
New hope for advanced nasopharyngeal cancer—an Epstein-Barr virus-driven endemic malignancy?
It is well-known that the nasopharyngeal cancer (NPC) is highly endemic with the high incidences in Southern China and Southeast Asia (1). The undifferentiated histological subtype is the most common in endemic regions, which is highly sensitive to radiation therapy and chemotherapy. Intensity-modulated radiation therapy as the most commonly employed technique in the contemporary era is the mainstay of treatment for previously untreated early-stage NPC while concurrent chemoradiation is indicated in locoregionally advanced disease (2-5). That said, about 30% of patients develop relapse either as locoregional recurrence or distant metastasis despite intensive aggressive treatment (6).
Doublet chemotherapy is the standard 1st line treatment of choice for unresectable recurrent/metastatic disease. Zhang et al. demonstrated the superiority of gemcitabine over 5-FU, in combination with cisplatin as 1st line treatment, which led to an improvement of median overall survival (OS) from 20.9 to 29.1 months (7). Progression-free survival (PFS) also improved from 5.6 to 7.0 months. Nevertheless, the evidence of chemotherapy as subsequent systemic therapy following failure to 1st line chemotherapy is less well-defined. Single agent without platinum, e.g., gemcitabine, taxane, capecitabine and metronomic cyclophosphamide, is an also acceptable option for heavily pretreated patients (8-11). Targeted therapy including anti-EGFR (gefitinib and cetuximab), anti-VEGF/VEGFR (axitinib), multi-kinase tyrosine kinase inhibitor (sorafenib and sunitinib) and Akt inhibitor were also evaluated in numerous phase II trials (12-15). Unfortunately, none of them produced promising results. Significant toxicity leading to fatal hemorrhagic events is observed with use of anti-VEGF/VEGFR agent.
Immuno-oncology has become a novel exploratory strategy for head and neck cancers. In fact, recurrence of squamous cell carcinoma of the head and neck are facilitated by evasion from the host immune system (16), This is mediated to a certain extent by robust expression of the programmed death ligands (mainly PD-L1 and PD-L2) of the T-cell—suppressive immune-checkpoint receptor programmed death 1 (PD-1) (17-20). The recent CHECKMATE-141 and KEYNOTE-040 study using nivolumab and pembrolizumab respectively as subsequent therapy after failure to 1st line platinum-based chemotherapy demonstrated improved objective response and survival compared to standard chemotherapy in head and neck squamous cell carcinoma (HNSCC) (21,22). These two drugs have been recently approved by the Food and Drug Administration (FDA) of the United States for recurrent or metastatic HNSCC that has continued to progress despite standard-of-care treatment with chemotherapy.
A new hope with immunotherapy using immune checkpoint inhibitors is also approaching NPC. Hsu et al. has recently reported the safety and anti-tumor activity of a multi-cohort phase Ib study (KEYNOTE-028) using pembrolizumab in 20 different types of advanced solid malignancies including locally advanced or metastatic NPC. Within the NPC cohort, the eligibility criteria include locally advanced or metastatic PD-L1-positive NPC for which prior standard therapy was ineffective, did not exist, or was not considered appropriate (23). Pembrolizumab 10 mg/kg was given every 2 weeks to eligible patients for up to 24 months or until progressive disease, unacceptable toxicity, patient refusal or investigator decision to discontinue it. Objective tumor response was assessed by computed tomography or magnetic resonance imaging every 8 weeks for the first 6 months followed by every 12 weeks afterwards. The primary endpoint is objective response rate while secondary endpoints comprised PFS, OS, duration of response and safety of tolerability. PD-L1 positivity, confirmed at a central laboratory was defined as membranous staining on 1% or more of a modified proportion score or interface pattern on either an archived formalin-fixed paraffin-embedded tumor sample or a newly obtained sample using a custom-made laboratory-developed prototype immunohistochemical assay.
