
Clinical outcomes of proximal gastrectomy versus total gastrectomy for locally advanced proximal gastric cancer: a propensity score matching analysis
Introduction
Gastric cancer remains a worldwide cancer with the third most frequent cause of cancer-related deaths (1). Although the overall incidence of gastric cancer has been declining in Western and Eastern countries, the incidence of carcinoma of the upper-third of the stomach has been increasing at an alarming rate (2-4). Furthermore, cancer-related mortality of proximal is higher than other sites of stomach (5). Given these characteristics of proximal gastric cancer (PGC), the optimal surgical selection has received considerable attention.
For early PGC, proximal gastrectomy (PG) has been generally accepted by most surgeons for its oncological radicality and safety (6-15). However, concerning to locally advanced PGC (LAPGC), it still has not reached a consensus. Proponents (10,16,17) of PG have argued that PG can achieve an equivalent overall survival (OS) compared to total gastrectomy (TG), whereas others (18,19) showed that TG was associated with better 5-year OS. Moreover, there was no clinical outcome of clinical randomized trial targeting the same issue.
Given the suggested but undecided survival differences between PG and TG, the aim of our study was to compare the clinicopathologic features, surgical and survival outcomes for LAPGC patients with either PG or with TG based on the China National Cancer Center Gastric Cancer Database (NCCGCDB), in order to provide evidences for the development of guiding strategies for LAPGC patients.
Methods
Patient population
All the study data were abstracted from the NCCGCDB. The NCCGCDB was a clinical gastric cancer database based on a huge retrospective cohort, which was sourced from China National Cancer Center, a single but large-volume institution, and included more than 19,000 patients from all around China 1998 to 2018. LAPGC was defined as clinical stage IB–III (according to the eighth edition of the International Union against Cancer Classification) with the epicenter located in cardia (C16.0) or fundus (C16.1). The extent of gastric resection, TG or PG, was dictated by tumor size and epicenter, tumor stage, the potential volume of the future remnant stomach, and surgeon’s preference. Finally, 2,737 PG patients and 181 TG patients were identified during 1998 to 2018 year. This study was approved by the ethics committee of National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (No. 17-156/1412), and informed consent was taken from all patients.
Statistical analyses
Patient demographics and clinical characteristics between PG and TG groups were compared with t-test for continuous variables with normal distribution and chi-square test for categorical variables.
Given the inherent differences between patients in PG and TG groups, we calculated a propensity score for following variables: gender, age, smoking, drinking, HER2 score, H. pylori infection, Lauren classification, histologic type, linitis plastica, nerve invasion, vascular invasion, pTNM, adjuvant therapies, BMI and no. of lymph nodes metastasis. The propensity score was estimated using a logit model. Matching was performed using a 1:1 optimal matching method with 0.2 of caliper value, which yielded 150 pairs of TG and PG patients. Surgical and OS outcomes after surgery were compared within the propensity-score matched cohorts. Three- and five-year OS rates were calculated with the Kaplan-Meier method and compared by Z test. The differences of OS during the whole follow-up period between two groups were assessed using the log-rank test when two survival curves didn’t cross otherwise using two-stage hazard rate comparison method (20). To find risk predictors of all-cause mortality in the matched population, the following variables were evaluated in a univariate model: gender, age, smoking, drinking, HER2 score, H. pylori infection, Lauren classification, histologic type, linitis plastica, nerve invasion, vascular invasion, pTNM stage, surgical margin, adjuvant therapies. Then, hazard ratio (HR) and 95% confidence interval (CI) were calculated by a multivariate analysis using the Cox proportional hazard regression model.
A P value less than 0.05 was considered statistically significant and all tests were two-sided. Statistical analysis was performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA) and Rstudio (RStudio, Inc., Boston, MA, USA).
Results
Clinicopathologic characteristics
In this study, 2,918 patients were included. The clinicopathologic features of 181 patients (6.20%) with TG and 2,737 patients (93.80%) with PG were compared (Table 1). Clearly, a higher PG proportion was found in the LAPGC in China National Cancer Center. The median follow-up times were 62.7±3.5 months in PG group and 45.9±5.6 months in TG groups.
