
TGF-β signaling proteins and CYP24A1 may serve as surrogate markers for progesterone calcitriol treatment in ovarian and endometrial cancers of different histological types
Introduction
Endometrial cancer (EC) is the fifth most common type of cancer in developed countries. In 2019, there will be approximately 320,000 new cases of EC worldwide, leading to 76,000 deaths (1). Uterine cancers are generally treated with surgery, radiation, hormonal therapy, and/or chemotherapy contingent on stage and cancer type. Surgery is employed to treat patients with early stage disease (stages I and II). Approximately 28% of early stage patients have high-risk disease and also receive radiation and/or chemotherapy in addition to surgery. Among the women with advanced-stage disease (stage III and IV), the majority receive surgery followed by radiation and/or chemotherapy. Despite the success of primary treatment, nearly all women with advanced disease experience a recurrence of cancer, which is often resistant to chemotherapy (2). The unpretentious performance of therapeutic tactics has offered the impetus for the prevention of EC, a viable alternative to chemotherapy.
A compelling body of clinical and epidemiologic evidence suggests that progestins and vitamin-D are highly effective cancer preventive agents. In premenopausal women, progestin containing oral contraceptives use grants a significant reduction in cancer risk (3-5). Moreover, progestin-potent oral contraceptives have increased cancer protective effects compared to oral contraceptives containing weak progestins (6,7). The active form of vitamin D3-calcitriol, produced in the epidermis or obtained from the diet is known for the prevention of a number of tumors, including ovarian and ECs (8,9). Levels of vitamin-D are maintained by a number of enzymes that are involved in the synthesis, activation and inactivation (10). The active 1,25-D3 is neutralized by CYP24A1. This enzyme is vital in determining the antitumor activity of vitamin-D3. It has been shown that high expression of CYP24A1 promotes carcinogenesis in a number of cancers, including breast, thyroid and prostate (11-13). We compared the expression of CYP24A1 in endometrial and ovarian cancer cells and in immortalized endometrial and ovarian epithelial cells, and found elevated CYP24A1 expression in cancer cells compared to normal cells. Furthermore, our data demonstrated a marked reduction of CYP24A1 expression in progesterone treated endometrial and ovarian cancer cells. These findings imply that CYP24A1 overexpression diminishes the antitumor effects of calcitriol in cancer cells and that progestins can be promising for sustaining calcitriol’s anti-cancer activity (14,15).
In a recent study, we examined the effects of progesterone, calcitriol, and their combination of EC cells and identified their targets of action. Our results demonstrated that combination treatment of EC cells with both agents impeded cell proliferation through increased vitamin-D receptor (VDR) expression, caspase-3 activation, induction of cell-cycle arrest and downregulation of cyclins (16) TGF-β signaling pathway performs important roles in several biological processes, such as cell growth, differentiation, apoptosis and migration. The TGF-β pathway is dysregulated in tumors and associated with cancer initiation and progression (17-19). Bokhari et al. (20) reported a significant decrease in the expression of three TGFβ isoforms, TGF-β receptor and SMAD2/3 in progesterone treated EC cells. Additionally, progesterone effectively reduced basal and TGF β1-stimulated cancer cell viability and invasion, which was associated with increased E-cadherin and decreased vimentin expression. An inhibitor of TGFβRI blocked TGFβ1-induced effects on cell viability and invasion and attenuated antitumor effects of progesterone.
Previously, we have shown that the progesterone and calcitriol combination is highly effective in inhibiting the growth of serous ovarian and endometrial tumors (14-16,20) by attenuating the expression of TGF-β signaling proteins and downregulating the expression of vitamin-D inactivating enzyme, CYP24A1. There is a critical need for developing effective chemopreventive and therapeutic strategies for distinct types of endometrial and ovarian cancer, and to determine if a consistent set of biomarkers may exist for evaluating the effectiveness of treatments initially in preclinical models and ultimately in investigations in human subjects. The availability of a breadth of cancer cell lines from different subtypes provides opportunities for the design of cancer prevention/treatment studies that can test the specificity or conversely, broad applicability of therapeutic interventions in the clinic (21). The first goal of this study was to determine if the progesterone and calcitriol combination have restricted or broad potential applications in chemoprevention and treatment in a variety of subtypes of endometrial and ovarian cancers, including those with mutations in ARID1A or PIK3CA, DNA mismatch repair (MMR) deficiency or BRCA1 null status. The second goal was to test the hypothesis that TGF-β signaling proteins and CYP24A1 may be used as generalizable surrogate biomarkers of progesterone-calcitriol response in clear cell, endometrioid, BRCA1 null and DNA MMR deficient gynecologic cancers.
