
Serum gamma-glutamyl transpeptidase-to-platelet ratio (GPR) can predict the prognosis of hepatocellular carcinoma: a meta-analysis and systematic review
Introduction
In China, hepatocellular carcinoma (HCC) is one of the most common malignancies, with high morbidity and mortality. Its onset is hidden, the early clinical symptoms are not obvious, and the imaging and pathological diagnosis are mostly in the middle and late stages. Rapid disease progression and high mortality are its characteristics, and the 5-year survival rate is less than 10%. The key to liver cancer prevention and treatment lies in early diagnosis and precise treatment. Therefore, it is essential to establish an early diagnosis system. Alpha-fetoprotein (AFP) is currently the most widely used HCC marker. Serum tumor marker detection has the advantages of convenient specimen collection and no risk of tumor spread caused by invasive procedures and has been commonly used in clinical practice. However, many HCC patients with chronic liver disease also show elevated AFP. Similarly, some HCC patients continue to have negative AFP, indicating that AFP is less sensitive (1).
Recent studies show that gamma-glutamyl transpeptidase-to-platelet ratio (GPR) is an effective indicator of chronic hepatic fibrosis with chronic viral hepatitis-B (2). Pang et al. (3) designed this indicator for the first time and used it to predict the preoperative survival rate of HCC patients. Gamma-glutamyl transpeptidase (GGT) mostly exists in hepatocytes (4) and it helps hepatocytes decrease the oxidation products produced during normal metabolism, and it can serologically indicate liver injury (5). Platelet count in patients with liver cirrhosis is an important indicator of the degree of liver cirrhosis. Severe liver cirrhosis accompanied by portal hypertension causes hypersplenism, which lowers platelet levels (6). In addition, studies have shown that elevated serum GGT levels are closely related to the occurrence of HCC (7). Platelets can promote the production of liver tumor cells through derived factors. For example, platelet-derived growth factor C (PDGF-C) can stimulate the high expression of PDGF-C receptors on HSC cell membranes, accelerate HSC activation, and induce liver cell carcinogenesis and proliferation. HCC cells can release IL-6 to stimulate the expression of thrombopoietin (TPO) and induce platelet increase. On the other hand, vascular endothelial growth factor (VEGF) and endothelial cells activate protein kinase signaling pathways through phosphorylation, activate the corresponding receptors on the surface, and ultimately induce endothelial cell proliferation and activation, promote the formation of new blood vessels, and accelerate tumor cell metastasis (8). GPR has been proven to be one of the independent risk factors for HCC (9). Recent studies have shown that GPR is one of the indicators suggesting liver fibrosis in patients with chronic HBV infection. The severity of liver fibrosis increases with the increase of the GPR value. Preoperative liver reserve function is an important indicator of HCC survival. The previous study only conducted a correlation study on the GPR of HCC patients before surgery, the smaller the value of GPR, indicating a better prognosis (10). Due to the small size of the sample of GPR related clinical studies, randomised controlled clinical studies are lacking, and the results of these studies are not consistent. To this end, we made up for these shortcomings through meta-analysis, and conducted a systematic review and consistency evaluation of the original research results. Therefore, the relationship between GPR and HCC prognosis is also of great significance (10). We summarized the ability of GPR to assess the overall prognosis of HCC patients. Our goal is to eliminate the publication bias of previous articles and determine the value of GPR in predicting HCC. Here, we are trying to determine the critical importance of GPR for predicting the prognosis of HCC. We present the following article in accordance with the PRISMA reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-21-2559/rc).
Methods
Search strategies
Use the online databases PubMed, Embase, Web of Science and China national knowledge infrastructure (CNKI) to select all relevant articles from the beginning of this study to October 30, 2021. The search terms are limited to the following main terms: “gamma-glutamyl transpeptidase to platelet ratio” or “gamma-glutamyl transferase to platelet ratio” or “GPR”, and “hepatocellular carcinoma” or “liver cancer” or “liver neoplasm” or “hepatic neoplasm” or “hepatocellular cancer” or “HCC”.