Table 1
| Characteristics | Overall (N=2,918) | Propensity score matched (N=300)1 | |||||
|---|---|---|---|---|---|---|---|
| TG group (N=181) | PG group (N=2,737) | P value | TG group (N=150) | PG group (N=150) | P value | ||
| Gender, n (%) | 0.67 | 1.00 | |||||
| Male | 150 (82.87) | 2,301 (84.07) | 127 (84.67) | 127 (84.67) | |||
| Female | 31 (17.13) | 436 (15.93) | 23 (15.33) | 23 (15.33) | |||
| Age, n (%) | 0.04 | 1.00 | |||||
| <50 | 26 (14.36) | 276 (10.08) | 21 (14.00) | 21 (14.00) | |||
| 50–64 | 96 (53.04) | 1,360 (49.69) | 82 (54.67) | 82 (54.67) | |||
| 65–74 | 54 (29.83) | 919 (33.58) | 42 (28.00) | 42 (28.00) | |||
| ≥75 | 5 (2.76) | 182 (6.65) | 5 (3.33) | 5 (3.33) | |||
| Smoking history, n (%) | 0.002 | 0.91 | |||||
| Yes | 76 (41.99) | 1,525 (55.72) | 66 (44.00) | 69 (46.00) | |||
| No | 104 (57.46) | 1,199 (43.81) | 83 (55.33) | 80 (53.33) | |||
| Unknown | 1 (0.55) | 13 (0.47) | 1 (0.67) | 1 (0.67) | |||
| Alcohol intake history, n (%) | 0.41 | 0.78 | |||||
| Yes | 70 (38.67) | 1,196 (43.70) | 61 (40.67) | 67 (44.67) | |||
| No | 110 (60.77) | 1,530 (55.90) | 88 (58.67) | 82 (54.67) | |||
| Unknown | 1 (0.55) | 11 (0.40) | 1 (0.67) | 1 (0.67) | |||
| HER2 score, n (%) | <0.001 | 0.80 | |||||
| Negative | 77 (42.54) | 635 (23.20) | 68 (45.33) | 74 (49.33) | |||
| Positive+ | 40 (22.10) | 616 (22.51) | 32 (21.33) | 24 (16.00) | |||
| Positive++ | 18 (9.94) | 266 (9.72) | 17 (11.33) | 18 (12.00) | |||
| Positive+++ | 13 (7.18) | 178 (6.50) | 9 (6.00) | 11 (7.33) | |||
| Unknown | 33 (18.23) | 1,042 (38.07) | 24 (16.00) | 23 (15.33) | |||
| H. pylori infection, n (%) | 0.06 | 0.69 | |||||
| Negative | 22 (12.15) | 200 (7.31) | 18 (12.00) | 19 (12.67) | |||
| Positive | 10 (5.52) | 157 (5.74) | 8 (5.33) | 5 (3.33) | |||
| Unknown | 149 (82.32) | 2,380 (86.96) | 124 (82.67) | 126 (84.00) | |||
| Lauren, n (%) | <0.001 | 0.99 | |||||
| Diffuse type | 56 (30.94) | 318 (11.62) | 47 (31.33) | 47 (31.33) | |||
| Intestinal type | 34 (18.78) | 768 (28.06) | 32 (21.33) | 34 (22.67) | |||
| Mixed type | 45 (24.86) | 390 (14.25) | 40 (26.67) | 39 (26.00) | |||
| Unknown | 46 (25.41) | 1,261 (46.07) | 31 (20.67) | 30 (20.00) | |||
| Histologic type, n (%) | <0.001 | 0.07 | |||||
| Well | 7 (3.87) | 149 (5.44) | 4 (2.67) | 3 (2.00) | |||
| Moderately | 24 (13.26) | 827 (30.22) | 23 (15.33) | 11 (7.33) | |||
| Poorly | 140 (77.35) | 1,668 (60.94) | 123 (82.00) | 136 (90.67) | |||
| Undifferentiated, anaplastic | 0 | 1 (0.04) | 0 | 0 | |||
| Unknown | 10 (5.52) | 92 (3.36) | |||||
| Linitis plastica, n (%) | 0.15 | 1.00 | |||||
| Yes | 2 (1.10) | 7 (0.26) | 1 (0.67) | 1 (0.67) | |||
| No | 179 (98.90) | 2,716 (99.23) | 149 (99.33) | 149 (99.33) | |||
| Unknown | 0 | 14 (0.51) | – | – | |||
| Nerve invasion, n (%) | <0.001 | 0.64 | |||||
| Yes | 94 (51.93) | 914 (33.39) | 83 (55.33) | 79 (52.67) | |||
| No | 85 (46.96) | 1,793 (65.51) | 67 (44.67) | 71 (47.33) | |||
| Unknown | 2 (1.10) | 30 (1.10) | |||||