Methods
Cell culture and treatment
Human ovarian and endometrial cell lines, ES-2, TOV-21G, TOV-112D, HEC-1A, OV-90, and UWB1.289 were obtained from the American Type Culture Collection (ATCC, Manassas, VA, USA). HEC-59 cells were purchased from AddexBio (San Diego, CA, USA). These human-derived cell lines were authenticated by DNA short-tandem repeat analysis by ATCC and Sigma. All cell lines were initially expanded and cryopreserved within 1 month of receipt. Cells were typically used for 3 months, at which time a fresh vial of cryopreserved cells was used. TOV-21G, TOV-112D and OV-90 were cultured in a 1:1 mixture of MCDB (Sigma, St. Louis, MO, USA): medium 199 with 15% fetal bovine serum (FBS). ES-2 and HEC-1A were grown in McCoy’s 5a Medium (ATCC, Manassas, VA, USA) with 10% FBS. The cell line UWB1.289 was cultured in a 1:1 mixture of Mammary Epithelial Basal medium (MEBM, Lonza, Walkersville, MD, USA) and Roswell Park Memorial Institute (RPMI) medium 1640 (Theromo Fisher Scientific, Waltham, MA, USA) supplemented with bovine pituitary extract (BPE), hydrocortisone, human recombinant epidermal growth factor (hEGF), insulin, penicillin and streptomycin and 3% FBS. HEC-59 cells were cultured in Iscove’s Modified Dulbecco’s Medium (IMDM) from Thermo Fisher Scientific (Waltham, MA, USA). All media were supplemented with penicillin and streptomycin to a final concentration of 1%. The cells were cultured at 37 °C in a humidified atmosphere containing 5% CO2. Forty-eight hours later, the media were replaced with the same media but containing charcoal-stripped FBS. The cells were treated with progesterone (10–80 µmol/L), calcitriol (10–80 nmol/L) or a combination for 72 or 120 hours. To avoid the toxicity associated with higher doses of progesterone in most experiments, we used the lower dose of progesterone (20 µmol/L) that has a potent inhibitory effect on the growth of cancer cells. Because high doses of calcitriol are associated with hypercalcemia in vivo, we therefore used a concentration of calcitriol that would not induce hypercalcemia in vivo (22).
Cell viability assay
Cell viability of cancer cell lines treated with progesterone, calcitriol or the combination was evaluated using the CellTiter 96 AQueous One Solution cell viability as previously reported (14,16,20). Briefly, CellTiter 96 AQueous One Solution reagent was added into each well of the 96-well assay plate containing the samples in 100 µL of culture medium. Absorbance was measured at 490 nm using an ELX800 microtiter reader (Winooski, VT, USA). Relative cell viability was expressed as % change of treated cells over vehicle-treated cells. The half maximal inhibitory concentration (IC50) values were calculated based on the four-parameter non-linear regression method by Graphpad Prism 4.0 software (San Diego, CA, USA). The combination of progesterone and calcitriol was characterized by a combination index (CI) as described by Chou et al. (23) and calculated with CompuSyn (ComboSyn, Inc., Paramus, NJ, USA). CI values were interpreted as follows: CI <1, synergism; CI =1, additive; CI >1, antagonism.
Western blot analysis
Cancer cell extracts from cells treated with progesterone or calcitriol and the combination of the two were analyzed using antibodies against TGFβ1, TGFβ2, TGFβ3, TGFβRI, TGFβRII, TGFβRIII, pSMAD2/3, SMAD2/3, SMAD4, progesterone receptor (PR) and VDR from Santa Cruz Biotechnology (Dallas, TX, USA), CYP24A1 from Abgent (San Diego, CA, USA), and β-actin from Sigma-Aldrich (St. Louis, MO, USA). Equal amounts of protein were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis and the intracellular amount of β-actin was analyzed as a loading control. The enhanced chemiluminescence system was used to visualize the protein bands as recommended by the manufacturer (Thermo Fisher Scientific, Waltham, MA, USA). Bands were quantified by densitometry using ImageJ software (version1.51j8, NIH, Bethesda, MD, USA) and protein band intensities were normalized to β-actin. The bars represent the means ± standard error of the mean (SEM) of normalized levels of three independent experiments.
Statistical analysis
Each experiment was conducted independently at least three times. Cell proliferation experiments were performed in quadruplicates and values were presented as the means ± SEM. Statistically significant differences between control and treatment groups were identified using two-way analysis of variances (ANOVAs) followed by Tukey post-hoc tests. A P value of less than 0.05 was considered statistically significant.
Results
Progesterone and calcitriol inhibit proliferation of clear cell ovarian cancer by inhibiting TGF-β signaling pathway proteins
We examined the dose response effects of progesterone and calcitriol alone or in combination on the growth of ovarian clear cell cancer lines ES-2 and TOV-21G. Cells were treated with progesterone (10, 20, 40 or 80 µmol/L), calcitriol (10, 20, 40 or 80 nmol/L), or the combination for 72 or 120 hours. At the end of the treatment time, cell viability was assessed by (3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium) (MTS) assay. Although progesterone and progesterone-calcitriol inhibited cell proliferation in all cell lines at both treatment times, only results of cells incubated with hormones for 120 hours are presented. In both cell lines, progesterone reduced cell viability in a dose-dependent manner. The IC50 values of progesterone, calcitriol and the combination of two for ES-2 were 24.86±2.62, 30.25±2.59, 18.64±1.78 and for TOV-21G were 41.64±1.59, 47.66.25±3.41, 25.84±1.96, respectively. Combined progesterone and calcitriol treatment showed a pronounced synergistic inhibitory effect (CI <0.62 for ES-2 and 0.57 for TOV-21G) on cell numbers compared to either single agent in both cell lines tested (Figure 1A). Endometrial tumors have been reported to express high levels of three TGF-β isoforms and TGF-β receptors in vivo (24,25). In addition, it has been suggested that TGF-β plays a major role in the initiation of endometrial carcinoma invasion (26). To determine whether progesterone regulates the expression of TGF-β and their receptors, ES-2 and TOV-21G cell lines were exposed to progesterone, calcitriol or their combination for 120 hours. Exposure of cells to progesterone and calcitriol-progesterone combination significantly decreased the expression of TGF-β1, TGF-βR1 and TGF-βR2 in ES-2 and TOV-21G cells. Expression of TGF-β2, TGF-β3, and TGF-βR3 was not affected by progesterone or calcitriol-progesterone combination. While the expression of total SMAD2/3 and pSMAD2/3 was attenuated with both progesterone and calcitriol-progesterone combination in both clear cell cancer cell lines, SMAD4 was not affected with any treatment (Figure 1B,C).

