
The value of hysteroscopy and transvaginal ultrasonography in the diagnosis of endometrial hyperplasia: a systematic review and meta-analysis
Introduction
Pathologic endometrial hyperplasia is an endometrial proliferative lesion with irregular gland size, increased glandular mass, and increased interstitial ratio of glands. It is a common gynecological disorder and is often characterized by abnormal uterine bleeding (1). According to the 2014 edition of the World Health Organization pathological diagnosis classification, endometrial hyperplasia was classified into non-atypical endometrial hyperplasia and endometrial atypical hyperplasia depending on whether it has cell atypia; endometrial atypical hyperplasia is considered to be the precancerous lesions of the type I endometrial cancer (2). Diagnosis of endometrial hyperplasia is of great value in preventing the progression int endometrial cancer (especially type I endometrial cancer). Auxiliary examination techniques of endometrial hyperplasia include transvaginal ultrasonography (3), hysteroscopic examination or hysteroscopy guide biopsy (4), saline infusion sonography (5,6), magnetic resonance imaging (MRI) (7,8), computed tomography (CT) (9), cervical (10) and endometrial cytology (11), and diagnostic curettage (12). Among these methods, transvaginal ultrasonography and hysteroscopic examination are the two auxiliary examination methods used most commonly in clinical practice. The final diagnosis of endometrial hyperplasia was based primarily on histological results. However, there is no overall value analysis of hysteroscopic examination and transvaginal ultrasonography in the diagnosis of endometrial hyperplasia. Therefore, the aim of this study is to evaluate the diagnostic value of hysteroscopic and transvaginal ultrasonography examination for endometrial hyperplasia systematically using the meta-analysis method, in order to provide recommend auxiliary diagnostic method for such pathologic lesions.
Methods
Information retrieval
A total of 8 databases were searched in detail from inception of the database to December 2017. The databases that were searched include China Knowledge Network Database, Wanfang Chinese Database, China Biomedical Literature Database, China Science and Technology Journal Database, PubMed, Medline, The Cochrane Library, and web of science. The retrieval combined the following topic terms, free search terms and key words: “Endometrial Hyperplasia/Simple Endometrial Hyperplasia/Complex Endometrial Hyperplasia/Atypical Endometrial Hyperplasia/ Hysteroscopic Examination/Hysteroscopy/Uterine cavity Endoscopy/diagnostic hysteroscopy/Transvaginal Ultrasonography/Ultrasonic Imaging/Transvaginal Sonography/Transvaginal Color Doppler”.
Inclusion and exclusion standard
Inclusion standard
(I) The type of research was diagnostic research, Mandarin and English were the preferred languages; (II) the research target was patients with endometrial hyperplasia as diagnosed by gold standard to have endometrial cancer (pathological diagnosis) methods who formed the cases group. Those with other endometrial benign diseases, or healthy women were used as the control group; (III) the outcome index comprised of sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, diagnostic odds ratio, area under the summary receiver operating characteristic curve, and the Cochrane-Q index.
Exclusion standard
The following were excluded from the search: (I) Conference papers, reviews, lectures, abstracts, and other relevant published materials; (II) unavailable full texts papers; (III) literature with lack of significant information or with poor data integrity; (IV) self-control clinical trials.
Document quality evaluation
The quality of the literature was evaluated with QUADAS-2 quality evaluation standard (13,14). The QUADAS-2 tool is mainly composed of case selection, evaluation test, gold standard, test procedure, and time interval. It uses “yes”, “no”, or “unclear” to answer the relevant question. The answer is then used to determine the methodological quality of the included studies.
Data extraction
Two researchers screened the literature, extracted data, and evaluated the quality of the literature based on the inclusion and exclusion standard independently. They used self-made data extraction forms, which included the following information: basic information in the literature, patient characteristics, number of samples, hysteroscopic diagnosis, vaginal ultrasound diagnosis, pathologic diagnosis, the number of true positive cases, false positive cases, false negative cases, and true negative cases.
Statistical processing
Data-analysis was performed using Review Manager 5.3, Stata 13.0, and Metadisc 1.4 software. according to the implementation guidelines for the evaluation of diagnostic test systems by Devillé et al. (15), we calculated the combined sensitivity, combined specificity, combined positive likelihood ratio, combined negative likelihood ratio, combined diagnostic odds ratio, and the corresponding 95% CI to obtain the diagnostic value of hysteroscopy and transvaginal ultrasonography for endometrial hyperplasia. We also plotted a summary receiver operating characteristic curve and calculated its area under the summary receiver operating characteristic curve and the Cochrane-Q index in our investigation. The test level for the meta-analysis was α=0.05. Deeks funnel plots were used to analyze potential publication bias.