| Vascular invasion, n (%) | 0.006 | 0.93 | |||||
| Yes | 83 (45.86) | 948 (34.64) | 68 (45.33) | 71 (47.33) | |||
| No | 94 (51.93) | 1,744 (63.72) | 80 (53.33) | 77 (51.33) | |||
| Unknown | 4 (2.21) | 45 (1.64) | 2 (1.33) | 2 (1.33) | |||
| pT, n (%) | 0.24 | 0.02 | |||||
| T0 | 0 | 0 | 0 | 0 | |||
| T1 | 5 (2.76) | 36 (1.32) | 5 (3.33) | 1 (0.67) | |||
| T2 | 18 (9.94) | 355 (12.97) | 11 (7.33) | 16 (10.67) | |||
| T3 | 91 (50.28) | 1,413 (51.63) | 80 (53.33) | 99 (66.00) | |||
| T4 | 67 (37.02) | 933 (34.09) | 54 (36.00) | 34 (22.67) | |||
| pN, n (%) | 0.04 | 0.08 | |||||
| N0 | 53 (29.28) | 877 (32.04) | 46 (30.67) | 29 (19.33) | |||
| N1 | 40 (22.10) | 795 (29.05) | 33 (22.00) | 37 (24.67) | |||
| N2 | 34 (18.78) | 472 (17.25) | 30 (20.00) | 27 (18.00) | |||
| N3 | 54 (29.83) | 593 (21.67) | 41 (27.33) | 57 (38.00) | |||
| pM, n (%) | – | – | |||||
| M0 | 181 (100.00) | 2,737 (100.00) | 150 (100.00) | 150 (100.00) | |||
| M1 | 0 | 0 | 0 | 0 | |||
| pTNM, n (%) | 0.44 | 0.43 | |||||
| Ib | 13 (7.18) | 246 (8.99) | 9 (6.00) | 8 (5.33) | |||
| II | 67 (37.02) | 1,089 (39.79) | 59 (39.33) | 49 (32.67) | |||
| III | 101 (55.80) | 1,402 (51.22) | 82 (54.67) | 93 (62.00) | |||
| Adjuvant therapies, n (%) | <0.001 | 0.45 | |||||
| Multimodality treatment | 98 (54.14) | 1,018 (37.19) | 75 (50.00) | 65 (43.33) | |||
| Surgery only | 10 (5.52) | 258 (9.43) | 9 (6.00) | 8 (5.33) | |||
| Unknown | 73 (40.33) | 1,461 (53.38) | 66 (44.00) | 77 (51.33) | |||
| BMI, kg/m2 (mean ± SD)* | 23.6±3.5 | 24.1±3.4 | 0.08 | 23.8±3.4 | 23.8±3.5 | 0.92 | |
| No. of lymph nodes metastasis, median [quantiles]* | 2 [0–10] | 2 [0–6] | 0.02 | 2 [0–8] | 4 [1–9] | 0.07 | |
*, some patients had missing values. 1, Propensity score matched for gender, age, smoking, drinking, HER2 score, H. pylori infection, Lauren classification, histologic type, linitis plastica, nerve invasion, vascular invasion, pTNM, adjuvant therapies, BMI and no. of lymph nodes metastasis. TG, total gastrectomy; PG, proximal gastrectomy.
Compared to TG groups, patients in the PG group were more likely to be older age (≥65 years, 40.23% vs. 32.59%, P=0.04), smoking history (55.72% vs. 41.99%, P=0.002), and intestinal type (28.06% vs. 18.78%, P<0.001). Patients in TG group were also more likely to have more HER2 negative (42.54% vs. 23.20%, P<0.001), nerve invasion (51.93% vs. 33.39%, P<0.001), vascular invasion (45.86% vs. 34.64%, P=0.006), and to be in later pN stage (N2 and N3, 48.61% vs. 38.92%, P=0.04). In addition, the metastasis rate of the total number of resected lymph nodes was significantly higher in the TG group compared to PG group (P=0.02).
After propensity score matching, 150 matched pairs for PG vs. TG were selected. Patients who underwent PG were also more likely to be in earlier pT stage (pT4, 22.67% vs. 36.00%, P=0.02) comparing with TG group. As for other clinicopathologic characteristics, there was no significant difference between the two groups (P>0.05) (Table 1).