Effect of progesterone and calcitriol on the expression of PR, VDR and CYP24A1 in clear cell ovarian cancer
Both isoforms of PR were expressed in clear cell cancer cell lines but no marked change was observed in the expression of PR isoforms following progesterone, calcitriol, or combination treatments (Figure 1B). We also analyzed the effect of progesterone, calcitriol, or both on VDR protein expression in ovarian clear cells. As shown in Figure 1B, VDR expression was enhanced in ES-2 cells treated with progesterone and calcitriol-progesterone combination and treatment failed to alter VDR expression in TOV-21G cells. CYP24A1 protein levels were examined by Western blotting after 120 h of exposure to progesterone and calcitriol either alone or in combination. Progesterone and calcitriol-progesterone inhibited CYP24A1 levels in both clear cell lines. Calcitriol alone showed no effect on CYP24A1 expression (Figure 1B,C).
Progesterone and progesterone-calcitriol combination attenuated proliferation of ovarian endometrioid carcinoma by suppressing TGF-β signaling
The TOV-112D cells were cultured with various doses of progesterone (10–80 µM) and proliferation was inhibited in a dose-dependent manner with an IC50 of 25.48±2.54. Exposure of cells to calcitriol alone for 120 hours resulted in inhibition of cell growth and an IC50 of 34.18±3.39. Concurrent treatment of cells with progesterone and calcitriol produced a greater reduction in growth compared to single treatment with an IC50 of 18.22±1.98 and CI <0.74 (Figure 2A). Expression of TGF-β1, TGF-β2, TGF-βR1, TGF-βR2, total SMAD2/3 and pSMAD2/3 was attenuated in TOV-112D cells with progesterone alone and progesterone-calcitriol combination. There was no change in expression of TGF-β3, TGF-βR3 and SMAD4 (Figure 2B,C).
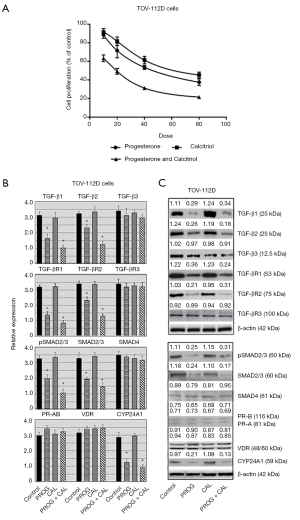
Effect of progesterone and calcitriol on the expression of PR, VDR and CYP24A1 in of ovarian endometrioid carcinoma
The effect of progesterone-calcitriol treatment was analyzed on the ovarian endometrioid carcinoma cell line, TOV-112D. The expression of PR and VDR was not affected by progesterone and calcitriol treatment. Expression of CYP24A1 in TOV-112D was markedly inhibited by progesterone alone and in combination with calcitriol (Figure 2B,C).
Progesterone and progesterone-calcitriol combination attenuated proliferation of ovarian papillary serous adenocarcinoma by suppressing TGF-β signaling
To investigate the cytotoxic effect of progesterone-calcitriol, OV-90 cells were exposed to different concentrations of progesterone or calcitriol ranging from 0 to 80 µM for 120 h. The MTS assay was used to determine the cell viability (Figure 3A). A dose-dependent attenuation of cell viability was noticed with progesterone and calcitriol. The IC50 values for progesterone and calcitriol were 30.42±2.11 and 46.35±4.50 respectively. The combination treatment synergistically enhanced growth inhibitory effects (IC50 21.30±3.16 and CI <0.45). Exposure of OV-90 cells to progesterone, calcitriol alone or calcitriol- progesterone combination exhibited reduced expression of TGF-β1, TGF-β2, TGF-βR1, TGF-βR2, pSMAD2/3 and total SMAD2/3. Expression of TGF-β3, TGF-βR3 and SMAD4 was not affected by any treatment (Figure 3B,C).
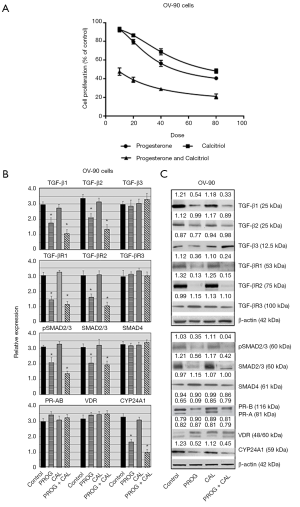
Effect of progesterone and calcitriol on the expression of PR, VDR and CYP24A1 in ovarian papillary serous adenocarcinoma
Treatment of the OV-90 cell line with progesterone alone or with progesterone-calcitriol combination inhibited expression of CYP24A1. There was no effect on the expression of PR-B and VDR. However, expression of PR-A was suppressed by progesterone and calcitriol-progesterone combination (Figure 3B,C).