Results
Information retrieval results
A total of 529 related articles were detected at the beginning of this study, and after thorough reading and screening by layer, 9 studies were accepted for our investigation finally (16-24). The literature screening process and results was as shown in Figure 1.
Basic characteristics and quality of selected literature
The basic characteristics of the included studies was as shown in Table 1, and the results of the evaluation of literature quality was as shown in Figure 2. The 9 studies included a combined total of 1,354 cases, 350 were diagnosed with endometrial hyperplasia. Four of the studies (16,19,20,22) were prospective studies while five were retrospectively designed (17,18,21,23,24). All studies didn’t mention the specific recruitment methods. But there were still some risks on bias, applicability concerns for the index test and applicability concerns of patient selection: Regarding risk of bias for the patient selection, one study was labeled as having high bias (22). Regarding applicability concerns for the index test, one study did not prespecify the diagnostic threshold (24). Regarding applicability concerns for the patient selection, one study was labeled as having high bias (19).
Table 1
| Study | Country | Research design | Age (year) | Total number of objects (person) | Endometrial hyperplasia | Non-endometrial hyperplasia | Method | TP (n) | FP (n) | FN (n) | TN (n) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bingol et al., 2011 (16) | Turkey | P | 61.60±9.60 | 137 | 39 | 98 | HM | 37 | 1 | 2 | 97 |
| TU | 27 | 19 | 12 | 79 | |||||||
| Chen et al., 2015 (17) | China | R | 38.88±10.28 | 208 | 56 | 152 | HM | 32 | 29 | 24 | 123 |
| TU | 42 | 39 | 14 | 113 | |||||||
| Li et al., 2015 (18) | China | R | 45.50±5.50 | 192 | 60 | 132 | HM | 49 | 8 | 11 | 124 |
| TU | 45 | 16 | 15 | 116 | |||||||
| Mukhopadhayay et al., 2007 (19) | India | P | 44–55 | 85 | 14 | 71 | HM | 7 | 3 | 7 | 68 |
| TU | 6 | 9 | 8 | 62 | |||||||
| Garg et al., 2016 (20) | India | P | Average 46.315 | 60 | 27 | 33 | HM | 17 | 18 | 10 | 15 |
| TU | 16 | 6 | 11 | 27 | |||||||
| Shen et al., 2016 (21) | China | R | 46.80±5.70 | 245 | 78 | 167 | HM | 63 | 9 | 15 | 158 |
| TU | 56 | 21 | 22 | 146 | |||||||
| Xu et al., 2007 (22) | China | P | 59.20±6.70 | 89 | 6 | 83 | HM | 5 | 3 | 1 | 80 |
| TU | 4 | 38 | 2 | 45 | |||||||
| Yang et al., 2016 (23) | China | R | 45.31±6.27 | 252 | 56 | 196 | HM | 38 | 11 | 18 | 185 |
| TU | 38 | 61 | 18 | 135 | |||||||
| Yao et al., 2008 (24) | China | R | 27–65, average 46.1 | 86 | 14 | 72 | HM | 7 | 3 | 7 | 69 |
| TU | 8 | 8 | 6 | 64 |
Because the inclusion criteria for each study are not identical, the non-endometrial proliferative patients in the table include patients with endometrial cancer and/or other benign diseases of the endometrium and/or healthy women. P, prospective research; R, retrospective research; HM, hysteroscopy examination; TU, transvaginal ultrasonography.
Systematic review results
Results of the heterogeneity test showed no heterogeneity arising from threshold effects in the dates (Spearman correlation coefficient for hysteroscopic examination =−0.343, P=0.366; Spearman correlation coefficient for transvaginal ultrasonography examination =0.092, P=0.814). The summary receiver operating characteristic curve plan, which does not have a “shoulder arm” distribution, suggested that there is no heterogeneity caused by the threshold effect. In the diagnostic odds ratio forest map, the diagnostic odds ratio and the combined diagnostic odds ratio for each study were not distributed along the same line, indicating that heterogeneity was caused by non-threshold effects. The combined sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio with the Cochrane-Q index for hysteroscopic examination was 0.73, 0.92, 9.87, 0.34, and 70.9 respectively (P<0.05), and their corresponding I2 values was 76.0%, 90.8%, 92.9%, 81.2%, and 88.7% respectively. The combined sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio with the Cochrane-Q index for transvaginal ultrasonography was 0.69, 0.78, 3.40, 0.41, and 161.11 (P<0.05) respectively, and their corresponding I2 values were 5.3%, 87.0%, 75.1%, 28.9%, and 50.3% respectively.