Surgical outcomes after propensity score matching
The surgical outcomes after propensity score matching of LAPGC patients undergoing PG and TG were detailed in Table 2. No significant differences between the two groups in negative surgical margin (92.67% vs. 97.33%, P=0.158), postoperative mortality (0.67% vs. 0.67%, P=1.00) and postoperative stay (12 vs. 11 days, P=0.64). A higher proportion of open gastrectomy (97.33% vs. 69.33%, P<0.001) and a lower proportion of laparoscopy-assisted gastrectomy (1.33% vs. 26.00%, P<0.001) was showed in PG patients than TG group. When compared with TG group, PG group was associated with shorter operative time (181.8±49.8 vs. 213.5±66.7 min, P<0.001). The mean estimated blood transfusion of the PG group was 235 mL less than that of TG group (743.8±296.6 vs. 978.4±421.1 mL, P=0.049). However, the no. of retrieved lymph nodes (34.3±17.0 vs. 24.2±11.0, P<0.001) in TG group was larger than PG.
Table 2
| Surgical outcomes | TG group (N=150) | PG group (N=150) | P value |
|---|---|---|---|
| Surgical margin, n (%) | 0.158 | ||
| Negative | 139 (92.67) | 146 (97.33) | |
| Positive | 9 (6.00) | 3 (2.00) | |
| Unknown | 2 (1.33) | 1 (0.67) | |
| Operative approach, n (%) | <0.001 | ||
| Open | 104 (69.33) | 146 (97.33) | |
| Laparoscopy-assisted | 39 (26.00) | 2 (1.33) | |
| Conversion to laparotomy | 1 (0.67) | 1 (0.67) | |
| Total laparoscopy | 4 (2.67) | 1 (0.67) | |
| Unknown | 2 (1.33) | 0 | |
| Blood transfusion, n (%) | 0.001 | ||
| Yes | 34 (22.67) | 15 (10.00) | |
| No | 94 (62.67) | 123 (82.00) | |
| Unknown | 22 (14.67) | 12 (8.00) | |
| Postoperative mortality, n (%) | 1.000 | ||
| Yes | 1 (0.67) | 1 (0.67) | |
| No | 148 (98.67) | 148 (98.67) | |
| Unknown | 1 (0.67) | 1 (0.67) | |
| Estimated blood transfusion, mL, mean ± SD* | 978.4±421.1 | 743.8±296.6 | 0.049 |
| No. of retrieved lymph nodes, mean ± SD | 34.3±17.0 | 24.2±11.0 | <0.001 |
| Operative time, min, mean ± SD* | 213.5±66.7 | 181.8±49.8 | <0.001 |
| Postoperative stay, days, median [quantiles]* | 12 [10–14] | 11 [10–13] | 0.644 |
| Total expenses, yuan, median (quantiles)* | 103,631.9 (87,613.2–127,005.8) | 78,506.8 (71,550.6–97,969.2) | <0.001 |
*, some patients had missing values. TG, total gastrectomy; PG, proximal gastrectomy.
Survival outcomes after propensity score matching
Kaplan-Meier survival curves of LAPGC patients following PG and TG were showed in Table 3 and Figure 1A. Although the OS rates following PG and TG had no statistically significant differences during the long-term follow-up period (P=0.62), the 3- and 5-year OS rates (79.1% vs. 77.2% and 74.5% vs. 72.0%, respectively, both P<0.001) in PG group were slightly higher than ones in TG group. Concerning to detailed group for stage, PG patients of stage II only had a higher 5-year OS rate (85.7% vs. 81.7%, P<0.001) while ones of stage III showed both improved 3- and 5-year OS rates (73.3% vs. 65.2% and 68.8% vs. 62.4%, respectively, both P<0.001) (Figure 1B,C, Table 3). After controlling for confounding variables (Table 4), the multivariable results from Cox proportional hazards regression analysis also showed that the extent of resection had no impact on the long-term OS status (HR: 1.172, 95% CI: 0.916–1.499, P=0.208), even stratified into stage II and III (Tables S1,S2).
Table 3
| The resection types | N | Mean of OS (95% CI) | 3-year OS rate (%) | 5-year OS rate (%) |
|---|---|---|---|---|
| LAPGC | ||||
| PG | 150 | 158.8 (140.5–177.1) | 79.1 | 74.5 |
| TG | 150 | 112.4 (102.0–122.8) | 77.2 | 72.0 |
| Stage II | ||||
| PG | 49 | 157.7 (127.1–188.4) | 91.0 | 85.7 |
| TG | 59 | 125.9 (112.2–139.6) | 90.3 | 81.7 |
| Stage III | ||||
| PG | 93 | 155.7 (136.0–175.4) | 73.3 | 68.8 |
| TG | 82 | 98.4 (83.1–113.7) | 65.2 | 62.4 |
LAPGC: two stage hazard rate comparison, P=0.2826; 3- and 5-year OS rates: P<0.0001; Stage II: two stage hazard rate comparison, P=0.3372; 3-year OS rates: P=0.36; 5-year OS rates: P<0.0001; Stage III: log-rank chi-square =1.3760, P=0.2408; 3- and 5-year OS rates: P<0.0001. OS, overall survival; LAPGC, locally advanced proximal gastric cancer; PG, proximal gastrectomy; TG, total gastrectomy.
