
Family health history of colorectal cancer: a structural equation model of factors influencing Chinese Americans’ communication with family members
Introduction
Chinese Americans, the largest subgroup of Asian Americans with a 63% of first generation immigrants (1,2), suffer from high incidences and mortality rates of colorectal cancer (CRC) (3,4). CRC is the second most diagnosed cancer for both Chinese American males and females. It also ranks as the second leading cause of death by cancer for Chinese American women and third for Chinese American men (3). Family health history (FHH) of CRC is a record of an individual’s CRC family medical history and plays an important role in CRC prevention. As an identification marker to classify the CRC risk level, FHH of CRC can help physicians provide patients with personalized CRC prevention recommendations, such as undergoing early or more frequent CRC screenings, receiving genetic testing and counseling, as well as engaging in specific healthy behaviors to lower the risk of CRC (5-8).
The use of FHH in CRC prevention has been promoted by leading health agencies (9-11) and researchers (6,7). For example, both the Centers of Disease Control and Prevention and the American Cancer Society encourage the lay public to obtain their FHH of CRC and later share this information with physicians so that physicians can provide specific steps to prevent CRC (8,12). In addition, few FHH-based interventions for cancer (including CRC) have been developed and successfully implemented for Appalachian women (79% White and 18% Black) recruited from communities and patients (91% White) recruited from primary care practices in the United States (US) (13,14).
Given that FHH plays an important role in CRC prevention, obtaining comprehensive and accurate FHH of CRC is critical to ensure the appropriate risk classification and personalized prevention strategies. Yet, it is unknown regarding Chinese Americans’ communication (collection and discussion) of FHH of CRC with family members. Lack of such baseline data may lead to the failure of FHH-based CRC interventions and exacerbate cancer disparities for this racial/ethnic minority. To fill the gap, the purpose of this first-of-its-kind study is to: (I) examine Chinese Americans’ behavior of FHH of CRC communication with family members, and (II) assess the psychological factors affecting such behavior.
Methods
Participants
We conducted the first FHH-based CRC prevention program for Chinese Americans in Texas. Potential participants were recruited from both urban and rural areas in Texas, including Austin, Bryan/College Station, Cypress, Dallas, Galveston, Houston, Port Lavaca, and San Antonio. Specifically, we advertised for our study by posting and distributing flyers in various restaurants, grocery stores, healthcare clinics, community events, community outreach, and senior living communities. Additional recruitment methods through mass media, such as Chinese newspapers, a radio station, social media, websites, and a TV channel, and via Chinese community health workers and personal connections were adopted. Participants who were interested in the program were asked to directly contact our research team and were screened for their eligibility to participate in this study. The eligible criteria were Texas Chinese Americans with the age between 18 to 75, no personal cancer history, and were able to listen, speak, read, and write Mandarin or English. If the participants were aged 50 or older, did not follow the CRC screening guideline, such as undergoing an annual fecal occult blood testing/fecal immunochemical test every year, a CT colonography/flexible sigmoidoscopy every 5 years, or a colonoscopy every 10 years. If the participants’ ages were under 50, they had never received any CRC screening. The final sample size consisted of 742 Chinese Americans living in Texas.
Study design
The study protocol was approved by the Institutional Review Board at Texas A&M University [IRB number: 2016-0068D]. The program utilized the community-based participatory research approach with a convenience sample (15). All participants signed the informed consent and the authorization form for use and disclosure of protected health information before taking part in this study. The incentives for participating in the entire study included $75 in gift cards compensation, refreshments, and a free fecal occult blood test. This study used the baseline data, which focused on Chinese Americans’ collection and discussion of FHH of CRC with family members. Participants were given 30–45 minutes to complete the paper-and-pencil baseline survey. If they had any questions, the research team immediately answered and explained the survey items to them.