Inclusion and exclusion criteria
The inclusion criteria of the screening literature are as follows: (I) the content of the study is to evaluate the value of GPR in the predictive diagnosis of liver cancer; (II) cases are clearly diagnosed with a pathological gold standard for HCC; (III) the research design is divided into case group and control group; (IV) HCC patients can be extracted from the research results: true positive (TP), true negative (TN), false positive (FP), and false negative (FN) of GPR in serum were used to construct a 2×2 four-grid table.
The literature search excluded studies involving: (I) studies that were not randomized controlled clinical trials; (II) studies involving patients with too many complications that may cause uncertain measurements; (III) studies with incomplete data or lacking full text; (IV) any conference papers, reviews, case reports, studies on lessons learned, and repetitive literature (for multilingual papers, only the earliest version was used); (V) nonalcoholic fatty liver disease; (VI) patients with liver genetic metabolic diseases; (VII) patients with liver metastasis; (VIII) patients with acute heart failure, pregnancy or combined tuberculosis and acute malaria; (IX) patients who do not meet radical resection or high tumor-node-metastasis (TNM) staging (stage IV); (X) patients undergoing preoperative chemotherapy, radiotherapy, or other anticancer treatment; (XI) HCC patients with tumour number ≥2, tumour satellite lesions, or other organ tumours; (XII) clinically confirmed infections, haematological diseases or immune disorders; (XIII) postoperative pathological diagnosis of non-HCC cases; (XIV) incomplete clinical and follow-up data; (XV) perioperative death; (XVI) loss of contact during follow-up. Follow-up examinations included computerized tomography/magnetic resonance imaging, abdominal ultrasound, and serological examination.
Data extraction
Two researchers, HM and NW, independently screened the literature and evaluated the quality of the selected literature. Extract the following information: first author’s name, publication year, country, number of patients, age, gender, cut-off value, TNM stage, survival outcome, follow-up duration and TP, FP, TN, FN.
Quality assessment
Two researchers, NW and KS, evaluated the literature’s quality based on the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) standard tool (11). There are 14 questions in the standard, and each item can be rated as “yes” or 1 point, and “unclear” and “no” as 0 points. If the researchers disagree, discuss and resolve.
Statistical analysis
The data extraction of the figure is carried out using GetData 2.26 software. We use RevMan5.2 to screen the literature quality evaluation and use Stata16.0 to calculate the combined sensitivity, specificity, positive likelihood ratio (PLR), negative likelihood ratio (NLR) and diagnostic odds ratio (DOR) and draw the forest map and summarize the receiver operating characteristic curve SROC; statistical heterogeneity was quantified by I2 statistic. We drew Fagan charts using STATA 16.1 to determine the prior (current incidence) and posterior (estimated incidence after this diagnostic test). Draw Deek’s funnel chart to assess publication bias. P<0.05 indicates that the difference is statistically significant.
Results
Study selection
Among the 865 articles identified, 45 articles were screened out after full-text screening. Of these, 7 studies (3,12-17) involving 1,952 patients met inclusion criteria. No articles were added after evaluating the reference lists. We then extracted information from the 7 trials for meta-analyses. A flow chart of the literature search is shown in Figure 1.
Study characteristics
All included articles were published between 2016 and 2017, and a total of 7 studies were included. All studies used pathology as the gold standard for diagnosis. Use the 14 criteria in the QUADAS-2 quality assessment tool to assess the quality of the documents. The average quality score was >4, indicating that the quality of the literature was good. In terms of adaptability, all the literature is low risk, and the included literature has good adaptability. The essential characteristics and details of the 7 qualified articles and the QUADAS-2 score are shown in Table 1, and the scores of each dimension are shown in Figure 2.