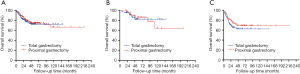
Table 4
| Prognostic factors | Number | n, % | Unadjusted | Adjusted1 | |||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||||
| Gender | |||||||
| Male | 254 | 56 (22.0) | 1 | 1 | |||
| Female | 46 | 17 (37.0) | 1.843 (1.071–3.173) | 0.027 | 1.723 (0.832–3.571) | 0.143 | |
| Age | |||||||
| <50 | 42 | 15 (35.7) | 1 | 1 | |||
| 50–64 | 164 | 36 (22.0) | 0.595 (0.325–1.086) | 0.091 | 0.935 (0.473–1.849) | 0.848 | |
| 65–74 | 84 | 19 (22.6) | 0.593 (0.301–1.166) | 0.130 | 0.941 (0.433–2.046) | 0.878 | |
| ≥75 | 10 | 3 (30.0) | 0.749 (0.217–2.587) | 0.647 | 1.394 (0.354–5.482) | 0.635 | |
| Smoking | |||||||
| Yes | 135 | 28 (20.7) | 0.824 (0.512–1.326) | 0.425 | 1.22 (0.640–2.324) | 0.546 | |
| No | 163 | 44 (27.0) | 1 | 1 | |||
| Unknown | 2 | 1 (50.0) | 2.386 (0.327–17.429) | 0.391 | 5.378 (0.467–62) | 0.177 | |
| Drinking | |||||||
| Yes | 128 | 27 (21.1) | 0.82 (0.509–1.324) | 0.418 | 1.165 (0.618–2.196) | 0.636 | |
| No | 170 | 45 (26.5) | 1 | 1 | |||
| Unknown | 2 | 1 (50.0) | 2.391 (0.328–17.449) | 0.390 | – | – | |
| HER2 score | |||||||
| Negative | 142 | 29 (20.4) | 1 | 1 | |||
| Positive+ | 56 | 11 (19.6) | 0.943 (0.471–1.889) | 0.869 | 1.415 (0.680–2.941) | 0.353 | |
| Positive++ | 35 | 7 (20.0) | 0.949 (0.416–2.168) | 0.902 | 0.929 (0.360–2.398) | 0.879 | |
| Positive+++ | 20 | 9 (45.0) | 2.656 (1.256–5.616) | 0.011 | 5.038 (2.164–11.725) | 0.000 | |
| Unknown | 47 | 17 (36.2) | 1.435 (0.777–2.652) | 0.249 | 0.958 (0.378–2.428) | 0.927 | |
| H. pylori infection | |||||||
| Negative | 37 | 3 (8.1) | 1 | 1 | |||
| Positive | 13 | 3 (23.1) | 3.701 (0.746–18.361) | 0.109 | 9.453 (1.555–57.467) | 0.015 | |
| Unknown | 250 | 67 (26.8) | 3.408 (1.072–10.839) | 0.038 | 3.543 (0.924–13.585) | 0.065 | |
| Lauren | |||||||
| Intestinal type | 66 | 8 (12.1) | 1 | 1 | |||
| Diffuse type | 94 | 27 (28.7) | 2.636 (1.197–5.803) | 0.016 | 2.218 (0.905–5.439) | 0.082 | |
| Mixed type | 79 | 16 (20.3) | 1.822 (0.779–4.257) | 0.166 | 1.620 (0.649–4.045) | 0.301 | |
| Unknown | 61 | 22 (36.1) | 2.553 (1.127–5.782) | 0.025 | 3.964 (1.322–11.885) | 0.014 | |
| Histologic type | |||||||
| Well | 7 | 0 | |||||
| Moderately | 34 | 5 (14.7) | 1 | 1 | |||
| Poorly | 259 | 68 (26.3) | 1.969 (0.794–4.885) | 0.144 | 1.952 (0.688–5.537) | 0.209 | |
| Linitis plastica | |||||||
| Yes | 2 | 2 (100.0) | 15.025(3.522–64.107) | <0.001 | 10.263 (1.896–55.557) | 0.007 | |
| No | 298 | 71 (23.8) | 1 | 1 | |||
| Nerve invasion | |||||||
| Yes | 162 | 37 (22.8) | 1.018 (0.639–1.621) | 0.940 | 1.145 (0.656–1.998) | 0.634 | |
| No | 138 | 36 (26.1) | 1 | 1 | |||
| Vascular invasion | |||||||
| Yes | 139 | 34 (24.5) | 1.115 (0.701–1.773) | 0.646 | 0.737 (0.431–1.262) | 0.267 | |
| No | 157 | 38 (24.2) | 1 | 1 | |||
| Unknown | 4 | 1 (25.0) | 1.350 (0.185–9.87) | 0.767 | 1.258 (0.136–11.655) | 0.840 | |
| pTNM | |||||||
| I | 17 | 2 (11.8) | 0.855 (0.196–3.72) | 0.834 | 0.878 (0.188–4.105) | 0.869 | |
| II | 108 | 16 (14.8) | 1 | 1 | |||
| III | 175 | 55 (31.4) | 2.651 (1.518–4.632) | 0.001 | 2.621 (1.415–4.855) | 0.002 | |
| Surgical margin | |||||||
| Negative | 285 | 67 (23.5) | 1 | 1 | |||
| Positive | 12 | 4 (33.3) | 1.559 (0.568–4.277) | 0.389 | 0.986 (0.31–3.138) | 0.981 | |
| Unknown | 3 | 2 (66.7) | 2.468 (0.603–10.096) | 0.209 | 3.032 (0.588–15.632) | 0.185 | |