Measures
Using an integrated theoretical framework, based on the constructs from the Health Belief Model (HBM) (16), the Theory of Planned Behavior (TPB) (17), and the Social Cognitive Theory (18) associated with FHH communication and collection in the literature (15), we developed a baseline survey instrument in both Mandarin and English. The survey was reviewed by two physicians as well as the leader, staff, and volunteers at the partnering Chinese American organization. Additionally, a pilot test of the survey with a convenient sample of 11 Chinese Americans was conducted. The average age of participants was 63.7 years, and most were female (60.0%). Exploratory factor analysis suggested that the survey data had a good validity overall. With the exception of low reliability of the perceived barriers in FHH of CRC communication scale, all other constructs showed a good reliability with a Cronbach’s alpha near or above 0.80. Revisions were made based on their feedback and findings from the pilot test (15).
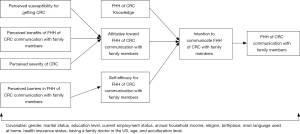
As shown in Figure 1, conceptually, knowledge, attitudes, and self-efficacy for FHH of CRC communication with family members were correlated to intention, which was directly linked to the behavior in collecting and discussing FHH of CRC with family members. Moreover, attitudes toward FHH of CRC communication were associated with perceived susceptibility of getting CRC, perceived severity for CRC, and perceived benefits of FHH communication with family members. Self-efficacy in FHH of CRC communication was related to the perceived barriers in communicating FHH of CRC with family members. The detailed measures of each scale and corresponding psychometric testing results of reliability (Cronbach’s alpha with a cutoff point as 0.5) (19-21) and construct validity [confirmatory factor analysis (CFA) with model fit indexes, such as chi-square fit statistics (χ2), root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), and comparative fit index (CFI)] in the integrated theoretical framework are described below.
Perceived susceptibility for getting CRC
Based on the HBM, perceived susceptibility is defined as an individual’s subjective belief of acquiring a specific disease (22). Adopted from the previous literature (23), this scale included three survey items with a four-point Likert scale, ranging from “Strongly Disagree” to “Strongly Agree”. An example was: “it is extremely likely that I will get CRC.” This scale had a good reliability as demonstrated by a Cronbach’s alpha of 0.876. The CFA results showed a saturated model and all the items were significantly related to the construct (P<0.001).
Perceived severity of CRC
Perceived severity, according to the HBM, refers to an individual’s “belief in the extent of harm that can result from the acquired disease (22) (page 76).” Adopted from a past study (23), the perceived severity of CRC was measured by four items using a four-point Likert scale. For example, participants were asked “The thought of getting CRC scares me [Strongly Disagree, Disagree, Agree, and Strongly Agree].” The Cronbach’s alpha of perceived severity of getting CRC was 0.876, which indicated an excellent reliability. Construct validity also indicated a good model fit [χ2(df =1) =1.69, P=0.194; RMSEA =0.031; CFI =0.999; SRMR =0.008].
Perceived benefits of FHH of CRC communication with family members
Perceived benefits, based on the HBM, define as the “belief in the advantages of the methods suggested for reducing the risk or seriousness of the disease or harmful state resulting from a particular behavior (22) (page 76).” In this study, this construct refers to Chinese American participants’ perceptions regarding health benefits resulting from FHH of CRC communication with family members. This construct was tested by three items developed by the research team and used a four-point Likert scale, ranging from “Strongly Disagree” to “Strongly Agree.” The example item was, “I believe collecting FHH of CRC would help me prevent CRC.” This construct had an excellent reliability with a Cronbach’s alpha of 0.933. The CFA result showed a saturated model due to the three items for this construct, and all three items were significantly related to the construct (P<0.001).
Knowledge of FHH of CRC
As a construct of the HBM (22), the knowledge of FHH of CRC scale consisted of seven multiple choice questions developed by the research team. This scale had a good CFA result [χ2(df =14) =47.38, P<0.001; RMSEA =0.057; CFI =1.0; SRMR =0.91] and an acceptable Cronbach’s alpha (0.513). The example question was, “a complete FHH of CRC means getting the CRC information from the first- and second-degree relatives [Disagree/Agree/Don’t know].” The answers of the knowledge questions were coded as “1” for the correct answer and as “0” for an incorrect answer as well as the “don’t know” answer. The theoretical range for the knowledge sum score was from zero to seven. The average of actual knowledge sum score from participants’ responses was 2.3 (Standard deviation =1.5).