Out of 47 and 44 screened and evaluable patients respectively, PD-L1 positivity was found in 41 patients (93.2%). Finally, 27 patients were treated with pembrolizumab and evaluated for treatment outcomes. Three patients completed 2-year pembrolizumab treatment and two remained on study at the time of publication. Twenty-two discontinued from study treatment following progressive disease while the remaining patients stopped the treatment because of adverse events, physician decision and patient withdrawal. Among the 27 PD-L1—positive patients recruited in this cohort, 25 (92.5%) were PD-L1 positive in the tumor only, 1 (3.7%) was positive in the tumor and stroma, and 1 (3.7%) was PD-L1 negative in the tumor but positive in the stroma.
Objective response was observed in 7 (25.9%) patients, all had partial responses after pembrolizumab. An additional 14 (51.9%) patients demonstrated stable disease. Intriguingly, about one-third of patients enjoyed long-lasting disease control for at least 6 months. After a median follow-up duration of 20 months, the median time to response, duration of response, duration of stable disease were 1.9, 17.1 and 5.6 months respectively. The median PFS (investigator) and median PFS (central review) was 6.5 and 2.3 months respectively. A clinicopathological correlation demonstrated that all 7 patients with partial response had PD-L1 expression in the tumour cells only. Grade ≥3 adverse events occurred in 8 (29.6%) patients including pneumonitis, proteinuria, anemia, hepatitis, etc. One (3.7%) patient died of sepsis. Immune-related adverse events were observed in 10 (37.0%) patients including hepatitis (14.8%), hypothyroidism (7.4%) and pneumonitis (7.4%).
Besides the caveats inherent to all phase IB studies, there are also some limitations pertaining to this study. It may be better if a mandatory new biopsy of one of the target lesions for PD-L1 expression can be obtained before the study begins, instead of just retrieving the archive specimen. This will give a more conclusive evidence demonstrating the correlation of PD-L1 expression of the tumors and the surrounding stroma with the treatment outcomes. Besides, different histological subtypes of NPC were included in this study. It will be interesting to know if a particular subtype especially the undifferentiated and the keratinizing differentiated subtypes prevalent in endemic areas derives a differential response to pembrolizumab. Furthermore, the dose of pembrolizumab in this multi-cohort study is higher than the currently recommended dose by the FDA, which may account for the slightly higher treatment-related and immune-related adverse events.
Following this study, the recently announced phase II multi-center study on nivolumab for recurrent/metastatic NPC after failure to at least 1 line of platinum-based chemotherapy demonstrated an objective response rate 19% and disease control rate of 52% in a total of 45 patients recruited in this study (24). Eight (18.2%) had grade ≥3 adverse events including 1 who died of sepsis. Interestingly, all patients who enjoyed partial response had >5% of PD-L1 expression and 1 patient with complete response at the primary tumor and partial response in the lung revealed the highest PD-L1 expression (80%). On the other hand, majority of patients with progressive disease had <1% PD-L1 expression in the tumors.
The prognostic role of PD-L1 expression at different levels in the tumor cells and the surrounding inflammatory cells in NPC remains to be deciphered. At least five Phase II randomized and non-randomized trials are ongoing to investigate the safety and efficacy of immune check inhibitors, including nivolumab, pembrolizumab, PDR001 and avelumab in the recurrent/metastatic setting after prior exposure to platinum-based chemotherapy (NCT02339558, NCT02611960 and NCT02605967, NCT02875613) (Table 1). Very likely their promising results, if any, will prompt the commencement of phase III randomized-controlled trials which compare to standard chemotherapy regimens. More importantly, it is hoped that potential predictive and prognostic biomarkers following immunotherapy can be identified for NPC.
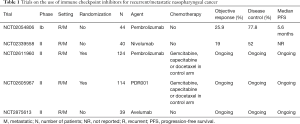
Full table
Apart from the use of immune checkpoint inhibitor, other immunotherapeutic approaches have been comprehensively evaluated in NPC. They primarily involve Epstein-Barr virus (EBV)-directed adoptive and active immunotherapy, administration of antibodies and induction of EBV lytic cycle, etc. Clinical trials examined the use of CD8 + CTLs through autologous transfer or vaccination with dendritic cells or peptides in patients with recurrent/metastatic NPC have been conducted since two decades ago (25-27). The results demonstrated favorable LMP2 specific immune responses as well as modest and durable tumor regression in some patients. Other approaches include T-cell therapy with chemotherapy and the use of novel adenovirus vector for more optimal T-cell expansion have also been reported (26,28). An updated result of the use of adenovirus vector for T-cell adoptive therapy either pre-emptively in at-risk patients with no or minimal residual disease or therapeutically in patients with active recurrent or metastatic disease showed that the median PFS and OS were 5.5 and 38.1 months, respectively (29). It was further noted that disease stabilization in patients with active disease was significantly associated with the functional and phenotypic composition of in vitro-expanded T-cell immunotherapy. These included a higher proportion of effector CD8 positive T-cells and increased number of EBV-specific T-cells with broader antigen specificity.
