
Multifocal primary intracranial yolk sac tumor in an adult patient: a case report and literature review
Introduction
Yolk sac tumor (YST) is a type of germ cell tumor. It commonly arises in the gonads but sometimes can occur outside the gonads. Primary intracranial YST is sporadic, and multifocal primary intracranial YST is even rare. It is always located in the pineal, suprasellar and posterior third ventricular region (1). Because of the low incidence rate, such lesion has not been well documented. Here we report a case of multifocal primary intracranial YSTs, besides pineal and suprasellar regions, one mass located at the left temporal lobe. Then we review the literature and discuss the diagnosis and treatment of such lesions. We present the following case in accordance with the CARE reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-21-2561/rc).
Case presentation
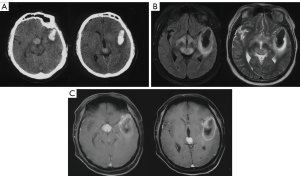
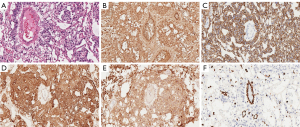
A 29 years old male patient was admitted to our department due to a sudden coma and a history of headaches for one month. Biochemistry of the blood revealed a raised alpha-fetoprotein concentration of 55.80 ng/mL (the expected value should be <20 ng/mL). Computed Tomography and magnetic resonance imaging of the head showed three massed located at the suprasellar region, pineal region and left temporal lobe separately (Figure 1). The mass at the left temporal lobe was successfully resected with emergency surgery, and decompressive craniectomy was also performed. Intraoperative findings revealed that the tumor was a solid mass with intra-tumoral hemorrhage and the blood supply was very rich. The pathology examination confirmed the diagnosis of yolk sac tumor (Figure 2). Hematoxylin and eosin staining clearly showed the Schiller-Duval body. Immunohistochemistry examination showed it was postive for alpha-fetoprotein (AFP), pan-cytokeratin (CK-PAN), LIN28, placental alkaline phosphatase (PLAP) and Vimentin (Figure 2). Postoperatively Computed Tomography of the chest and abdomen was uneventful. The final diagnosis was a multifocal primary intracranial yolk sac tumor. The patient's state of consciousness did not improve significantly after the surgery. Whole-brain radiotherapy was performed after the operation, and the patient died in a local hospital 11 months after the surgery. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the legal guardian for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Germ cell tumors (GCTs) are classified as extragonadal if there is no evidence of a primary tumor in either the testes or the ovaries. According to previous report, Asian children tend to develop intracranial GCTs (2-4). The peak incidence of intracranial GCT is during the second decade of life, with a median age at diagnosis of 10 to 14 years (5) (6). YST is a type of germ cell tumor. They primarily affect children and adolescents and mainly originate from gonads as other GCTs (7). Primary intracranial YSTs are very rare, accounting for 0.1% of all primary brain tumors (8). Multifocal primary intracranial YSTs have seldom been reported.
After reviewing the literature, we find several cases of YSTs in patients with Down syndrome have been reported (9,10). It was reported that 14 cases were germ cell tumors among the 23 case reports of brain tumors in patients with Down syndrome (9). They believed that the overexpression of the Dscr1 or Dyrk1a gene on chromosome 21 played a vital role in this (9-11). At the same time, intracranial GCTs are more common in Asian countries than in North America and Europe (2-4). Even in the United States, individuals with Asian/Pacific Islander ancestry have a two- to a threefold higher risk of intracranial GCT than whites, suggesting that genetic factors may be more important than environmental factors in the etiology of GCT (12).
Although Magnetic Resonance Imaging is the imaging of choice, there are few specific radiological features for YST (13). But magnetic resonance diffusion weighted images and magnetic resonance spectroscopy was reported to be helpful in differentiation from other neoplasms (14). The final diagnosis of YSTs depends on the pathology examinations, Schiller-Duval body and is pathognomonic of YSTs. However, Schiller-Duval bodies are present in 50–70% of YSTs (11,15). The treatment of YST is similar to other GCTs, complete surgical resection is the key to treatment, and a combination of surgical resection, chemotherapy, and radiotherapy is typically used (7,16). But the prognosis is still abysmal. The 3-year survival rate was reported as 27.3% (7,15).
Primary intracranial yolk sac tumors arise almost exclusively from midline locations such as pineal, suprasellar, etc. We find three nodules located at the pineal, suprasellar and left temporal lobe in the present case. According to the magnetic resonance imaging (MRI) and Intraoperative findings, we found that the tumor located at the left temporal lobe was much larger than the tumors situated in the pineal and suprasellar region, and intra-tumoral hemorrhage was observed for the tumor at the left temporal lobe, but this cannot be confirmed for the other two. We searched Pubmed with the MeSH Terms of “yolk sac tumors” and “CNS disease”, we found 83 reports. Then we searched with multiple or multifocal for all fields between these reports, with just 15 reports left. After screening the abstract, we found 2 cases that reported multiple intracranial yolk sac tumors (17,18). We have collected these patients' clinical features, including the present case in Table 1. This is the first report of multifocal primary intracranial yolk sac tumors with one nodule located at the left temporal lobe to the best of our knowledge.
