
Primary teratoma of the adrenal gland: a case report
Introduction
Teratomas are unusual tumors derived from more than one germ layer and often they arise from all three germ layers (1). Teratomas are rare neoplasms with an incidence rate of 0.9 per 100,000 people (2). Teratomas that occur in infancy and early childhood are usually extragonadal, while in adults they commonly occur in the gonads (3,4). Among retroperitoneal teratomas, primary adrenal teratomas are extremely rare in adults. Because of their low incidence, our understanding of adrenal teratomas is still limited. Here, we report a case involving a mature teratoma in the right adrenal gland of an adult female. We present the following case in accordance with the CARE reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-21-2913/rc).
Case presentation
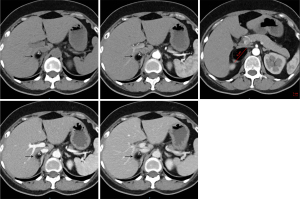
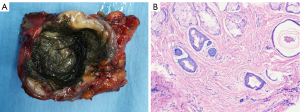
In this case, a mass was detected by computed tomography (CT) in the right adrenal gland of a 59-year-old female for 6 months without apparent discomfort. The patient did not have previous medical history. On examination, the patient’s blood pressure and adrenal function were found to be within the normal range. The patient did not exhibit adrenal dysfunction and had no family history of adrenal dysfunction. An abdominal enhanced CT scan revealed a heterogeneous mass measuring 6 cm by 5 cm in the right adrenal gland with a small cystic area, fat, and calcification (Figure 1). The patient’s initial diagnosis was adrenal myelolipoma. According to the Campbell-Walsh Urology (5), a relationship does exist between the size of an adrenal lesion and its malignant potential with larger masses more likely to exhibit adverse clinical and pathologic features. Masses less than 4 cm are considered to possess low malignant potential (2% are adrenal carcinomas). Masses that exceed 6 cm should be considered higher malignant potential (25% are adrenal carcinomas). In the intermediate size between 4 and 6 cm, the rate of malignancy is estimated to be 6%. Therefore, it is recommended that the tumor size greater than or equal to 6 cm is one of the indications for adrenalectomy. The size of this case is 6 cm, and the tumor has calcification on CT, which meets the surgical standard. The patient underwent laparoscopic right adrenalectomy and the tumor was found to have adhered to the liver and inferior vena cava. The mass had a cystic cavity of about 4.5 cm in diameter and was mainly composed of adipose tissue and hair (Figure 2A). It was pathologically diagnosed as mature teratoma of the adrenal gland (Figure 2B) and the patient recovered well without any complications.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Teratomas are neoplasms made of tissues from more than one germ layer. Although in adults they predominantly occur in the gonads, about 15% of teratomas occur in extragonadal sites (6). Extragonadal teratomas often occur in midline structures, such as the anterior mediastinum, retroperitoneum, sacrococcygeal region, pineal gland, and the suprasellar region (1). Primary extragonadal teratomas in retroperitoneal locations are very rare and account for only 4% of primary teratomas (2,3,7). It should be noted that unlike other adrenal tumors, so far, no patient has presented with bilateral adrenal teratomas. Highlighting the rarity of adrenal gland teratomas, only 39 cases have been reported in the past 30 years (8). Here, we report a case of a primary mature teratoma in the right adrenal gland of a 59-year-old female.
Zhong et al. reported that although adult adrenal teratomas occur over a wide age range, their incidence is highest in the third decade of life and they seem to be more common in women than in men (8). Asians have an increased risk of germ cell tumors, which may be associated with birthplace, genetic susceptibility and environmental exposure (9,10).
Most of the patients had solitary nonfunctioning adrenal masses. Clinically, the manifestation of adrenal teratomas is similar to that of other adrenal tumors without endocrine function. Sometimes adrenal teratomas are accompanied by nonobvious symptoms like abdominal distension, upper abdominal pain, or intestinal obstruction caused by compression (11). Imaging examination plays an important role in teratoma diagnosis and CT/magnetic resonance imaging (MRI) scanning can effectively distinguish adipose tissue from calcified masses. However, CT scans detect teratomas at an accuracy of only 64.3% and due to various image features, teratomas are easily confused with benign tumors like myelolipoma, adenoma, hamartoma, or even with malignant tumors (12). Because of the heterogeneity of fat content and density, differential diagnosis among adrenal myelolipoma, angiomyolipoma, liposarcoma, pheochromocytoma or malignant tumors is usually considered. Other differential diagnoses of retroperitoneal teratomas include ovarian tumors, renal cysts, adrenal tumors, Wilm’s tumor, sarcomas, retroperitoneal fibromas, cystic neuroblastoma, congenital mesoblastic nephroma, hemangiomas, xanthogranuloma, enlarged lymph nodes, and perirenal masses (12). CT scan makes it easy to mix up with some benign, even malignant tumors sometimes. Pathology is the gold standard. We think that it is inappropriate to classify this lesion as benign until proven by surgery and pathology.