In summary, this seems to be an epoch-making shift of management paradigm for recurrent/metastatic NPC in the era of immunotherapy. Before this comes true, much efforts have to be paid in future ongoing studies to prove the efficacy and safety of immunotherapy for this intractable disease.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor San-Gang Wu, MD (Department of Radiation Oncology, Xiamen Cancer Center, The First Affiliated Hospital of Xiamen University, Xiamen, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.12.25). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chang ET, Adami HO. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev 2006;15:1765-77. [Crossref] [PubMed]
- Lee AW, Ma BB, Ng WT, et al. Management of nasopharyngeal carcinoma: current practice and future perspective. J Clin Oncol 2015;33:3356-64. [Crossref] [PubMed]
- Peng G, Wang T, Yang KY, et al. A prospective, randomized study comparing outcomes and toxicities of intensity-modulated radiotherapy vs. conventional two-dimensional radiotherapy for the treatment of nasopharyngeal carcinoma. Radiother Oncol 2012;104:286-93. [Crossref] [PubMed]
- Lai SZ, Li WF, Chen L, et al. How does intensity-modulated radiotherapy versus conventional two-dimensional radiotherapy influence the treatment results in nasopharyngeal carcinoma patients? Int J Radiat Oncol Biol Phys 2011;80:661-8. [Crossref] [PubMed]
- Blanchard P, Lee A, Marguet SMAC-NPC Collaborative Group, et al. Chemotherapy and radiotherapy in nasopharyngeal carcinoma: an update of the MAC-NPC meta-analysis. Lancet Oncol 2015;16:645-55. [Crossref] [PubMed]
- Lee AW, Sze WM, Au JS, et al. Treatment results for nasopharyngeal carcinoma in the modern era: the HongKong experience. Int J Radiat Oncol Biol Phys 2005;61:1107-16. [Crossref] [PubMed]
- Zhang L, Huang Y, Hong S, et al. Gemcitabine plus cisplatin versus fluorouracil plus cisplatin in recurrent or metastatic nasopharyngeal carcinoma: a multicentre, randomised, open-label, phase 3 trial. Lancet 2016;388:1883-92. [Crossref] [PubMed]
- Zhang L, Zhang Y, Huang PY, et al. Phase II clinical study of gemcitabine in the treatment of patients with advancednasopharyngeal carcinoma after the failure of platinum-based chemotherapy. Cancer Chemother Pharmacol 2008;61:33-8. [Crossref] [PubMed]
- Chua D, Wei WI, Sham JS, et al. Capecitabine monotherapy for recurrent and metastatic nasopharyngeal cancer. Jpn J Clin Oncol 2008;38:244-9. [Crossref] [PubMed]
- Ngeow J, Lim WT, Leong SS, et al. Docetaxel is effective in heavily pretreated patients with disseminated nasopharyngeal carcinoma. Ann Oncol 2011;22:718-22. [Crossref] [PubMed]
- Lee VH, Kwong DL, Lam KO, et al. Metronomic oral cyclosphosphamide as third-line systemic treatment or beyond in patients with inoperable locoregionally advanced recurrent or metastatic nasopharyngeal carcinoma. Medicine (Baltimore) 2017;96:e6518 [Crossref] [PubMed]
- Chua DT, Wei WI, Wong MP, et al. Phase II study of gefitinib for the treatment of recurrent and metastatic nasopharyngeal carcinoma. Head Neck 2008;30:863-7. [Crossref] [PubMed]
- Chan AT, Hsu MM, Goh BC, et al. Multicenter, phase II study of cetuximab in combination with carboplatin in patients with recurrent or metastatic nasopharyngeal carcinoma. J Clin Oncol 2005;23:3568-76. [Crossref] [PubMed]