Attitudes toward FHH of CRC communication with family members
According to the TPB, attitudes are defined as the “overall feelings of like or dislike toward any given behavior (22) (page 123)”. We examined Chinese Americans’ attitudes toward FHH of CRC communication with family members using five items on a four-point Likert-type scale developed by the research team. The item was illustrated as “I should ask family members about my FHH of CRC [Strongly Disagree, Disagree, Agree, Strongly agree].” The data of the attitudes scale had an excellent reliability with a Cronbach’s alpha coefficient of 0.941 and a good construct validity [χ2(df =3) =3.38, P=0.33; RMSEA =0.013; CFI =1.0; SRMR =0.006].
Perceived barriers to FHH of CRC communication with family members
The construct of the perceived barriers is defined as the “beliefs concerning actual and imagined costs of following the new behavior (22) (page 76)” in the HBM. Perceived barriers to FHH of CRC communication with family members were measured by four items, adopted from the previous literature (24). Participants were asked, “how much do you agree or disagree with the following challenges in collecting and discussing FHH of CRC with your family members?” The response options were strongly disagree, disagree, agree, and strongly agree. The example statements were “some of my family members do not live in the United States” and “there are Chinese cultural taboos associated with sharing and discussing FHH.” The perceived barriers scale of the four original four items had an unacceptable construct validity. Thus, based on the Pearson correlation findings, the perceived barriers scale was coded as two dimensions: (I) perceived family related barriers (two items) and (II) perceived non-family related barriers (two items).
Self-efficacy for FHH of CRC communication with family members
The term for self-efficacy is defined as the “confidence in one’s ability to pursue a behavior (22) (page 77)” by the Social Cognitive Theory. In this study, we developed six questions to measure Chinese Americans’ self-efficacy for FHH of CRC communication with family members, such as “how confident are you in asking family members about your FHH of CRC?”. We asked the Chinese participants to circle the number which best indicated their level of confidence in each question. The smallest number, zero, meant “not confident at all” and the largest number, ten, meant that they had “absolutely (100%) confident.” The self-efficacy scale had an excellent internal consistency as demonstrated by a Cronbach’s alpha of 0.966 and a good construct validity as shown by the CFA with a good model fit [χ2(df =4) =13.27, P<0.05; RMSEA =0.056; CFI =0.993; SRMR =0.005].
Intention to communicate FHH of CRC with family members
Intention is defined as a person’s “thought to perform the behavior (22) (page 123)” by the TPB. The TPB assumes that intention is a good predictor of the corresponding constant health behaviors (25,26). We developed five items with a four-point Likert-type scale ranging from “Not Likely at All” to “Extremely Likely” to assess Chinese American participants’ intentions to communication FHH of CRC with family members. For example, participants were asked “how likely are you to ask family members about your FHH of CRC.” The Cronbach’s alpha coefficient of the intention scale was 0.957, indicating an excellent internal consistency. The CFA results showed that the intention scale also had a good construct validity [χ2(df =2) =9.17, P<0.05; RMSEA =0.07; CFI =0.996; SRMR =0.008].
FHH of CRC communications with family members
In this study, behavior refers to the Chinese American participants’ FHH of CRC communication with family members. This construct was evaluated by five items developed by our research team with a five-point Likert-type scale ranging from “Never”, “Seldom”, “Sometimes”, “Often”, to “Always”. An example item was, “I have asked family members about my FHH of CRC.” Cronbach’s alpha of this behavior scale was 0.966 which indicated an excellent reliability. Construct validity also suggested a good model fit [χ2 (df =3) =9.24, P<0.05; RMSEA =0.053; CFI =0.994; SRMR =0.008].