| Surgery type | |||||||
| PG | 150 | 37 (24.7) | 1 | 1 | |||
| TG | 150 | 36 (24.0) | 1.060 (0.842–1.334) | 0.620 | 1.172 (0.916–1.499) | 0.208 | |
1, Adjust for gender, age, smoking, drinking, HER2, H. pylori infection, Lauren, histologic type, plastica, nerve invasion, vascular invasion, TNM, surgical margin, complex therapies and surgery type. OS, overall survival; PG, proximal gastrectomy; TG, total gastrectomy.
Prognostic factors of survival in univariate and multivariate analyses
As shown in Table 4, univariate analyses of LAPGC patients revealed significantly different survival based on the following parameters: gender, HER2 positive (+++), diffuse type, linitis plastica, and pTNM stage. When appropriate significant factors were taken into consideration, multivariate analysis revealed HER2 positive (+++), H. pylori infection, linitis plastica and pTNM stage were independent predictors for poor prognosis.
Discussion
To date, we found that only two large-scale randomized trials (Trial registration number: NCT01433861 and NCT02892643) targeting the same issue are currently underway, and surgeons are awaiting the results. Realistically, many surgeons are now actively applying PG to LAPGC. To our best knowledge, our analysis represented the largest evaluations of outcomes for LAPGC patients undergoing PG or TG. A major finding of our study was that PG was an optional surgical procedure of LAPGC treatment for its better 3-, 5-year survival rates when compared to TG.
In this large retrospective cohort study from the NCCGCDB, the number of patients varies significantly between the two groups, with an incidence of TG: PG = 1: 16. There were some possible reasons for this quantitative difference. Firstly, more and more studies have proved that TG was not always necessary for LAPGC (10,16,17,21-23). Secondly, surgeons from China National Cancer Center have enough ability to finish the technically demanding for PG surgery. Respect to clinicopathologic characteristics, we found TG patients appeared to more lymph node spread, nerve invasion, lymphatic vessel invasion and vascular invasion before propensity score matching, which was also observed in two published studies (17,24). This may a considerable factor for these patients underwent TG approach. Therefore, we performed a strict propensity match to eliminate the bias.
The extent of lymphadenectomy was a consideration when TG and PG are compared. Our study showed that the mean retrieved lymph nodes of TG group were ten lymph nodes more than that of PG group, which was in accordance with most studies targeting this issues (13,25-28). Therefore, TG did enable a more complete nodal dissection and it was apparent from the number of lymph nodes retrieved in the current study that TG did result in a somewhat better lymph node yield. Although TG can provide more complete lymphadenectomy, the correlation between clinical survival for LAPGC patients of these factors still needs further study. Yura et al. (29) following 202 LAPGC patients indicated that the metastatic rate of these lymph nodes was really low (#4d, 0.99%; #5, 0% and #6, 0%), while the nodes with high metastatic rate for PGC, like #3, #2 and #1, were included in PG. This study also approved that oncological safety would be ensured by PG, without the need for TG when targeting for nodal dissection.