Progesterone and calcitriol attenuated proliferation of DNA MMR deficient EC cell lines by suppressing TGF-β signaling
The effect of various doses of progesterone, calcitriol and their combination on the growth of two DNA MMR deficient cell (HEC-1A and HEC-59) lines was investigated. Both cell lines demonstrated a dose-dependent reduction (IC50 27.86±4.47 and 32.39±2.47 for HEC1A and HEC59, respectively) in cell viability after 120 hours of culture with progesterone. Simultaneous exposure of cells to progesterone and calcitriol resulted in further reduction (HEC-1A, IC50 22.43±2.57, CI <0.54; HEC-59, IC50 27±3.12, CI <0.48) of cell growth compared to progesterone alone treatment (Figure 4A). The expression of TGF-β ligands, TGF-β receptors and downstream signaling proteins were evaluated in HEC-1A and HEC-59 cell lines. In HEC-1A, a marked decrease of TGF-β1, TGF-βR1, total SMAD2/3, and pSMAD2/3 expression was seen following progesterone and progesterone-calcitriol combination. HEC-59 cell lines showed a similar response as HEC-1A, with the addition of TGF-β2 and TGF-βR2 suppression with progesterone-calcitriol treatment. Neither cell line showed changes in TGF-β3, TGF-βR3, or SMAD4 after treatment with progesterone and calcitriol (Figure 4B,C).
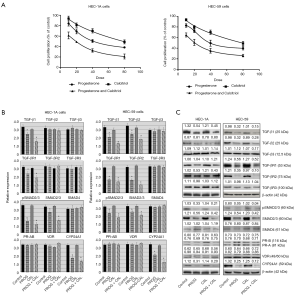
Effect of progesterone and calcitriol on the expression of PR, VDR and CYP24A1 in DNA MMR deficient EC cells
In both DNA MMR deficient cell lines, the expression of PR and VDR was not altered after treatment with progesterone and progesterone-calcitriol combination. CYP24A1 was markedly downregulated with progesterone and calcitriol-progesterone combination in HEC-1A and HEC-59 cell lines (Figure 4B,C).
Progesterone and calcitriol attenuated proliferation of ovarian cancer BRCA1 null cell ovarian cancer line by suppressing TGF-β signaling
The ovarian cancer cell line UWB1.289 was treated with various doses of progesterone, calcitriol or a combination of progesterone and calcitriol. Progesterone attenuated proliferation of cells in a dose-dependent manner and the IC50 was 27.93±1.85. Cells exposed to the combination of calcitriol and progesterone showed greater decrease (IC50 20.46±2.68 and CI <0.68) in cell number than either of the treatments alone (Figure 5A). The expression of TGF-β signaling components were analyzed in progesterone, calcitriol and progesterone-calcitriol treated ovarian cancer BRCA1 null ovarian cancer cells (Figure 5B). Progesterone and progesterone-calcitriol combination downregulated the expression of TGF-β1, TGF-β2, TGF-βR1, pSMAD2/3 and total SMAD2/3 in cells. No change in TGF-β3, TGF-βR3, and SMAD4 was observed (Figure 5B,C).

Effect of progesterone and calcitriol on the expression of PR, VDR and CYP24A1 in BRCA1 null ovarian cancer cells
The progesterone-calcitriol combination failed to alter the expression of PR and VDR in BRCA1 null cells. However, the expression of vitamin-D induced gene, CYP24A1, was attenuated with progesterone-calcitriol combination and progesterone alone (Figure 5B,C).
Discussion
Previously, our group showed that the combination of a low dose of progesterone with a low dose of calcitriol markedly inhibited growth of serous ovarian and EC cells. The mechanism for growth inhibition was by enhanced expression of the VDR, activation of caspase-3, induction of cell cycle arrest and downregulation of cyclins. Furthermore, our results revealed downregulation of TGF-β signaling proteins and CYP24A1, an enzyme that breaks down the active form of vitamin-D (14-16,20).
Ovarian and ECs are not single diseases but a compendium of diseases with distinct histologic subtypes, molecular alteration(s) and ecosystems of tumor cells, stromal and immune cells compositions (27-29). Owing to the heterogeneous nature of both cancers, it is expected that they might respond to the treatment in different ways. Thus, it is important to test whether the progesterone-calcitriol combination that successfully suppressed the growth of serous ovarian and endometrioid EC would be effective in attenuating growth of different cancer subtypes and those with various mutations. Analyzing the mechanistic activity of the progesterone and calcitriol combination on different subtypes of endometrial and ovarian cancer has the potential to increase our understanding of these cancers and may translate into expanded applications of the progesterone-calcitriol combination in clinical practice in chemopreventive and therapeutic settings.