Moreover, as socio-demographic characteristics and acculturation levels may shape Chinese Americans’ CRC communication with family members, these variables served as covariates in the integrated theoretical framework. The measures of the socio-demographic characteristics and the acculturation level are listed below:
Socio-demographic characteristics
Socio-demographic characteristics included age, gender (female or male), marital status (married, single, or divorced/separated/widowed), education level (below college or college graduate or above), current employment status (employed or others, such as unemployed and retired), annual household income (<$20,000, $20,000 to <$35,000, $35,000 to <$50,000, $50,000 to <$75,000, or ≥$75,000), religion (Christian, Buddhism, unaffiliated/none, or others), birthplace (born outside of the US or born in the US), main language used at home (English or other languages), health insurance status (uninsured, private insurance, Medicare, Medicaid, multiple insurances, or unknown insurance), and the status of having a family doctor in the US (no or yes).
Acculturation level
To measure participants’ acculturation levels, a reliable and valid acculturation scale for Chinese immigrants was adopted. This scale consisted of 12-items with a five-point Likert scale, which covered the dimensions of preferred languages used in personal life, desired languages for the mass Media, and favored ethnicities of social contacts. The acculturation score was calculated by the average of the summed scores of the 12 items. The theoretical range of the acculturation scale was one to five and higher scores represented a higher level of acculturation (27). The survey data from participants showed that participants overall had a low acculturation level with an average of 1.9 (standard deviation =0.7 and range, 1.0–4.3).
Data analysis
Descriptive statistics were conducted using SPSS 22.0 (28). Mplus (V8.0), a structural equation modeling (SEM) program, was used to analyze the relationships among the constructs in the integrated theoretical model. Missing data were analyzed with the full information maximum likelihood estimation method as a default approach in Mplus (29). We tested the correlations between with the main theoretical constructs (i.e., knowledge, attitudes, self-efficacy, intention, and behavior) and covariates (i.e., social-demographic characteristics and the acculturation level). Only covariates that were significantly correlated with the main theoretical constructs were included into the final SEM model. An adequate model fit for SEM model was considered for those with acceptable model fit indexes: RMSEA smaller than 0.08, CFI greater than 0.90, and SRMR smaller than 0.06 (30).
Results
Demographic descriptive data for our study participants are presented in Table 1. Of 742 participants, 60.0% were female, 72.0% were married, and 24.8% were uninsured with an average age was 47.7 years (SD =14.9). About half of the participants were employed (52.7%) and had college degrees or above (54.5%), some religious beliefs (52.5%), and primary care physicians (45.1%). The majority of the participants were not born in the US (95.4%) and did not speak English at home (95.5%).
Table 1
| Variables | Frequency |
|---|---|
| Gender | |
| Female | 60.0% |
| Male | 40.0% |
| Marital status | |
| Married | 72.0% |
| Single | 21.0% |
| Divorced/separated/widowed | 7.0% |
| Education level | |
| Below college | 45.5% |
| College graduate or above | 54.5% |
| Current employment status | |
| Employed | 52.7% |
| Other (i.e., unemployed, retired, student, and homemaker) | 47.3% |
| Annual household income | |
| <$20,000 | 37.4% |
| $20,000 to <$35,000 | 17.9% |
| $35,000 to <$50,000 | 10.5% |
| $50,000 to <$75,000 | 12.5% |
| $75,000 or more | 21.6% |
| Religion | |
| Christian | 33.1% |
| Buddhism | 15.9% |
| Unaffiliated/none | 47.5% |
| Other (i.e., Judaism, Taoism, and multiple religions) | 3.5% |
| Birthplace | |
| Born outside of the US | 95.4% |
| Born in the US | 4.6% |
| Main language used at home | |
| English | 4.5% |
| Other non-English languages (e.g., Mandarin, Cantonese, Taiwanese, and Shanghainese) | 95.5% |
| Health insurance status | |
| Uninsured | 24.8% |
| Private | 56.0% |
| Medicare | 5.8% |
| Medicaid | 1.0% |
| Multiple insurances | 1.6% |
| Unknown insurance | 10.9% |
| Having a family doctor in the US | |
| No | 54.9% |
| Yes | 45.1% |
| Age | 47.7 (14.9)a |
a, mean (standard deviation).