PG has long been thought to confer worse prognosis. A published study from Korea with 147 patients reported that individuals with pathological stage III gastric cardiac cancer, the 5-year survival of the TG was significantly higher than that of the PG group (38.4% vs. 17.1%, P=0.04) (24). Ying et al. compared the two groups for PGC patients with stage I–III and also demonstrated PG and TG groups had significantly different 5-year OS (45.2 vs. 50.9%, P=0.047) (19). However, a recent study for LAPGC patients including neoadjuvant chemotherapy revealed that the overall 2-year survival following PG and TG was 73.8% and 49.9%, respectively, and not statistically different (P=0.10), which might show the important role of chemotherapy for LAPGC patients survival outcomes (16). In our study, 3-, 5-year survival rates in PG group were slightly higher than ones in TG group, which might indicate that PG was a preferable approach for LAPGC patients. After propensity score matching in this study, a primary finding was that TG was not independently associated with OS when compared with PG even stratified by AJCC stage. Furthermore, PG was not a negative prognostic indicator in multivariate analysis.
Strengths and limitations should be considered when interpreting the study results. One limitation of this study was that it was retrospective and just conducted in a single institution, so the results might not represent the whole Chinese population. The second limitation was that postoperative function and patient quality of life following PG or TG was neither evaluated nor documented well. The study also had several strengths. Firstly, to date, this cohort was the largest to compare the long-term survival outcomes between PG and TG. Secondly, we used a propensity score matching analysis to reduce bias, which was considered to mimic randomized controlled trials.
Conclusions
In conclusion, the extent of resection for LAPGC patients did not influence the long-term OS outcomes. Moreover, future randomized clinical trials of quality of life following PG or TG are expected to assist surgeons in the choice of surgical approach and strategy for LAPGC patients.
Table S1
| Prognostic factors | Number | n, % | Unadjusted | Adjusted1 | |||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||||
| The resection types | |||||||
| PG | 49 | 8 (16.3) | 1 | 1 | |||
| TG | 59 | 8 (13.6) | 1.015 (0.621–1.659) | 0.952 | 1.329 (0.713–2.478) | 0.371 | |
1, adjust for gender, age, smoking, drinking, HER2 score,
Table S2
| Prognostic factors | Number | n, % | Unadjusted | Adjusted1 | |||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||||
| The resection types | |||||||
| PG | 93 | 27 (29.0) | 1 | 1 | |||
| TG | 82 | 28 (34.1) | 1.171 (0.898–1.528) | 0.243 | 1.196 (0.889–1.608) | 0.236 | |
1, adjust for gender, age, smoking, drinking, HER2 score,
Acknowledgments
All authors made substantial contributions to the intellectual content of this paper.
Funding: This study was funded in part by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2020.02.38). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the ethics committee of National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (No. 17-156/1412). Written informed consent was obtained from the patient for publication of this study and any accompanying images. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 2019;144:1941-53. [Crossref] [PubMed]
- Deans C, Yeo MS, Soe MY, et al. Cancer of the gastric cardia is rising in incidence in an Asian population and is associated with adverse outcome. World J Surg 2011;35:617-24. [Crossref] [PubMed]
- Carr JS, Zafar SF, Saba N, et al. Risk factors for rising incidence of esophageal and gastric cardia adenocarcinoma. J Gastrointest Cancer 2013;44:143-51. [Crossref] [PubMed]
- Steevens J, Botterweck AA, Dirx MJ, et al. Trends in incidence of oesophageal and stomach cancer subtypes in Europe. Eur J Gastroenterol Hepatol 2010;22:669-78. [PubMed]
- Crew KD, Neugut AI. Epidemiology of gastric cancer. World J Gastroenterol 2006;12:354-62. [Crossref] [PubMed]
- An JY, Youn HG, Choi MG, et al. The difficult choice between total and proximal gastrectomy in proximal early gastric cancer. Am J Surg 2008;196:587-91. [Crossref] [PubMed]