Table 1
| Study | Year | Country | Cut off value | Cancer stage* | TP | FP | TN | FN | QUADAS-2 |
|---|---|---|---|---|---|---|---|---|---|
| Peng (3) | 2016 | China | GPR ≥0.76, GPR <0.76 | NA | 54 | 39 | 55 | 34 | 8 |
| Dong (13) | 2021 | China | GPR ≥0.54, GPR <0.54 | NA | 49 | 6 | 22 | 24 | 9 |
| Dai (12) | 2020 | China | GPR ≥0.35, GPR <0.35 | I–IV | 112 | 30 | 78 | 82 | 9 |
| Wang (14) | 2016 | China | GPR ≥0.84, GPR <0.84 | NA | 106 | 34 | 115 | 102 | 11 |
| Yang (15) | 2021 | China | GPR ≥0.30, GPR <0.30 | IV | 99 | 70 | 85 | 41 | 9 |
| Zhang (16) | 2017 | China | GPR ≥0.38, GPR <0.38 | I–IV | 118 | 66 | 125 | 59 | 9 |
| Wu (17) | 2021 | China | GPR ≥0.48, GPR <0.48 | I–IV | 112 | 53 | 116 | 66 | 8 |
*, malignant tumors classified according the TNM stage. TP, true positive; TN, true negative; FP, false positive; FN, false negative; QUADAS-2, Quality Assessment of Diagnostic Accuracy Studies; GPR, gamma-glutamyl transpeptidase-to-platelet ratio; TNM, tumor-node-metastasis.
Diagnostic accuracy evaluation
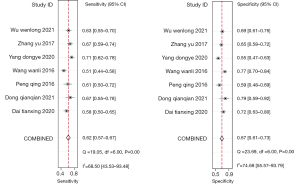
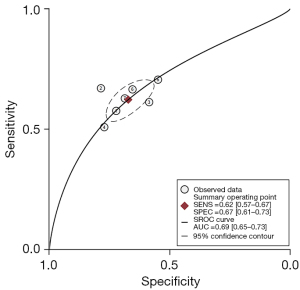
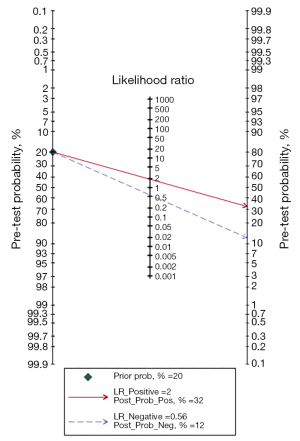
Meta-analysis results show (Figure 3), GPR predicts the prognosis of HCC with a moderate sensitivity of 0.62 and a specificity of 0.67 (95% CI: 0.57–0.67 and 0.61–0.73, respectively, NLR is 0.56 (95% CI: 0.51–0.62), PLR is 2.0 (95% CI: 1.7–2.2), DOR is 3 (95% CI: 3–4), SROC curve analysis revealed an area under the curve (AUC) of 0.69 (0.65–0.73), indicating the value of prognostic prediction of GPR on HCC (Figure 4). The Fagan plot (Figure 5) suggests that the post-test positive predictive value of the patient’s GPR for predicting HCC is 32%, which is significantly higher than that before the test.
Heterogeneity
The heterogeneity I2 of sensitivity analysis was 68.5%, and the Q test of sensitivity analysis showed P<0.001, indicating that the included studies were heterogeneous. After referring to the included articles, we summarized the possible sources of heterogeneity: (I) the changes of pathological stages in patients included in the study were from NA to IV; (II) different groups are included; (III) the cut-off value of GPR set by different studies is quite different. We take heterogeneity into account when conducting the data synthesis.
Publication bias
Analysis of publication bias using STATA 16.1 (Deek’s funnel plot) did not reveal obvious publication bias (P=0.48) in the included study (Figure 6).
Discussion
As shown in previous studies, 90% of primary liver cancer is HCC. It is the primary pathological subtype of liver cancer and the three most common causes of cancer-related deaths worldwide. The poor prognosis of liver cancer is due to the high rate of recurrence and metastasis. The main risk factors include genetics, epigenetic changes, chronic hepatitis B, hepatitis C virus infection, aflatoxin exposure, smoking, obesity, and diabetes (18). Some patients with early-stage liver cancer have not yet confirmed the diagnosis before determining the best treatment strategy and may therefore lose the opportunity to cure HCC (19). In the past few decades, the methods of treating liver cancer have been continuously improved. However, HCC biomarkers used for monitoring and early diagnosis have not been significantly improved clinically. These biomarkers have clinical effects on both prognosis and treatment response. Therefore, it is essential to screen other new biomarkers through proteomics, metabolomics, and genomics to evaluate liver cancer (20).