TGF-β is a superfamily of cytokines with pleiotropic functions. It regulates a number of biological processes such as cell proliferation, differentiation, migration, survival, apoptosis, angiogenesis, extracellular matrix production and immune response (30,31). There are three homologous isoforms of TGF-β ligands (TGF-β1, TGF-β2 and TGF-β3). The ligands exercise their effects by binding to the TGF-βR2, which recruits the TGF-βR1. SMAD2 and 3 are phosphorylated by type I receptor, which in turn form heteromeric complexes with SMAD4. The activated SMAD complexes accumulate in the nucleus and bind to a specific promoter region on target genes along with transcription factors and/or co-activators/repressors (30,31). Our published work demonstrated an intact TGF-β pathway in EC cells. Progesterone markedly inhibited basal and TGF-β1-induced proliferation and invasive potential of EC cells. Furthermore, TGF-βR1 blocker (SD-208) abrogated TGF-β1 induced growth as well as progesterone induced growth inhibition. These results suggest that progesterone exerts its growth inhibitor effects via the TGF-β1/SMAD signaling pathway (20). Phosphorylation and subsequent translocation of SMAD2 and SMAD3 to the nucleus are crucial steps in TGF-β signal transduction. Western blotting revealed that the total and phosphorylated SMAD2/3 levels were reduced by progesterone and the combination of progesterone-calcitriol in all cell lines tested. This indicates that reduction of pSMAD2/3 is due to the decreased total-SMAD2/3. These findings are in concert with our previous immunofluorescence staining study (20) showing that TGF-β1 treatment of the EC cells increased and caused translocation of SMAD2/3 from the cytoplasm to the nucleus and treatment with progesterone decreased expression in the cytoplasm and the nucleus of cells.
Local levels of vitamin-D3 are maintained in the cells by a delicate balance between the activities of CYP27B1 and CYP24A1, which promote synthesis and deactivate vitamin-D3 respectively. CYP24A1 is a vitamin-D3 induced gene. Factors that modify the activity of CYP27B1 and CYP24A1 have the potential to impact vitamin D3 signaling. A number of microarray studies have shown induction of CYP24A1 and TGF-β signaling proteins in response to vitamin-D3 in prostate, colon, and breast cancer cells (32-34). Towsend et al. (33) showed that co-treatment with vitamin-D3 and TGF-β2 enhanced the accumulation of CYP24A1 further in the MCF-7 cells compared to cells treated with vitamin-D3 alone. The relationship between the TGF-β pathway and CYP24A1 has been further substantiated in prostate cancer and stromal cells. Treatment of cancer/stromal cells with TGF-β increased expression of CYP24A1, which metabolizes vitamin-D3 and thus reduces VDR activity. Knock down of a TGF-β-inducible nuclear receptor co-regulator also known as Hic-5, reduced basal VDR expression, vitamin-D3-induced CYP24A1 expression and TGF-β-enhanced CYP24A1 expression (34).
The main histological subtypes of ovarian and ECs are serous, endometrioid, clear cell, and mucinous adenocarcinoma. These subtypes reflect significant biological alterations in the behavior of tumors which demonstrate different phenotypes with distinct biological and genetic backgrounds (29,35). To develop treatment for cancer, it is crucial to test the efficacy of drugs on individual cancer subtypes to understand whether treatment is effective for a wide variety of cancers. In our previous studies, we prioritized evaluations of the effects of progesterone and calcitriol in the most common EC histologies, endometrioid adenocarcinoma and ovarian serous carcinoma, and discovered the mechanisms by which these two agents suppressed tumor growth. In this study, we extended our analysis to other ovarian and EC subtypes. The TGF-β signaling pathway is activated in ovarian and ECs as seen by high levels of TGF-β and pSMAD2/3 in different ovarian and endometrial cell lines (20,36). In the present study, the expression of TGF-β ligands, TGF-β receptors and SMADs were assessed in clear cell, endometrioid and papillary serous ovarian cancer cell lines exposed to progesterone, calcitriol and the combination of the two. All cancer subtypes showed high expression of TGF-β signaling proteins. These findings concur with earlier studies showing elevated expression of these proteins in ovarian clear cell, endometrioid and papillary serous cancers (37,38). Treatment of these subtypes of cancer with progesterone and combination of progesterone with calcitriol markedly inhibited the growth and the expression of TGF-β1, TGF-β2, TGF-βR1, TGF-βR2 and SMAD2/3. These results support the therapeutic use of progesterone-calcitriol combination as an effective strategy in suppressing growth of different histological subtypes of tumors by abrogating the expression of TGF-β signaling proteins.
Progesterone elicits action through PR and cancers with high PR expression have good prognosis compared to those with lower expression of PR (39). The cell lines used in the present study representing clear cell, endometrioid and papillary serous subtypes of ovarian tumors, express both forms of PR in varying levels depending on the cell line. A number of studies reported higher PR positivity in serous (58%) and endometrioid (76%) carcinoma compared to clear-cell (8%) carcinoma (40-42). Previously, we showed expression of PR-A and PR-B on serous ovarian and EC cells and demonstrated anti-proliferative actions of progesterone, primarily through the induction of apoptosis (14,15). We examined the effects of progesterone, calcitriol, or both on PR protein expression in cancer cell lines of different subtypes. No noticeable changes were observed in any cell line following progesterone, calcitriol, or combination treatments except OV-90, a papillary serous ovarian cancer cell line, where progesterone and combination suppressed PR-A expression. This observation indicates that reduced PR-A may have different functional outcomes, which remain to be investigated.