- Kitamura K, Yamaguchi T, Okamoto K, et al. Total gastrectomy for early gastric cancer. J Surg Oncol 1995;60:83-8. [Crossref] [PubMed]
- Kaibara N, Nishimura O, Nishidoi H, et al. Proximal gastrectomy as the surgical procedure of choice for upper gastric carcinoma. J Surg Oncol 1987;36:110-2. [Crossref] [PubMed]
- Ikeguchi M, Kader A, Takaya S, et al. Prognosis of patients with gastric cancer who underwent proximal gastrectomy. Int Surg 2012;97:275-9. [Crossref] [PubMed]
- Nozaki I, Hato S, Kobatake T, et al. Long-term outcome after proximal gastrectomy with jejunal interposition for gastric cancer compared with total gastrectomy. World J Surg 2013;37:558-64. [Crossref] [PubMed]
- Ichikawa D, Komatsu S, Kubota T, et al. Long-term outcomes of patients who underwent limited proximal gastrectomy. Gastric Cancer 2014;17:141-5. [Crossref] [PubMed]
- Isobe T, Hashimoto K, Kizaki J, et al. Reconstruction methods and complications in proximal gastrectomy for gastric cancer, and a comparison with total gastrectomy. Kurume Med J 2014;61:23-9. [Crossref] [PubMed]
- Son MW, Kim YJ, Jeong GA, et al. Long-term outcomes of proximal gastrectomy versus total gastrectomy for upper-third gastric cancer. J Gastric Cancer 2014;14:246-51. [Crossref] [PubMed]
- Hosoda K, Yamashita K, Katada N, et al. Potential benefits of laparoscopy-assisted proximal gastrectomy with esophagogastrostomy for cT1 upper-third gastric cancer. Surg Endosc 2016;30:3426-36. [Crossref] [PubMed]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 2011;14:113-23. [Crossref] [PubMed]
- Sugoor P, Shah S, Dusane R, et al. Proximal gastrectomy versus total gastrectomy for proximal third gastric cancer: total gastrectomy is not always necessary. Langenbecks Arch Surg 2016;401:687-97. [Crossref] [PubMed]
- Rosa F, Quero G, Fiorillo C, et al. Total vs proximal gastrectomy for adenocarcinoma of the upper third of the stomach: a propensity-score-matched analysis of a multicenter western experience (On behalf of the Italian Research Group for Gastric Cancer-GIRCG). Gastric Cancer 2018;21:845-52. [Crossref] [PubMed]
- Zhao D, Xu H, Li K, et al. Prognostic factors for patients after curative resection for proximal gastric cancer. J Huazhong Univ Sci Technolog Med Sci 2010;30:530-5. [Crossref] [PubMed]
- Ying KM, Chen Z, Dang CX, et al. Clinicopathology and survival in patients with gastroesophageal reflux after radical surgery of proximal gastric cancer. Dig Dis Sci 2018;63:1035-42. [Crossref] [PubMed]
- Qiu P, Sheng J. A two-stage procedure for comparing hazard rate functions. J R Stat Soc Series B Stat Methodol 2008;70:191-208.
- Erturk MS, Ciçek Y, Ersan Y, et al. Analysis of clinicopathological prognostic parameters in adenocarcinoma of the gastric cardia. Acta Chir Belg 2003;103:611-5. [Crossref] [PubMed]
- Yoo CH, Sohn BH, Han WK, et al. Long-term results of proximal and total gastrectomy for adenocarcinoma of the upper third of the stomach. Cancer Res Treat 2004;36:50-5. [Crossref] [PubMed]
- Harrison LE, Karpeh MS, Brennan MF. Total gastrectomy is not necessary for proximal gastric cancer. Surgery 1998;123:127-30. [Crossref] [PubMed]
- Kim JH, Park SS, Kim J, et al. Surgical outcomes for gastric cancer in the upper third of the stomach. World J Surg 2006;30:1870-6; discussion 1877-8.
- Hayami M, Hiki N, Nunobe S, et al. Clinical outcomes and evaluation of laparoscopic proximal gastrectomy with double-flap technique for early gastric cancer in the upper third of the stomach. Ann Surg Oncol 2017;24:1635-42. [Crossref] [PubMed]
- Kosuga T, Ichikawa D, Komatsu S, et al. Feasibility and nutritional benefits of laparoscopic proximal gastrectomy for early gastric cancer in the upper stomach. Ann Surg Oncol 2015;22:S929-35. [Crossref] [PubMed]
- Jung DH, Lee Y, Kim DW, et al. Laparoscopic proximal gastrectomy with double tract reconstruction is superior to laparoscopic total gastrectomy for proximal early gastric cancer. Surg Endosc 2017;31:3961-9. [Crossref] [PubMed]
- Yoo CH, Sohn BH, Han WK, et al. Proximal gastrectomy reconstructed by jejunal pouch interposition for upper third gastric cancer: prospective randomized study. World J Surg 2005;29:1592-9. [Crossref] [PubMed]
- Yura M, Yoshikawa T, Otsuki S, et al. Oncological safety of proximal gastrectomy for T2/T3 proximal gastric cancer. Gastric Cancer 2019;22:1029-35. [Crossref] [PubMed]