AFP is one of the most widely used biomarkers in liver cancer patients. The level of AFP in chronic HCV patients is significantly increased, resulting in low sensitivity in specific populations (21). Lens culinaris lectin-responsive AFP (AFP-L3) is one of the subtypes of AFP. Researchers have found that the serum AFP-L3 level of HCC patients is specific, and the average value is higher than that of patients with chronic liver disease. However, AFP-L3 is not perfect in diagnosing HCC, and the low sensitivity is still controversial (22). Golgi glycoprotein 73 (GP73) is a transmembrane Golgi glycoprotein. The serum GP73 of HCC patients is significantly increased, the sensitivity of GP73 is 60%, and the specificity is 77%. The same problem as AFP, GP73, may also be elevated in the serum of patients with benign liver tumors. Therefore, the significance of the GP73 test is still controversial. It cannot distinguish between primary malignant and benign liver tumors, and it cannot give a valuable hint to the prognosis of HCC patients (23). Des-γ-carboxyprothrombin, which is known as DCP, is an aberrant prothrombin protein. The result in shows that although Serum DCP has low diagnostic sensitivity, it yields reasonable specificity for HCC, which is around 81% to 98% (24). In practice, combining various related biomarkers to perform the test can vastly improve the corresponding sensitivity and specificity. The best combination of diagnostic methods can improve the prognosis of patients and guide future research. Appropriate combined diagnostic methods may improve the prognosis of patients and guide future research (16). Previous work has proved that for those HCC patients, combining AFP, AFP-L3 and DCP can significantly improve their diagnostic sensitivity and specificity (25).
In recent years, a large number of studies have shown that noninvasive serological prognostic prediction models have made significant progress in assessing fibrosis and cirrhosis of patients with chronic hepatitis. Some models are used to evaluate the prognosis of HCC and have high accuracy (26-29). Lemoine et al. (30) found that GPR has high diagnostic value for chronic hepatitis B fibrosis and cirrhosis. Subsequent studies further verified its high accuracy for chronic hepatitis B cirrhosis (31). GPR can be used to assess the degree of fibrosis and cirrhosis of hepatitis B-related chronic hepatitis (8). Its prognostic evaluation of hepatitis B-related HCC also shows a specific value, especially for HCC patients receiving TACE, local ablation or systemic treatment. GPR is based on the basic clinical serological examination calculation, which has the advantages of convenient inspection, good repeatability, and is conducive to the promotion and use of primary medical institutions (32).
GPR has the advantages of simple examination, good repeatability and good diagnostic performance, which is suitable for clinical application (12). In this study, we evaluated 7 studies, including a total of 1,952 patients, and confirmed the predictive value of GPR in predicting HCC. This study revealed that the specificity and sensitivity of GPR in predicting HCC prognosis were 0.62 and 0.67, which are higher than the values we set before. This proves that GPR is highly accurate in predicting HCC prognosis. SROC curve analysis revealed an AUC of 0.69 (0.65–0.73). Suggesting the same effect as the ROC curve: GPR can help predict patients’ prognosis with HCC.
This study has certain limitations. First, we included data from different populations. The differences in age and course of disease lead to large differences in the degree of hepatocyte lesions in patients, which brings great heterogeneity to this review. We tried stratified analysis, but eventually balanced the relationship between sample size and heterogeneity. Second, the data included in the studies are not all positive, which may be related to the uncertainty of the physiological mechanism of liver cell lesions. And this suggested that even in the positive population, GPR changes may be different from the manifestations. Third, the critical values of positive outcomes set by different studies vary a lot. Therefore, the specificity of GPR in some patients may be overestimated or underestimated. In order to obtain more definitive conclusions, more studies using the same implementation standard and standardized patients are needed to provide more exact evidence.
Conclusions
In short, in HCC patients, GPR can be used as a marker to predict the prognosis of HCC, allowing clinicians to do it in advance in a simple way at work. A prediction is made, however, a large number of high-quality multi-center studies are still needed for further verification.