FHH of CRC communication with family members
As shown in Table 2, the majority of the Chinese Americans in our sample had never or seldom collected and discussed with their family members about their FHH of CRC. Specifically, most of the participants had never or seldom asked family members about FHH of CRC (69.0%), collected FHH of CRC (73.3%), gathered complete (78.3%) and accurate (78.6%) FHH of CRC, and discussed FHH of CRC with family members (74.8%). Moreover, the barriers affecting FHH communication with family members included family related barriers—physical distance from family members outside the US (86.0%) and perceived healthy family (42.8%), and non-family related barriers—Chinese cultural taboos (25.0%) and the beliefs of insignificance of communicating FHH of CRC with family members (12.8%).
Table 2
| How often do you perform the following behaviors? | Never | Seldom | Sometimes | Often | Always |
|---|---|---|---|---|---|
| I have asked family members about my FHH of CRC | 54.4% | 14.6% | 21.1% | 6.9% | 3.0% |
| I have collected my FHH of CRC. | 64.3% | 9.0% | 17.8% | 6.2% | 2.7% |
| I have collected a complete FHH of CRCa | 69.6% | 8.7% | 14.3% | 5.2% | 2.2% |
| I have collected an accurate FHH of CRCb | 70.9% | 7.7% | 13.9% | 4.9% | 2.6% |
| I have discussed FHH of CRC with family members | 60.1% | 14.7% | 16.4% | 6.0% | 2.7% |
a, a complete FHH of CRC included information of three-degrees of relatives; b, an accurate FHH of CRC included information regarding if the family members had been diagnosed with CRC and the age of CRC diagnosis. FHH, family health history; CRC, colorectal cancer.
SEM findings
As seen in Figure 2, the SEM model fit the survey data adequately based on the model fit indices (i.e., CFI =0.935; RMSEA =0.074; SRMR =0.021) even though the overall model chi-square was significant [χ2(20) =100.88, P<0.001]. Perceived susceptibility for getting CRC, perceived severity for CRC, and perceived benefits of FHH of CRC communication with family members were significantly and positively associated with Chinese American participants’ attitudes toward FHH communication with family members (β =0.089, P<0.005; β =0.141, P<0.001; and β =0.479, P<0.001, respectively). Participants’ stronger perceptions of non-family related barriers, including Chinese cultural taboos and beliefs of unimportance in collection and discussion of FHH of CRC were correlated with their lower self-efficacy in communicating FHH of CRC with their families (β =−0.130, P<0.005). Attitudes (β =0.324, P<0.001) and self-efficacy (β =0.577, P<0.001) in FHH of CRC communication were positively and significantly associated with the Chinese American sample’s intention in communicating FHH of CRC with family members. Stronger intention was correlated with participants’ behavior in FHH of CRC communication (β =0.410, P<0.001).
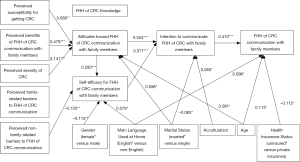
Furthermore, the behavior in FHH of CRC communication with family members was positively related to non-English speaking at home (β =0.096, P<0.05), older ages (β =0.113, P<0.05), and uninsured status (β =−0.112, P<0.05). Intention in communicating FHH of CRC was positively correlated to higher acculturation level (β =0.083, P<0.05), and married status (β =−0.083, P<0.05). Attitudes toward FHH of CRC communication had positive relationships with older age (β =0.081, P<0.05) and single status (β =0.098, P<0.05). Participants’ confidence in collecting and discussing FHH of CRC with family members were associated with the female gender (β =−0.115, P<0.005) and not speaking English at home (β =0.079, P<0.05) in positive ways.
