), astrocytoma, brain metastasis, and hemangioma, there was a significant reduction in dose administered to functional structures and fiber tracts (22). The frequency of motor complications after radiosurgery integrated with corticospinal tractography in 24 patients with AVMs involving the basal ganglia and thalamus was significantly lower than in a historical cohort of 28 patients without tractography integration (4.2% vs. 17.9%; P=0.02) (23). Tractography is increasingly being integrated into radiosurgery planning for benign brain conditions.
Assessing the impact of these advancing technologies on pediatric brain tumor patients using the critical endpoints of quality of life and disease and survival outcomes in a prospective, high-level fashion, as has been done by Jalali et al., is the ideal (6). Although the impacts on disease endpoints are unclear, the potential improvement on NC and NE outcomes cannot be understated.
Conclusions
The study by Jalali et al. provides a high level of evidence in favor of tumor and radiation dose localization with highly conformal RT in the treatment of recurrent or progressive benign and low-grade brain tumors. They demonstrate that improved tumor and dose localization in this population results in an important benefit with treatment-associated adverse effects and quality of life without a detriment in tumor control.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Xianxin Qiu (Shanghai Proton and Heavy Ion Center (SPHIC), a.k.a. the Proton and Heavy Ion Center of Fudan University Shanghai Cancer Center (FUSCC), Shanghai, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.09.35). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Marcus KJ, Goumnerova L, Billett AL, et al. Stereotactic radiotherapy for localized low-grade gliomas in children: final results of a prospective trial. Int J Radiat Oncol Biol Phys 2005;61:374-9. [Crossref] [PubMed]
- Jakola AS, Myrmel KS, Kloster R, et al. Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. JAMA 2012;308:1881-8. [Crossref] [PubMed]
- Wisoff JH, Sanford RA, Heier LA, et al. Primary neurosurgery for pediatric low-grade gliomas: a prospective multi-institutional study from the Children's Oncology Group. Neurosurgery 2011;68:1548-54; discussion 1554-5. [Crossref] [PubMed]
- Merchant TE, Kun LE, Wu S, et al. Phase II trial of conformal radiation therapy for pediatric low-grade glioma. J Clin Oncol 2009;27:3598-604. [Crossref] [PubMed]
- Merchant TE, Conklin HM, Wu S, et al. Late effects of conformal radiation therapy for pediatric patients with low-grade glioma: prospective evaluation of cognitive, endocrine, and hearing deficits. J Clin Oncol 2009;27:3691-7. [Crossref] [PubMed]
- Jalali R, Gupta T, Goda JS, et al. Efficacy of Stereotactic Conformal Radiotherapy vs Conventional Radiotherapy on Benign and Low-Grade Brain Tumors: A Randomized Clinical Trial. JAMA Oncol 2017;3:1368-76. [Crossref] [PubMed]
- Winkfield KM, Niemierko A, Bussiere MR, et al. Modeling intracranial second tumor risk and estimates of clinical toxicity with various radiation therapy techniques for patients with pituitary adenoma. Technol Cancer Res Treat 2011;10:243-51. [Crossref] [PubMed]
- Jalali R, Mallick I, Dutta D, et al. Factors influencing neurocognitive outcomes in young patients with benign and low-grade brain tumors treated with stereotactic conformal radiotherapy. Int J Radiat Oncol Biol Phys 2010;77:974-9. [Crossref] [PubMed]
- Bloom HJ, Glees J, Bell J, et al. The treatment and long-term prognosis of children with intracranial tumors: a study of 610 cases, 1950-1981. Int J Radiat Oncol Biol Phys 1990;18:723-45. [Crossref] [PubMed]
- Jalali R, Budrukkar A, Sarin R, et al. High precision conformal radiotherapy employing conservative margins in childhood benign and low-grade brain tumours. Radiother Oncol 2005;74:37-44. [Crossref] [PubMed]
- Ajithkumar T, Price S, Horan G, et al. Prevention of radiotherapy-induced neurocognitive dysfunction in survivors of paediatric brain tumours: the potential role of modern imaging and radiotherapy techniques. Lancet Oncol 2017;18:e91-e100. [Crossref] [PubMed]
- Attia A, Page BR, Lesser GJ, et al. Treatment of radiation-induced cognitive decline. Curr Treat Options Oncol 2014;15:539-50. [Crossref] [PubMed]
- Müller HL, Merchant TE, Puget S, et al. New outlook on the diagnosis, treatment and follow-up of childhood-onset craniopharyngioma. Nat Rev Endocrinol 2017;13:299-312. [Crossref] [PubMed]
- Loeffler JS, Shih HA. Radiation therapy in the management of pituitary adenomas. J Clin Endocrinol Metab 2011;96:1992-2003. [Crossref] [PubMed]
- Mendenhall NP, Fitzgerald TJ. Conventional Radiation Therapy Compared With Stereotactic Conformal Therapy-A Rare and Laudable Randomized Trial. JAMA Oncol 2017;3:1376-7. [Crossref] [PubMed]
- Burns PB, Rohrich RJ, Chung KC. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg 2011;128:305-10. [Crossref] [PubMed]
- Grau C, Defourny N, Malicki J, et al. Radiotherapy equipment and departments in the European countries: final results from the ESTRO-HERO survey. Radiother Oncol 2014;112:155-64. [Crossref] [PubMed]
- Gondi V, Yock TI, Mehta MP. Proton therapy for paediatric CNS tumours - improving treatment-related outcomes. Nat Rev Neurol 2016;12:334-45. [Crossref] [PubMed]
- Greenberger BA, Pulsifer MB, Ebb DH, et al. Clinical outcomes and late endocrine, neurocognitive, and visual profiles of proton radiation for pediatric low-grade gliomas. Int J Radiat Oncol Biol Phys 2014;89:1060-8. [Crossref] [PubMed]
- Yock TI, Yeap BY, Ebb DH, et al. Long-term toxic effects of proton radiotherapy for paediatric medulloblastoma: a phase 2 single-arm study. Lancet Oncol 2016;17:287-98. [Crossref] [PubMed]
- Kovács A, Tóth L, Glavák C, et al. Integrating functional MRI information into radiotherapy planning of CNS tumors-early experiences. Pathol Oncol Res 2011;17:207-17. [Crossref] [PubMed]
- Pantelis E, Papadakis N, Verigos K, et al. Integration of functional MRI and white matter tractography in stereotactic radiosurgery clinical practice. Int J Radiat Oncol Biol Phys 2010;78:257-67. [Crossref] [PubMed]
- Koga T, Shin M, Maruyama K, et al. Integration of corticospinal tractography reduces motor complications after radiosurgery. Int J Radiat Oncol Biol Phys 2012;83:129-33. [Crossref] [PubMed]