Acknowledgments
Funding: This study is supported by
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-21-2559/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-21-2559/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang K, Lu Z, Li L, et al. Construction of a ceRNA network and a genomic-clinicopathologic nomogram to predict survival for HBV-related HCC. Hum Cell 2021;34:1830-42. [Crossref] [PubMed]
- Spoto B, D'Arrigo G, Tripepi G, et al. Serum gamma-glutamyltransferase, oxidized LDL and mortality in the elderly. Aging Clin Exp Res 2021;33:1393-7. [Crossref] [PubMed]
- Pang Q, Bi JB, Wang ZX, et al. Simple models based on gamma-glutamyl transpeptidase and platelets for predicting survival in hepatitis B-associated hepatocellular carcinoma. Onco Targets Ther 2016;9:2099-109. [Crossref] [PubMed]
- Hanigan MH. Gamma-glutamyl transpeptidase: redox regulation and drug resistance. Adv Cancer Res 2014;122:103-41. [Crossref] [PubMed]
- Zilkens C, Friese J, Köller M, et al. Hepatic failure after injury - a common pathogenesis with sclerosing cholangitis? Eur J Med Res 2008;13:309-13. [PubMed]
- Ziol M, Nault JC, Aout M, et al. Intermediate hepatobiliary cells predict an increased risk of hepatocarcinogenesis in patients with hepatitis C virus-related cirrhosis. Gastroenterology 2010;139:335-43.e2. [Crossref] [PubMed]
- Bao M, Zhu Q, Aji T, et al. Development of Models to Predict Postoperative Complications for Hepatitis B Virus-Related Hepatocellular Carcinoma. Front Oncol 2021;11:717826. [Crossref] [PubMed]
- Xue TC, Ge NL, Xu X, et al. High platelet counts increase metastatic risk in huge hepatocellular carcinoma undergoing transarterial chemoembolization. Hepatol Res 2016;46:1028-36. [Crossref] [PubMed]
- Luo D, Li H, Hu J, et al. Development and Validation of Nomograms Based on Gamma-Glutamyl Transpeptidase to Platelet Ratio for Hepatocellular Carcinoma Patients Reveal Novel Prognostic Value and the Ratio Is Negatively Correlated With P38MAPK Expression. Front Oncol 2020;10:548744. [Crossref] [PubMed]
- Wang RQ, Zhang QS, Zhao SX, et al. Gamma-glutamyl transpeptidase to platelet ratio index is a good noninvasive biomarker for predicting liver fibrosis in Chinese chronic hepatitis B patients. J Int Med Res 2016;44:1302-13. [Crossref] [PubMed]
- Whiting PF, Rutjes AW, Westwood ME, et al. A systematic review classifies sources of bias and variation in diagnostic test accuracy studies. J Clin Epidemiol 2013;66:1093-104. [Crossref] [PubMed]
- Dai T, Deng M, Ye L, et al. Prognostic value of combined preoperative gamma-glutamyl transpeptidase to platelet ratio and fibrinogen in patients with HBV-related hepatocellular carcinoma after hepatectomy. Am J Transl Res 2020;12:2984-97. [PubMed]
- Dong J, Wang Y. Relationship between γ-glutamyl transpeptidase to platelet ratio index and prognosis of hepatitis B related hepatocellular carcinoma. Chin J Lab Diagn 2021;25:860-4.
- Wang WL, Zheng XL, Zhang ZY, et al. Preoperative γ-glutamyl transpeptidase to platelet ratio (GPR) is an independent prognostic factor for HBV-related hepatocellular carcinoma after curative hepatic resection. Medicine (Baltimore) 2016;95:e4087. [Crossref] [PubMed]
- Yang D, Wu H, Nong W, et al. A new model based on gamma-glutamyl transpeptidase to platelet ratio (GPR) predicts prognostic outcome after curative resection of solitary hepatocellular carcinoma. Clin Res Hepatol Gastroenterol 2021;45:101509. [Crossref] [PubMed]
- Zhang Y, Wu L, Ma L, et al. Relationship between preoperative serum γ-glutamyl transpeptidase/platelet ratio index and prognosis of patients with HBV-related hepatocellular carcinoma after operation. Journal of Tianjin Medical 2017;45:489-92.