- Hui EP, Ma BB, King AD, et al. Hemorrhagic complications in a phase II study of sunitinib in patients of nasopharyngeal carcinoma who has previously received high-dose radiation. Ann Oncol 2011;22:1280-7. [Crossref] [PubMed]
- Ma B, Hui EP, King A, et al. A phase II study of patients with metastatic or locoregionally recurrent nasopharyngeal carcinoma and evaluation of plasma Epstein-Barr virus DNA as a biomarker of efficacy. Cancer Chemother Pharmacol 2008;62:59-64. [Crossref] [PubMed]
- Ferris RL. Immunology and immunotherapy of head and neck cancer. J Clin Oncol 2015;33:3293-304. [Crossref] [PubMed]
- Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell 2015;27:450-61. [Crossref] [PubMed]
- Li J, Jie HB, Lei Y, et al. PD-1/SHP-2 inhibits Tc1/Th1 phenotypic responses and the activation of T cells in the tumor microenvironment. Cancer Res 2015;75:508-18. [Crossref] [PubMed]
- Badoual C, Hans S, Merillon N, et al. PD-1-expressing tumor-infiltrating T cells are a favorable prognostic biomarker in HPV-associated head and neck cancer. Cancer Res 2013;73:128-38. [Crossref] [PubMed]
- Concha-Benavente F, Srivastava RM, Trivedi S, et al. Identification of the cellintrinsic and -extrinsic pathways downstream of EGFR and IFNγ that induce PD-L1 expression in head and neck cancer. Cancer Res 2016;76:1031-43. [Crossref] [PubMed]
- Ferris RL, Blumenschein G Jr, Fayette J, et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med 2016;375:1856-67. [Crossref] [PubMed]
- Cohen EE, Harrington KJ, Le Tourneau C, et al. Pembrolizuamb (pembro) vs standard of care (SOC) for recurrent or metastatic head and neck squamous cell carcinoma (R/M HNSCC): Phase 3 KEYNOT-040 trial. Ann Oncol 2017;28:v605-49. [Crossref]
- Hsu C, Lee SH, Ejadi S, et al. Safety and antitumor activity of pembrolizumab in patients with programmed death-ligand 1–positive nasopharyngeal carcinoma: results of the KEYNOTE-028 study. J Clin Oncol 2017;35:4050-6. [Crossref] [PubMed]
- Ma BB, Goh BC, Lim WT, et al. Multicenter phase II study of nivolumab in previously treated patients with recurrent and metastatic non-keratinizing nasopharyngeal carcinoma - Mayo clinic Phase 2 Consortium P2C-MN026, NCI9742, NCT02339558. Cancer Res 2017;77:Abstract nr CT076.
- Chua D, Huang J, Zheng B, et al. Adoptive transfer of autologous Epstein-Barr virus-specific cytotoxic T cells for nasopharyngeal carcinoma. Int J Cancer 2001;94:73-80. [Crossref] [PubMed]
- Smith C, Tsang J, Beagley L, et al. Effective treatment of metastatic forms of Epstein-Barr virus-associated nasopharyngeal carcinoma with a novel adenovirus-based adoptive immunotherapy. Cancer Res 2012;72:1116-25. [Crossref] [PubMed]
- Hui EP, Taylor GS, Jia H, et al. Phase I trial of recombinant modified vaccinia ankara encoding Epstein-Barr viral tumor antigens in nasopharyngeal carcinoma patients. Cancer Res 2013;73:1676-88. [Crossref] [PubMed]
- Chia WK, Wang WW, Teo M, et al. A phase II study evaluating the safety and efficacy of an adenovirus-DeltaLMP1-LMP2 transduced dendritic cell vaccine in patients with advanced metastatic nasopharyngeal carcinoma. Ann Oncol 2012;23:997-1005. [Crossref] [PubMed]
- Smith C, Lee V, Schuessler A, et al. Pre-emptive and therapeutic adoptive immunotherapy for nasopharyngeal carcinoma: phenotypic and effector function of T cells impact on clinical response. Oncoimmunology 2017;6:e1273311 [Crossref] [PubMed]