Meta-analysis results were as shown in Figure 3 and Figure S1. The combined sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio with hysteroscopic examination for the diagnosis of endometrial hyperplasia was 0.73 (95% CI: 0.68−0.77), 0.92 (95% CI: 0.90−0.93), 9.87 (95% CI: 4.08−23.84), 0.34 (95% CI: 0.22−0.52), and 31.64 (95% CI: 10.34−96.78) respectively. The combined sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio with transvaginal ultrasonography for the diagnosis of endometrial hyperplasia was 0.69 (95% CI: 0.64−0.74), 0.78 (95% CI: 0.76−0.81), 3.40 (95% CI: 2.46−4.70), 0.41 (95% CI: 0.34−0.50), and 8.94 (95% CI: 5.80−13.79) respectively. The area under the summary receiver operating characteristic curve for hysteroscopic examination and transvaginal ultrasonography was 0.8830 and 0.8180 respectively, and the corresponding Cochrane-Q index indices was 0.8135 and 0.7518 respectively.
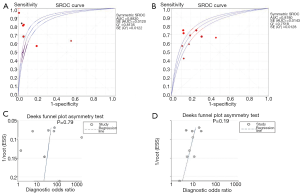
Publication bias evaluation
Deeks funnel plot tests did not show publication bias for hysteroscopic examination and transvaginal ultrasonography (P>0.05, Figure 3).
Discussion
Endometrial cancer is one of the most common gynecologic malignancy in China (25). It is generally posited that endometrial atypical hyperplasia is the precancerous lesion of type I endometrial cancer. Endometrial hyperplasia has become one of the focuses of attention in the field of gynecology. Improving the diagnostic accuracy and identifying the pathological type is crucial to improve the prognosis of women with the subsequent disease.
Diagnostic curettage is widely used in the diagnosis of gynecological diseases, and was the main method used in the diagnosis of endometrial atypical hyperplasia in the past (26). However, endometrial atypical hyperplasia may often be accompanied by local cancer, and diagnostic curettage may miss the diagnosis of endometrial cancer due to examination blindness typical of this method (27). Transvaginal ultrasonography has the advantages of being non-invasive, convenient, economical, easy to operate, reproducible, and painless. It can show irregular endometrial contours or abnormal endometrial thickness, and good repeatability characteristic in suggesting such endometrial lesions (3,28). A number of studies (29-31) proposed that women with post-menopausal vaginal bleeding and endometrial thickness ≥4–5 mm should be recommended to receive endometrial biopsy. Hysteroscopy is a minimally invasive technique that allows direct observation of the endometrium, particularly at the bilateral fallopian tube opening. Uterine cavity and endometrial morphology under hysteroscopic examination can improve diagnostic sensitivity and accuracy (32). Under hysteroscopy, the endometrium of patients with endometrial hyperplasia may show local or diffuse hyperplasia, and some may have single or multiple protrusions, which may be honeycomb or mesh. If it is grayish white or yellow, or a heterogeneous blood vessel with a large distribution, endometrial atypical hyperplasia or endometrial cancer should be highly suspected (33). In theory, hysteroscopic biopsy is superior to blind diagnostic curettage and can detect blind missed lesions; it has a high diagnostic accuracy for endometrial hyperplasia. Some studies have shown that the use of hysteroscopy for the diagnosis of endometrial lesions is more accurate than for the exclusion of endometrial lesions (34); its diagnostic value in endometrial lesions is receiving much more attention latterly. In Evaluating Postmenopausal Asymptomatic Women with thickened Endometrium, hysteroscopy allows an accurate diagnosis of benign endometrial pathology and suspected malignant endometrial pathology, avoids biopsy in case of atrophic endometrium (35).
This study included a diagnostic test comparing the diagnostic value of hysteroscopic examination and transvaginal ultrasonography for endometrial hyperplasia in the same population. According to the meta-analyses results, hysteroscopic examination has a higher sensitivity, specificity, and area under the summary receiver operating characteristic curve for the diagnosis of endometrial hyperplasia compared with transvaginal ultrasonography, and its diagnostic efficiency is higher. This study directly compares the combined values of the meta-analyses of the diagnostic indicators of the two examination methods. Hysteroscopy can be an extremely well tolerated and effective tool to diagnose uterine disorder. But Its complications can be severe and life-threatening, it is essential that the surgeon, with proper training and education, understands and is ready to manage the potential complications (36).