Obtaining the main features of teratoma, such as cystic or solid cystic tumor containing calcification and fat and combining them with clinical features, imaging features, and endocrine examination is necessary for effective teratoma diagnosis and treatment. Most mature retroperitoneal teratomas are benign. For a retroperitoneal tumor, the possibility of germ cell tumor and tumor markers should be considered before surgery (13). The incidence of malignancy in retroperitoneal tumors in adults is 25.8%, which is significantly higher than in children (6.8%) (1,14). However, only few of the reported cases are malignant teratomas (15).
Surgical resection is the preferred strategy for the diagnosis and treatment of mature teratoma (1,16). Although open surgery was once the standard choice for resecting adrenal tumors, laparoscopic surgery has developed into the gold standard for the resection of benign adrenal masses. Open and laparoscopic surgical techniques do not differ significantly with regard to complications and cancer prognosis. Compared with open surgery, laparoscopic surgery can significantly reduce the incidence rate of complication, minimize pain, shorten hospital stay, and reduce overall recovery time.
In this case report, we successfully performed laparoscopic adrenalectomy. The prognosis for retroperitoneal teratoma usually good after complete resection, but close follow-up is recommended because of the risk of malignant transformation.
Acknowledgments
We thank F. Kobia, PhD, for editing the English text of a draft of this manuscript.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-21-2913/rc
Peer Review File: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-21-2913/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-21-2913/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gatcombe HG, Assikis V, Kooby D, et al. Primary retroperitoneal teratomas: a review of the literature. J Surg Oncol 2004;86:107-13. [Crossref] [PubMed]
- Taori K, Rathod J, Deshmukh A, et al. Primary extragonadal retroperitoneal teratoma in an adult. Br J Radiol 2006;79:e120-2. [Crossref] [PubMed]
- Polo JL, Villarejo PJ, Molina M, et al. Giant mature cystic teratoma of the adrenal region. AJR Am J Roentgenol 2004;183:837-8. [Crossref] [PubMed]
- Grosfeld JL, Billmire DF. Teratomas in infancy and childhood. Curr Probl Cancer 1985;9:1-53. [Crossref] [PubMed]
- McDougal WS, Wein AJ, Kavoussi LR, et al. editors. Campbell-Walsh Urology. 11 ed. Philadelphia: Elsevier Health Sciences 2015;Chapter III:Section 13.
- Li S, Li H, Ji Z, et al. Primary adrenal teratoma: Clinical characteristics and retroperitoneal laparoscopic resection in five adults. Oncol Lett 2015;10:2865-70. [Crossref] [PubMed]
- Bedri S, Erfanian K, Schwaitzberg S, et al. Mature cystic teratoma involving adrenal gland. Endocr Pathol 2002;13:59-64. [Crossref] [PubMed]
- Zhong W, Ma R, Cheng S, et al. Clinical Characteristics and Surgical Management of Adult Adrenal Teratoma: A 15-year Experience and Systematic Review of the Literature. Urology 2020;135:71-5. [Crossref] [PubMed]
- Chan JK, Gardner AB, Chan JE, et al. The influence of age and other prognostic factors associated with survival of ovarian immature teratoma - A study of 1307 patients. Gynecol Oncol 2016;142:446-51. [Crossref] [PubMed]
- Kakkar A, Biswas A, Kalyani N, et al. Intracranial germ cell tumors: a multi-institutional experience from three tertiary care centers in India. Childs Nerv Syst 2016;32:2173-80. [Crossref] [PubMed]
- Ciftci I, Cihan T, Koksal Y, et al. Giant mature adrenal cystic teratoma in an infant. Acta Inform Med 2013;21:140-1. [Crossref] [PubMed]
- Kuo EJ, Sisk AE, Yang Z, et al. Adrenal Teratoma: a Case Series and Review of the Literature. Endocr Pathol 2017;28:152-8. [Crossref] [PubMed]
- Rais-Bahrami S, Varkarakis IM, Lujan G, et al. Primary retroperitoneal teratoma presenting as an adrenal tumor in an adult. Urology 2007;69:185.e1-2. [Crossref] [PubMed]
- Okulu E, Ener K, Aldemir M, et al. Primary mature cystıc teratoma mimickıng an adrenal mass in an adult male patient. Korean J Urol 2014;55:148-51. [Crossref] [PubMed]
- Niu M, Liu A, Zhao Y, et al. Malignant transformation of a mature teratoma of the adrenal gland: A rare case report and literature review. Medicine (Baltimore) 2017;96:e8333. Erratum in: Medicine (Baltimore) 2017;96:e9104. [Crossref] [PubMed]
- Chiloiro S, Giampietro A, Bianchi A, et al. Clinical management of teratoma, a rare hypothalamic-pituitary neoplasia. Endocrine 2016;53:636-42. [Crossref] [PubMed]