- Wu W, Wang Q, Han D, et al. Prognostic value of preoperative inflammatory markers in patients with hepatocellular carcinoma who underwent curative resection. Cancer Cell Int 2021;21:500. [Crossref] [PubMed]
- Wang J, Li H, Xia C, et al. Downregulation of CENPK suppresses hepatocellular carcinoma malignant progression through regulating YAP1. Onco Targets Ther 2019;12:869-82. [Crossref] [PubMed]
- Llovet JM, Montal R, Sia D, et al. Molecular therapies and precision medicine for hepatocellular carcinoma. Nat Rev Clin Oncol 2018;15:599-616. [Crossref] [PubMed]
- Piñero F, Dirchwolf M, Pessôa MG. Biomarkers in Hepatocellular Carcinoma: Diagnosis, Prognosis and Treatment Response Assessment. Cells 2020;9:1370. [Crossref] [PubMed]
- Wong RJ, Ahmed A, Gish RG. Elevated alpha-fetoprotein: differential diagnosis - hepatocellular carcinoma and other disorders. Clin Liver Dis 2015;19:309-23. [Crossref] [PubMed]
- Yi X, Yu S, Bao Y. Alpha-fetoprotein-L3 in hepatocellular carcinoma: a meta-analysis. Clin Chim Acta 2013;425:212-20. [Crossref] [PubMed]
- Bröker ME, Ijzermans JN, Witjes CD, et al. The predictive value of Golgi protein 73 in differentiating benign from malignant liver tumors. PLoS One 2014;9:e100187. [Crossref] [PubMed]
- Grizzi F, Franceschini B, Hamrick C, et al. Usefulness of cancer-testis antigens as biomarkers for the diagnosis and treatment of hepatocellular carcinoma. J Transl Med 2007;5:3. [Crossref] [PubMed]
- Zhao Y, Gao Q, Pei L, et al. Current status and future prospects of biomarkers in the diagnosis of hepatocellular carcinoma. Int J Biol Markers 2017;32:e361-9. [Crossref] [PubMed]
- Zheng J, Zhou Z, Xu Z, et al. Serum microRNA-125a-5p, a useful biomarker in liver diseases, correlates with disease progression. Mol Med Rep 2015;12:1584-90. [Crossref] [PubMed]
- Zuo D, Chen L, Liu X, et al. Combination of miR-125b and miR-27a enhances sensitivity and specificity of AFP-based diagnosis of hepatocellular carcinoma. Tumour Biol 2016;37:6539-49. [Crossref] [PubMed]
- Zhu F, Jiang Y, Luo F, et al. Effectiveness of localized ultrasound-targeted microbubble destruction with doxorubicin liposomes in H22 mouse hepatocellular carcinoma model. J Drug Target 2015;23:323-34. [Crossref] [PubMed]
- Zhou Q, He Q, Liang LJ. Expression of p27, cyclin E and cyclin A in hepatocellular carcinoma and its clinical significance. World J Gastroenterol 2003;9:2450-4. [Crossref] [PubMed]
- Lemoine M, Shimakawa Y, Nayagam S, et al. The gamma-glutamyl transpeptidase to platelet ratio (GPR) predicts significant liver fibrosis and cirrhosis in patients with chronic HBV infection in West Africa. Gut 2016;65:1369-76. [Crossref] [PubMed]
- Zoulim F, Durantel D. Antiviral therapies and prospects for a cure of chronic hepatitis B. Cold Spring Harb Perspect Med 2015;5:a021501. [Crossref] [PubMed]
- Zhu YF, Tan YF, Xu X, et al. Gamma-glutamyl transpeptidase-to-platelet ratio and the fibrosis-4 index in predicting hepatitis B virus-related hepatocellular carcinoma development in elderly chronic hepatitis B patients in China: A single-center retrospective study. Medicine (Baltimore) 2019;98:e18319. [Crossref] [PubMed]