Nevertheless, there were notable limitations in this study. For instance: (I) the overall quality of the included studies was not high, and may have potentially affected the reliability of the conclusions; (II) in the inclusion and exclusion criteria of this study, other features that may have affected hysteroscopic examination and ultrasonography, such as menstrual status, type of biopsy, type of instrument (office isteroscopy or resectoscopy) were bot included, potentially causing a bias in the conclusion of the study; (III) moreover, this systematic review included Chinese and English literature only, yet didn’t rule out the possibility of language bias. Hence, with reference to the quality and quantity limitations of the included studies, further studies are necessary in the future to substantiate and validate these conclusions.
Conclusions
Hysteroscopy is better than transvaginal ultrasonography for the diagnose of endometrial hyperplasia, because of its higher sensitivity, specificity, and area under the summary receiver operating characteristic curve. More randomised controlled trials should be done in this area.

Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2019.06.33). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hoffman BL, Schorge JO, Schaffer JI, et al. Williams Gynecology. Beijing: Peking University Medical Press, 2015:819-22.
- Kurman RJ, Carcangiu ML, Herrington CS, et al. WHO classification of tumours of female reproductive organs, 4th ed. Lyon, France: International Agency for Research on Cancer, 2014:121-6.
- Kim MJ, Kim JJ, Kim SM. Endometrial Evaluation with Transvaginal Ultrasonography for the Screening of Endometrial Hyperplasia Or Cancer in Premenopausal and Perimenopausal Women. Obstet Gynecol Sci 2016;59:192-200. [Crossref] [PubMed]
- Spadoto-Dias D, Bueloni-Dias FN, Elias LV, et al. The Value of Hysteroscopic Biopsy in the Diagnosis of Endometrial Polyps. Womens Health (Lond) 2016;12:412-9. [Crossref] [PubMed]
- Cui CM, Yi DC. Comparison of diagnostic accuracy of saline infusion sonohysterography, transvaginal sonography and hysteroscopy in endometrial pathology. J Mod Med China 2011;21:4450-3.
- Chawla I, Tripathi S, Vohra P, et al. To Evaluate the Accuracy of Saline Infusion Sonohysterography (SIS) for Evaluation of Uterine Cavity Abnormalities in Patients with Abnormal Uterine Bleeding. J Obstet Gynaecol India 2014;64:197-201. [Crossref] [PubMed]
- Bakir B, Sanli S, Bakir VL, et al. Role of Diffusion Weighted MRI in the Differential Diagnosis of Endometrial Cancer, Polyp, Hyperplasia, and Physiological Thickening. Clin Imaging 2017;41:86-94. [Crossref] [PubMed]
- Ofinran O, Balega J. The Value of Magnetic Resonance Imaging in Investigating Complex Atypical Hyperplasia of the Endometrium. Minerva Ginecol 2016;68:400-4. [PubMed]
- Bogani G, Gostout BS, Dowdy SC, et al. Clinical Utility of Preoperative Computed Tomography in Patients with Endometrial Cancer. Int J Gynecol Cancer 2017;27:1685-93. [Crossref] [PubMed]
- Gupta P, Gupta N, Dey P. Morphometric Analysis of Endometrial Cells in Liquid-Based Cervical Cytology Samples. Cytopathology 2017;28:140-8. [Crossref] [PubMed]
- Yang X, Ma K, Chen R, et al. Liquid-Based Endometrial Cytology Associated with Curettage in the Investigation of Endometrial Carcinoma in a Population of 1987 Women. Arch Gynecol Obstet 2017;296:99-105. [Crossref] [PubMed]
- van Hanegem N, Prins MM, Bongers MY, et al. The Accuracy of Endometrial Sampling in Women with Postmenopausal Bleeding: A Systematic Review and Meta-Analysis. Eur J Obstet Gynecol Reprod Biol 2016;197:147-55. [Crossref] [PubMed]
- Wu L, Zhang Y, Zeng X. The QUADAS-2 Tool for Quality Assessment of Diagnostic Accuracy Study: An Introduction. J Hubei University Med 2013;32:201-8.
- Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies. Ann Intern Med 2011;155:529-36. [Crossref] [PubMed]
- Devillé WL, Buntinx F, Bouter LM, et al. Conducting Systematic Reviews of Diagnostic Studies: Didactic Guidelines. BMC Med Res Methodol 2002;2:9. [Crossref] [PubMed]
- Bingol B, Gunenc Z, Gedikbasi A, et al. Comparison of diagnostic accuracy of saline infusion sonohysterography, transvaginal sonography and hysteroscopy. J Obstet Gynaecol 2011;31:54-8. [Crossref] [PubMed]
- Chen M. Hysteroscopy and transvaginal ultrasound in the diagnosis and treatment of abnormal uterine bleeding. Hebei: Hebei Med University, 2015:9-27.