MMR deficient cells typically have many DNA mutations that lead to cancer. Alterations in the MMR pathway lead to high levels of microsatellite instability. Lately, it has been established that high levels of TGF-β induce genomic instability by impairing DNA repair. TGF-β has been shown to down-regulate the expression of MSH2 and ataxia telangiectasia mutated (ATM) (43-45), leading to an impaired DNA repair efficiency. The effect of progesterone and calcitriol on the HEC-1A cell line with the complete loss of MMR (hMSH6/hPMS2-defective), and HEC-59 with no hMSH2, was assessed. We found downregulation of TGF-β signaling proteins in both DNA MMR deficient EC cells and observed inhibition of growth with progesterone and calcitriol-progesterone combination treatments. These results suggest that calcitriol-progesterone may control growth of tumor cells by downregulating TGF-β signaling proteins.
Germline mutations of tumor suppressors BRCA1 and BRCA2 confers with an increased risk of developing breast and ovarian cancer (46-48). BRCAs participate in DNA damage repair via homologous recombination and impact genomic instability and malignant transformation (25,49). Treatment of UWB1.289 BRCA1 null cells with progesterone or calcitriol progesterone combination attenuated expression of TGF-β1, TGF-β2, TGF-βR1 and subsequently phosphorylated SMAD2/3. A link between BRCA1 and TGF-β1/SMAD pathway is well established. In breast cancer cells, interruption of endogenous BRCA1 in MCF-7 cell line changes their anti-proliferation responses, while maintenance of BRCA1 upholds TGF-β1 responsiveness through enhancing the stability of SMAD4 (50).
The CYP24A1 is upregulated in a number of cancers, including ovarian and endometrial, and impairs the activity of calcitriol (14,15). Here, we showed increased expression of CYP24A1 in endometrioid, clear cell, papillary serous carcinomas, endometrial tumors with DNA MMR deficiency and ovarian cancer with BRCA1/BRCA2 mutations. These findings indicate that cancer cells can evade the anti-tumorigenic effects of calcitriol by inducing the expression of CYP24A1. Moreover, progesterone inhibited the expression of CYP24A1 in not only serous ovarian and ECs, but also attenuated CYP24A1 expression in all types of cancer tested in this study. Similarly, recent studies have shown sensitization of cancer cells by inhibition of CYP24A1 using pharmacological inhibitors or genetic knockdown approaches (51,52). VDRs were expressed in all the cells lines tested. These results concur with investigations showing no significant differences in the expression of VDR in serous, mucinous, clear cell, and endometrioid subtypes of ovarian cancer (53). Previously, we have shown that progesterone upregulates the expression of VDR in serous EC cells and thus, enhances the anticancer effects of calcitriol (16). However, we have not seen upregulation of VDR in response to progesterone in any cell line tested, except ES-2 cells.
We acknowledge that in the current study we have used only one serous cell line. Our goal was to validate our findings in serous cancers to show the synergistic effect of progesterone and calcitriol combination on cell proliferation. Only one serous cancer cell line was commercially available at the time. Further studies will be performed to confirm the results of this study after procurement of more than one serous cancer cell lines from non-commercial sources.
In summary, our data reveal that the progesterone-calcitriol combination not only inhibited growth of different subtypes of endometrial and ovarian cancers, but also those with mutations in ARID1A or PIK3CA, DNA MMR deficiency or BRCA1 null status. Furthermore, in all cell lines of different histotypes, progesterone-calcitriol combination attenuated the expression of TGF-β signaling proteins and CYP24A1.
Collectively, these results underscore the potential expanded applications of the progesterone and calcitriol combination for further development as a chemopreventive and therapeutic strategy for endometrial and ovarian cancer, and the important role that surrogate biomarkers of TGF-β signaling proteins and CYP24A1 may play in future investigations of activity of this combination in preclinical model systems and human subjects.
Acknowledgments
Funding: This study was funded by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2019.07.36). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The institutional ethical approval and informed consent were waived.