Discussion
To the best of our knowledge, this first-of-its-kind study contributes to the current limited understanding about FHH of CRC communication with family members among Chinese Americans. Our findings suggested that Chinese Americans overall lacked FHH of CRC communication with family members. The data were slightly higher than the previous national survey result, which showed that 70.2% of Americans did not actively collect FHH information from their family members (31). Moreover, participants had a deficient knowledge of FHH. They also reported challenges affecting their discussing and collecting FHH of CRC with families, such as physical distances from family members who lived outside the US and misconceptions of the need to collect FHH of CRC due to the perception that the family members look healthy. Therefore, FHH education and interventions aiming to improve the FHH of CRC communication for this particular population are needed.
The survey data supported the integrated theoretical framework we proposed. In particular, FHH of CRC communication behavior was directly associated with Chinese participants’ intention, which was related to attitudes and self-efficacy in communicating FHH of CRC with family members. Attitudes toward FHH of CRC communication with family members were positively correlated to Chinese American participants’ perceive susceptibility of getting CRC, perceived seriousness of CRC, and perceived benefits of FHH communication. Self-efficacy in collecting and discussing FHH of CRC with family members were significantly related to the non-family related barriers. As such, these results suggested that FHH-based CRC interventions and education for Chinese Americans should focus on improving intention, attitudes, self-efficacy, and benefits of FHH communication, enhancing the beliefs of CRC susceptibility and severity, and addressing the non-family related barriers to FHH communication. For example, based on the effective strategies which were successfully implemented in other populations reported by past studies (32,33), future FHH-based CRC interventions may introduce an easy-to-use FHH collection tool, educate Chinese Americans on the importance of FHH of collection, and help them build up FHH communication skills with family members.
Interestingly, our study findings suggested that a few demographic characteristics were associated with participating Chinese Americans’ FHH of CRC communication behavior. Specifically, participants who were older, had no health insurance, and did not speak English at home were more likely to communicate of FHH of CRC with family members. This might be because the older and/or uninsured Chinese Americans might have worried more about their health than those who are younger and had private health insurance (34,35). Moreover, given that the majority of Chinese Americans are first-generation immigrants and had low English literacy (1), similar to that of Latino immigrants (36), participants who did not speak English at home might find it easier in connecting with other family members both in and outside the US to gather FHH of CRC.
Of note, although the original theoretical model proposed that knowledge of FHH of CRC was linked to Chinese American participants’ intention to communicate FHH of CRC with family members, the SEM findings showed that this pathway was not statistically significant. This could be that our knowledge scale measured the sample’s fundamental and basic knowledge in FHH of CRC. Similar to past studies (37,38), this type of knowledge was not related to intention. Yet, it is still important to educate Chinese Americans about the correct information regarding FHH of CRC to empower them with such knowledge. For example, knowing the definitions of first-, second-, and third-degree relatives would help participants in collecting a comprehensive FHH.
The original theoretical model proposed an association between perceived barriers in FHH of CRC communication and self-efficacy for FHH of CRC communication with family members. While perceived non-family-related barriers in FHH of CRC communication was significantly associated with self-efficacy, perceived family-related barriers had an insignificant relationship with self-efficacy in the final SEM model. In the initial data analysis stage, however, Pearson’s bivariate correlation showed that family-related barriers in FHH of CRC communication was significantly associated with self-efficacy for FHH of CRC communication with family members with a small correlation (r=−0.058, P<0.001). In the final SEM model, such a weak relationship might have been overpowered by other variables (i.e., attitudes, gender, main language used at home, and perceived non-family-related barriers), which had stronger effects with self-efficacy.
Our study is limited in three aspects. First, this study analyzed the baseline survey data. Due to the restriction of the cross-sectional design, we were unable to ascertain causal relationships. Second, the findings from this study may have a limited generalizability as the majority of participants were first-generation immigrants and the study was conducted in Texas. Future efforts may aim to assess the FHH of CRC communication behavior among second and third generations and/or resident outside of Texas. Third, our study suffered from potential selection bias. We recruited the potential participants directly from the Chinese communities in Texas. Our participants, therefore, might have been more interested in the topic of our program and/or have been more concerned about their health.