- Li M. Comparison of Ultrasound and hysteroscopy in the Diagnosis of Endometrial lesions. Practical J Can 2015;30:1031-4.
- Mukhopadhayay S, Bhattacharyya SK, Ganguly RP, et al. Comparative Evaluation of Perimenopausal Abnormal Uterine Bleeding by Transvaginal Sonography, Hysteroscopy and Endometrial Biopsy. J Indian Med Assoc 2007;105:624-626, 628. [PubMed]
- Garg P, Yadav S. Comparison of transvaginal ultrasonography and hysteroscopy in the evaluation of peri and postmenopausal bleeding. J Evolution Med Dent Sci 2016;5:1133-6. [Crossref]
- Shen C, Yu Y, Wang Q. Comparative Analysis of Vaginal Ultrasound and Hysteroscopy using in Diagnosis of Endometrial lesions. Mod Practical Med 2016;28:1050-3.
- Xu Y. Clinical Study of Transvaginal Sonography and Hysteroscopy in the Diagnosis of Postmenopausal Uterine Bleeding. Jinan: Shandong University, 2007:7-48.
- Yang F. The diagnostic value of hysteroscopy combined vaginal ultrasonography in abnormal perimenopausal uterine bleeding. Zhengzhou: Zhengzhou University, 2016:1-24.
- Yao L, Hu R, Zhong L. Transvaginal Sonography and Hysteroscopy in Diagnosing Uterus Endometrial lesions. Computed Med Imaging China 2008;(2):165-9.
- Witek Ł, Janikowski T, Bodzek P, et al. Expression of Tumor Suppressor Genes Related to the Cell Cycle in Endometrial Cancer Patients. Adv Med Sci 2016;61:317-24. [Crossref] [PubMed]
- Ma K, Yang X, Chen R, et al. Liquid-Based Endometrial Cytology Associated with Curettage in the Investigation of Endometrial Carcinoma in Postmenopausal Women. Taiwan J Obstet Gynecol 2016;55:777-81. [Crossref] [PubMed]
- Bourdel N, Chauvet P, Tognazza E, et al. Sampling in Atypical Endometrial Hyperplasia: Which Method Results in the Lowest Underestimation of Endometrial Cancer? A Systematic Review and Meta-Analysis. J Minim Invasive Gynecol 2016;23:692-701. [Crossref] [PubMed]
- Aghajanova L, Velarde M C, Giudice LC. Altered Gene Expression Profiling in Endometrium: Evidence for Progesterone Resistance. Semin Reprod Med 2010;28:51-8. [Crossref] [PubMed]
- Jacobs I, Gentry-Maharaj A, Burnell M, et al. Sensitivity of Transvaginal Ultrasound Screening for Endometrial Cancer in Postmenopausal Women: A Case-Control Study within the UKCTOCS Cohort. Lancet Oncol 2011;12:38-48. [Crossref] [PubMed]
- Mahajan NN, Mahajan K, Soni R. Endometrial Thickness Screening in Premenopausal Women with Abnormal Uterine Bleeding. J Obstet Gynaecol Res 2007;33:886-7. [Crossref] [PubMed]
- Karlsson B, Granberg S, Wikland M, et al. Transvaginal Ultrasonography of the Endometrium in Women with Postmenopausal Bleeding--A Nordic Multicenter Study. Am J Obstet Gynecol 1995;172:1488-94. [Crossref] [PubMed]
- Clark TJ, Voit D, Gupta JK, et al. Accuracy of Hysteroscopy in the Diagnosis of Endometrial Cancer and Hyperplasia: A Systematic Quantitative Review. JAMA 2002;288:1610-21. [Crossref] [PubMed]
- Xia E, Li Z. Gynecological endoscopy. Beijing: People’s Medical Publishing House, 2001:81.
- Capmas P, Pourcelot AG, Giral E, et al. Office Hysteroscopy: A Report of 2402 Cases. J Gynecol Obstet Biol Reprod (Paris) 2016;45:445-50. [Crossref] [PubMed]
- Trojano G, Damiani GR, Casavola VC, et al. The Role of Hysteroscopy in Evaluating Postmenopausal Asymptomatic Women with Thickened Endometrium. Gynecol Minim Invasive Ther 2018;7:6-9. [Crossref] [PubMed]
- Cholkeri-Singh A, Sasaki KJ. Hysteroscopy Safety. Curr Opin Obstet Gynecol 2016;28:250-4. [Crossref] [PubMed]