Disclaimer: The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Uniformed Services University of the Health Sciences, the Department of the Air Force, the Department of the Army, the Department of the Navy, or the Department of Defense.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69:7-34. [Crossref] [PubMed]
- Richardson DL. New and novel therapies for gynecologic cancers. Semin Oncol Nurs 2019;35:217-9. [Crossref] [PubMed]
- Armitage M, Nooney J, Evans S. Recent concerns surrounding HRT. Clin Endocrinol (Oxf) 2003;59:145-55. [Crossref] [PubMed]
- Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. JAMA 2002;288:321-33. [Crossref] [PubMed]
- Shumaker SA, Legault C, Rapp SR, et al. Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women: the Women's Health Initiative Memory Study: a randomized controlled trial. JAMA 2003;289:2651-62. [Crossref] [PubMed]
- Gambacciani M, Monteleone P, Sacco A, et al. Hormone replacement therapy and endometrial, ovarian and colorectal cancer. Best Pract Res Clin Endocrinol Metab 2003;17:139-47. [Crossref] [PubMed]
- Brekelmans CT. Risk factors and risk reduction of breast and ovarian cancer. Curr Opin Obstet Gynecol 2003;15:63-8. [Crossref] [PubMed]
- Guo H, Guo J, Xie W, et al. The role of vitamin D in ovarian cancer: epidemiology, molecular mechanism and prevention. J Ovarian Res 2018;11:71. [Crossref] [PubMed]
- Bandera Merchan B, Morcillo S, Martin-Nuñez G, et al. The role of vitamin D and VDR in carcinogenesis: through epidemiology and basic sciences. J Steroid Biochem Mol Biol 2017;167:203-18. [Crossref] [PubMed]
- Jones G, Prosser DE, Kaufmann M. Cytochrome P450-mediated metabolism of vitamin D. J Lipid Res 2014;55:13-31. [Crossref] [PubMed]
- Sheng L, Turner AG, Barratt K, et al. Mammary-specific ablation of Cyp24a1 inhibits development, reduces proliferation and increases sensitivity to vitamin D. J Steroid Biochem Mol Biol 2019;189:240-7. [Crossref] [PubMed]
- Hu N, Zhang H. CYP24A1 depletion facilitates the antitumor effect of vitamin D3 on thyroid cancer cells. Exp Ther Med 2018;16:2821-30. [PubMed]
- Swami S, Krishnan AV, Wang JY, et al. Dietary vitamin D3 and 1,25-dihydroxyvitamin D3 (calcitriol) exhibit equivalent anticancer activity in mouse xenograft models of breast and prostate cancer. Endocrinology 2012;153:2576-87. [Crossref] [PubMed]
- Bokhari AA, Lee LR, Raboteau D, et al. Progesterone potentiates the growth inhibitory effects of calcitriol in endometrial cancer via suppression of CYP24A1. Oncotarget 2016;7:77576-90. [Crossref] [PubMed]
- Rodriguez GC, Turbov J, Rosales R, et al. Progestins inhibit calcitriol-induced CYP24A1 and synergistically inhibit ovarian cancer cell viability: an opportunity for chemoprevention. Gynecol Oncol 2016;143:159-67. [Crossref] [PubMed]
- Lee LR, Teng PN, Nguyen H, et al. Progesterone enhances calcitriol antitumor activity by upregulating vitamin D receptor expression and promoting apoptosis in endometrial cancer cells. Cancer Prev Res (Phila) 2013;6:731-43. [Crossref] [PubMed]
- Syed V. TGF-β signaling in cancer. J Cell Biochem 2016;117:1279-87. [Crossref] [PubMed]
- Ahmadi A, Najafi M, Farhood B, et al. Transforming growth factor-β signaling: tumorigenesis and targeting for cancer therapy. J Cell Physiol 2019;234:12173-87. [Crossref] [PubMed]
- Miyazono K, Katsuno Y, Koinuma D, et al. Intracellular and extracellular TGF-β signaling in cancer: some recent topics. Front Med 2018;12:387-411. [Crossref] [PubMed]
- Bokhari AA, Lee LR, Raboteau D, et al. Progesterone inhibits endometrial cancer invasiveness by inhibiting the TGFβ pathway. Cancer Prev Res (Phila) 2014;7:1045-55. [Crossref] [PubMed]
- Kroeger PT Jr, Drapkin R. Pathogenesis and heterogeneity of ovarian cancer. Curr Opin Obstet Gynecol 2017;29:26-34. [Crossref] [PubMed]
- Yabushita H, Hirata M, Noguchi M, et al. Vitamin D receptor in endometrial carcinoma and the differentiation-inducing effect of 1,25-dihydroxyvitamin D3 on endometrial carcinoma cell lines. J Obstet Gynaecol Res 1996;22:529-39. [Crossref] [PubMed]
- Chou TC. Drug combination studies and their synergy quantification using the Chou-Talalay method. Cancer Res 2010;70:440-6. [Crossref] [PubMed]
- Drabsch Y, ten Dijke P. TGF-β signalling and its role in cancer progression and metastasis. Cancer Metastasis Rev 2012;31:553-68. [Crossref] [PubMed]
- Li D, Kang N, Ji J, et al. BRCA1 regulates transforming growth factor-β (TGF-β1) signaling through Gadd45a by enhancing the protein stability of Smad4. Mol Oncol 2015;9:1655-66. [Crossref] [PubMed]
- Piestrzeniewicz-Ulanska D, Brys M, Semczuk A, et al. Expression of TGF-beta type I and II receptors in normal and cancerous human endometrium. Cancer Lett 2002;186:231-9. [Crossref] [PubMed]