Table 1
| Author | Sex | Age (years) | AFP | Location | Treatment | Prognosis |
|---|---|---|---|---|---|---|
| Mukasa, 2017 | Female | 24 | Elevated | Spinal canal (T12-L5) | Surgery + chemoradiotherapy | No recurrence 5 years after the surgery |
| Tang, 2012 | Female | 15 | Elevated | Pineal region and frontal horn of the right lateral ventricle | Surgery + chemoradiotherapy | No recurrence 14 days after the surgery |
| Present case | Male | 29 | Elevated | Suprasellar region, pineal region and left temporal lobe | Surgery + chemoradiotherapy | Died 11 months after the surgery |
Conclusions
We reported a case of multifocal primary intracranial yolk sac tumor in an adult patient. Such lesion is very rare, and the prognosis is poor. Timely diagnosis and treatment are essential for a better prognosis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-21-2561/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-21-2561/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the legal guardian for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhao S, Shao G, Guo W, et al. Intracranial pure yolk sac tumor in the anterior third ventricle of an adult: A case report. Exp Ther Med 2014;8:1471-2. [Crossref] [PubMed]
- Wong TT, Ho DM, Chang KP, et al. Primary pediatric brain tumors: statistics of Taipei VGH, Taiwan (1975-2004). Cancer 2005;104:2156-67. [Crossref] [PubMed]
- Cho KT, Wang KC, Kim SK, et al. Pediatric brain tumors: statistics of SNUH, Korea (1959-2000). Childs Nerv Syst 2002;18:30-7. [Crossref] [PubMed]
- Wang CH, Hsu TR, Yang TY, et al. Primary yolk sac tumor of bilateral basal ganglia. J Chin Med Assoc 2010;73:444-8. [Crossref] [PubMed]
- Gittleman H, Cioffi G, Vecchione-Koval T, et al. Descriptive epidemiology of germ cell tumors of the central nervous system diagnosed in the United States from 2006 to 2015. J Neurooncol 2019;143:251-60. [Crossref] [PubMed]
- Takami H, Fukuoka K, Fukushima S, et al. Integrated clinical, histopathological, and molecular data analysis of 190 central nervous system germ cell tumors from the iGCT Consortium. Neuro Oncol 2019;21:1565-77. [Crossref] [PubMed]
- Xu ZN, Yue XY, Cao XC, et al. Multidisciplinary treatment of primary intracranial yolk sac tumor: A case report and literature review. Medicine (Baltimore) 2021;100:e25778. [Crossref] [PubMed]
- Uda H, Uda T, Nakajo K, et al. Adult-Onset Mixed Germ Cell Tumor Composed Mainly of Yolk Sac Tumor Around the Pineal Gland: A Case Report and Review of the Literature. World Neurosurg 2019;132:87-92. [Crossref] [PubMed]
- Sugimoto K, Ideguchi M, Sadahiro H, et al. Yolk sac tumor of the bilateral basal ganglia in a patient with Down syndrome. Brain Tumor Pathol 2013;30:247-52. [Crossref] [PubMed]
- Maeda Y, Yoshikawa K, Kajiwara K, et al. Intracranial yolk sac tumor in a patient with Down syndrome. J Neurosurg Pediatr 2011;7:604-8. [Crossref] [PubMed]
- Endo S, Kobayashi H, Terasaka S, et al. Primary intracranial yolk sac tumor in the posterior fossa: case report of a child with Down syndrome. Clin Neurol Neurosurg 2013;115:811-3. [Crossref] [PubMed]
- Poynter JN, Fonstad R, Tolar J, et al. Incidence of intracranial germ cell tumors by race in the United States, 1992-2010. J Neurooncol 2014;120:381-8. [Crossref] [PubMed]
- Kan P, Gottfried ON, Blumenthal DT, et al. Primary spinal yolk sac tumor with brain metastasis: case report and review of the literature. J Neurooncol 2006;78:249-53. [Crossref] [PubMed]
- Macvanski M, Ristić-Balos D, Vasić B, et al. Intracranial yolk sac tumor in an adult patient: MRI, diffusion-weighted imaging and 1H MR spectroscopy features. Vojnosanit Pregl 2012;69:277-80. [Crossref] [PubMed]
- Matsutani M, Sano K, Takakura K, et al. Primary intracranial germ cell tumors: a clinical analysis of 153 histologically verified cases. J Neurosurg 1997;86:446-55. [Crossref] [PubMed]
- Fetcko K, Dey M. Primary Central Nervous System Germ Cell Tumors: A Review and Update. Med Res Arch 2018; [PubMed]
- Mukasa A, Yanagisawa S, Saito K, et al. Successful treatment of mixed yolk sac tumor and mature teratoma in the spinal cord: case report. J Neurosurg Spine 2017;26:319-24. [Crossref] [PubMed]
- Tang Z, Shi X, Singh Khatri Chhetri KI, et al. Intracranial endodermal sinus tumors associated with growth hormone replacement therapy in a girl. J Neurosurg Pediatr 2012;9:49-53. [Crossref] [PubMed]