Despite the limitations above, this study served as an initial window to examine Chinese Americans’ FHH communication with family members using a large-scale survey data in Texas. Texas has the third largest Asian American population in the US (39). Our study showed that the majority of Chinese Americans did not communicate FHH of CRC with their family members. In addition, we established an integrated theoretical framework to propose relations among various theoretical constructs, demographic variables, and the acculturation level—which was later tested with the SEM. The SEM findings can be utilized for the development of FHH interventions and education for Chinese Americans in Texas.
Acknowledgments
Funding: This work was supported by
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Hui-Yi Lin, Tung-Sung Tseng) for the series “Population Science in Cancer” published in Translational Cancer Research. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2019.05.18). The series “Population Science in Cancer” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was taken from all patients. The study protocol was approved by the Institutional Review Board at Texas A&M University [IRB number: 2016-0068D].
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pew Research Center. Chinese in the U.S. fact sheet. 2017. Available online: http://www.pewsocialtrends.org/fact-sheet/asian-americans-chinese-in-the-u-s/. Accessed Feb 28, 2019.
- Hoeffel EM, Rastogi S, Kim MO, et al. The Asian Population: 2010 Census Briefs. 2012. Available online: https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf. Accessed Feb 28, 2019.
- Thompson CA, Gomez SL, Hastings KG, et al. The Burden of Cancer in Asian Americans: A Report of National Mortality Trends by Asian Ethnicity. Cancer Epidemiol Biomarkers Prev 2016;25:1371-82. [Crossref] [PubMed]
- Jin H, Pinheiro PS, Xu J, et al. Cancer incidence among Asian American populations in the United States, 2009–2011. Int J Cancer 2016;138:2136-45. [Crossref] [PubMed]
- Yoon PW, Scheuner MT, Peterson-Oehlke KL, et al. Can family history be used as a tool for public health and preventive medicine? Genet Med 2002;4:304-10. [Crossref] [PubMed]
- House W, Sharp D, Sheridan E. Identifying and screening patients at high risk of colorectal cancer in general practice. J Med Screen 1999;6:205-8. [Crossref] [PubMed]
- Lowery JT, Ahnen DJ, Schroy PC 3rd, et al. Understanding the contribution of family history to colorectal cancer risk and its clinical implications: A state-of-the-science review. Cancer 2016;122:2633-45. [Crossref] [PubMed]
- Centers for Disease Control and Prevention. Family Health History of Colorectal (Colon) Cancer. 2018. Available online: https://www.cdc.gov/genomics/disease/colorectal_cancer/family_history_coloretal.htm. Accessed Feb 28, 2019.
- Dennis Ahnen, Paul Schroy, NCCRT Family History and Early Age Onset CRC Task Group. Thanksgiving Is Family Health History Day. 2017. Available online: http://nccrt.org/blog-family-health-history-day/. Accessed Feb 28, 2019.
- Centers for Disease Control and Prevention. Knowing is Not Enough—Act on Your Family Health History. 2018. Available online: https://www.cdc.gov/features/familyhealthhistory/index.html. Accessed Feb 28, 2019.
- U.S. Department of Health & Human Services. The Surgeon General's Family Health History Initiative. 2016. Available online: https://www.hhs.gov/programs/prevention-and-wellness/family-health-history/index.html. Accessed Feb 28, 2019.
- American Cancer Society. Genetic Testing, Screening, and Prevention for People with a Strong Family History of Colorectal Cancer. 2018. Available online: https://www.cancer.org/cancer/colon-rectal-cancer/causes-risks-prevention/genetic-tests-screening-prevention.html. Accessed Feb 28, 2019.
- Wallace JP, Baugh C, Cornett S, et al. A family history demonstration project among women in an urban Appalachian community. Prog Community Health Partnersh 2009;3:155-63. [Crossref] [PubMed]
- Ruffin MT 4th, Nease DE Jr, Sen A, et al. Effect of preventive messages tailored to family history on health behaviors: the Family Healthware Impact Trial. Ann Fam Med 2011;9:3-11. [Crossref] [PubMed]
- Li M, Yeh YL, Sun H, et al. Community-based participatory research: a family health history-based colorectal cancer prevention program among Chinese Americans. J Cancer Educ 2019; [Epub ahead of print]. [PubMed]
- Rosenstock IM. The Health Belief Model and preventive health behavior. Health Educ Monogr 1974;2:354-86. [Crossref]
- Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an introduction to theory and research. Boston: Addison-Wesley Pub. Co., 1975.
- Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, 1986.
- Nunnally JC, Bernstein IH, Berge JM. Psychometric theory. New York: McGraw-Hill, 1967.
- Churchill GA Jr. A paradigm for developing better measures of marketing constructs. J Mark Res 1979;16:64-73. [Crossref]
- Hinton PR, Brownlow C, McMurray I, et al. SPSS Explained. New York: Routledge, 2004.
- Sharma M, Romas JA. Theoretical foundations of health education and health promotion. Burlington, Massachusetts: Jones & Bartlett Learning, 2012.
- Green PM, Kelly BA. Colorectal cancer knowledge, perceptions, and behaviors in African Americans. Cancer Nurs 2004;27:206-15. [Crossref] [PubMed]
- Chen LS, Li M, Talwar D, et al. Chinese Americans’ views and use of family health history: a qualitative study. PLoS One 2016;11:e0162706. [Crossref] [PubMed]
- Hrubes D, Ajzen I, Daigle J. Predicting Hunting Intentions and Behavior: An Application of the Theory of Planned Behavior. Leis Sci 2001;23:165-78. [Crossref]
- Bamberg S, Ajzen I, Schmidt P. Choice of Travel Mode in the Theory of Planned Behavior: The Roles of Past Behavior, Habit, and Reasoned Action AU - Bamberg, Sebastian. Basic Appl Soc Psych 2003;25:175-87. [Crossref]
- Gupta R, Yick AG. Preliminary validation of the acculturation scale on Chinese Americans. Prev Hum Serv 2001;2:43-56.
- SPSS IBM. IBM SPSS Statistics 22. Algorithms Chicago: IBM SPSS Inc., 2013.
- Muthén LK, Muthén BO. Mplus User's Guide. Eighth Edition. Los Angeles, CA: Muthen & Muthen, 1998-2017.
- Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling 1999;6:1-55. [Crossref]
- Centers for Disease Control and Prevention (CDC). Awareness of family health history as a risk factor for disease--United States, 2004. MMWR Morb Mortal Wkly Rep 2004;53:1044-7. [PubMed]
- Kaphingst KA, Lachance CR, Gepp A, et al. Educating underserved Latino communities about family health history using lay health advisors. Public Health Genomics 2011;14:211-21. [Crossref] [PubMed]
- Molster C, Kyne G, O'Leary P. Motivating intentions to adopt risk-reducing behaviours for chronic diseases: impact of a public health tool for collecting family health histories. Health Promot J Austr 2011;22:57-62. [Crossref] [PubMed]
- Patrick DL, Madden CW, Diehr P, et al. Health status and use of services among families with and without health insurance. Med Care 1992;30:941-9. [Crossref] [PubMed]
- El-Gabalawy R, Mackenzie CS, Thibodeau MA, et al. Health anxiety disorders in older adults: conceptualizing complex conditions in late life. Clin Psychol Rev 2013;33:1096-105. [Crossref] [PubMed]
- Goergen AF, Ashida S, Skapinsky K, et al. What you don't know: Improving family health history knowledge among multigenerational families of Mexican origin. Public Health Genomics 2016;19:93-101. [Crossref] [PubMed]
- Chen LS, Goodson P, Jung E, et al. A survey of Texas health educators' family health history-based practice. Am J Health Behav 2015;39:632-9. [Crossref] [PubMed]
- Chen LS, Kwok OM, Goodson P. US health educators' likelihood of adopting genomic competencies into health promotion. Am J Public Health 2008;98:1651-7. [Crossref] [PubMed]
- U.S. Department of Health & Human Services. Profile: Asian Americans. 2015. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=63. Accessed Feb 28, 2019.