- Beaufort CM, Helmijr JC, Piskorz AM, et al. Ovarian cancer cell line panel (OCCP): clinical importance of in vitro morphological subtypes. PLoS One 2014;9:e103988. [Crossref] [PubMed]
- Hussein YR, Soslow RA. Molecular insights into the classification of high-grade endometrial carcinoma. Pathology 2018;50:151-61. [Crossref] [PubMed]
- Bosse T, Nout RA, McAlpine JN, et al. Molecular classification of grade 3 endometrioid endometrial cancers identifies distinct prognostic subgroups. Am J Surg Pathol 2018;42:561-8. [PubMed]
- Colak S, Ten Dijke P. Targeting TGF-β signaling in cancer. Trends Cancer 2017;3:56-71. [Crossref] [PubMed]
- Haque S, Morris JC. Transforming growth factor-β: a therapeutic target for cancer. Hum Vaccin Immunother 2017;13:1741-50. [Crossref] [PubMed]
- Krishnan AV, Shinghal R, Raghavachari N, et al. Analysis of vitamin D-regulated gene expression in LNCaP human prostate cancer cells using cDNA microarrays. Prostate 2004;59:243-51. [Crossref] [PubMed]
- Towsend K, Trevino V, Falciani F, et al. Identification of VDR-responsive gene signatures in breast cancer cells. Oncology 2006;71:111-23. [Crossref] [PubMed]
- Solomon JD, Heitzer MD, Liu TT, et al. VDR activity is differentially affected by Hic-5 in prostate cancer and stromal cells. Mol Cancer Res 2014;12:1166-80. [Crossref] [PubMed]
- Ramalingam P. Morphologic, immunophenotypic, and molecular features of epithelial ovarian cancer. Oncology (Williston Park) 2016;30:166-76. [PubMed]
- Hirschhorn T, Barizilay L, Smorodinsky NI, et al. Differential regulation of Smad3 and of the type II transforming growth factor-β receptor in mitosis: implications for signaling. PLoS One 2012;7:e43459. [Crossref] [PubMed]
- Leslie KK, Stein MP, Kumar NS, et al. Progesterone receptor isoform identification and subcellular localization in endometrial cancer. Gynecol Oncol 2005;96:32-41. [Crossref] [PubMed]
- Huvila J, Talve L, Carpén O, et al. Progesterone receptor negativity is an independent risk factor for relapse in patients with early stage endometrioid endometrial adenocarcinoma. Gynecol Oncol 2013;130:463-9. [Crossref] [PubMed]
- Diep CH, Daniel AR, Mauro LJ, et al. Progesterone action in breast, uterine, and ovarian cancers. J Mol Endocrinol 2015;54:R31-53. [Crossref] [PubMed]
- Chen S, Dai X, Gao Y, et al. The positivity of estrogen receptor and progesterone receptor may not be associated with metastasis and recurrence in epithelial ovarian cancer. Sci Rep 2017;7:16922. [Crossref] [PubMed]
- Yu Y, Wang Y, Ren X, et al. Context-dependent bidirectional regulation of the MutS homolog 2 by transforming growth factor β contributes to chemoresistance in breast cancer cells. Mol Cancer Res 2010;8:1633-42. [Crossref] [PubMed]
- Huang SM, Lu KT, Wang YC. ATM/ATR and SMAD3 pathways contribute to 3-indole-induced G1 arrest in cancer cells and xenograft models. Anticancer Res 2011;31:203-8. [PubMed]
- Oda K, Tanikawa M, Sone K, et al. Recent advances in targeting DNA repair pathways for the treatment of ovarian cancer and their clinical relevance. Int J Clin Oncol 2017;22:611-8. [Crossref] [PubMed]
- Mavaddat N, Peock S, Frost D, et al. Cancer risks for BRCA1 and BRCA2 mutation carriers: results from prospective analysis of EMBRACE. J Natl Cancer Inst 2013;105:812-22. [Crossref] [PubMed]
- Girolimetti G, Perrone AM, Santini D, et al. BRCA-associated ovarian cancer: from molecular genetics to risk management. Biomed Res Int 2014;2014:787143. [Crossref] [PubMed]
- Pan Z, Xie X. BRCA mutations in the manifestation and treatment of ovarian cancer. Oncotarget 2017;8:97657-70. [PubMed]
- Roy R, Chun J, Powell SN. BRCA1 and BRCA2: different roles in a common pathway of genome protection. Nat Rev Cancer 2011;12:68-78. [Crossref] [PubMed]
- Aparicio T, Baer R, Gautier J. DNA double-strand break repair pathway choice and cancer. DNA Repair (Amst) 2014;19:169-75. [Crossref] [PubMed]
- Luo W, Hershberger PA, Trump DL, et al. 24-Hydroxylase in cancer: impact on vitamin D-based anticancer therapeutics. J Steroid Biochem Mol Biol 2013;136:252-7. [Crossref] [PubMed]
- Jeon SM, Shin EA. Exploring vitamin D metabolism and function in cancer. Exp Mol Med 2018;50:20. [Crossref] [PubMed]
- Luo W, Yu WD, Ma Y, et al. Inhibition of protein kinase CK2 reduces Cyp24a1 expression and enhances 1,25-dihydroxyvitamin D (3) antitumor activity in human prostate cancer cells. Cancer Res 2013;73:2289-97. [Crossref] [PubMed]
- Sun H, Jiang C, Cong L, et al. CYP24A1 inhibition facilitates the antiproliferative effect of 1,25(OH)2D3 through downregulation of the WNT/β-catenin pathway and methylation-mediated regulation of CYP24A1 in colorectal cancer cells. DNA Cell Biol 2018;37:742-9. [Crossref] [PubMed]
- Clendenen TV, Arslan AA, Koenig KL, et al. Vitamin D receptor polymorphisms and risk of epithelial ovarian cancer. Cancer Lett 2008;260:209-15. [Crossref] [PubMed]


