
Bibliometric analysis of an important diagnostic technique for the treatment of breast cancer
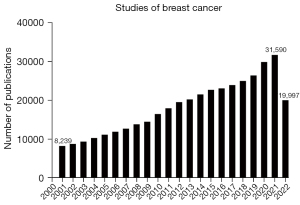
In 2020–2021, there were almost 40 million new cancer cases diagnosed, and 11.7% of those occurrences were neoplasms with the breast tissue as their primary tissue of development (1). In an oncological-gender specificity, this is the most prevalent site where women are affected by cancer and the leading causes of mortality (2). As a result, there is an increasing interest in breast cancer as a research target due to its high incidence and social effects. Consequently, it is seen that researchers are becoming more interested in finding ways to improve treatment approaches, as seen by the large quantity of scientific publications throughout time (Figure 1). And because published and ongoing research has a considerable impact on the clinical outcomes of breast cancer patients, it is crucial to comprehend the messages that come from this pool of accumulated literature (3).
Due to this demand, bibliometric studies serve as a crucial statistical instrument that contributes to the discovery of new themes and concepts for next studies through the mapping of data found in the literature (4,5). Additionally, makes it possible to evaluate the progress made thus far both qualitatively and quantitatively, enabling a better understanding and description of the dynamics of scientific findings in each research field (6). The analysis of published studies is crucial for pointing out therapeutic alternatives and encouraging the creation of guidelines, improving the prognosis for people with breast cancer.
Modifications in perivascular tissues are a significant factor among the early signs of this disease that can help to confirm a diagnosis more reliably. For instance, from axillary assessment, tissue that is directly associated with the illness stage may be collected and analyzed through biopsy (7). The status of the axillary lymph nodes is one of the strongest prognostic factors in early-stage of breast cancer, and the sentinel lymph node biopsy (SLNB) has become the standard of care in the assessment of metastatic spread, which is the major cause of cancer-related death (8). However, this method was questioned for its features like remarkably low invasiveness and great accuracy (9).
In this regard, we are pleased to highlight the remarkable findings published by Huo et al. [2022] (10), entitled “Thematic trends and knowledge structure map of sentinel lymph node biopsy for breast cancer: a bibliometric analysis from 2010 to 2019”. They examined a total of 4,152 articles published in 624 journals, discovered that in the previous ten years, researchers were very interested mainly in SLNB and sought to determine its benefits and drawbacks. In addition to learning more about how axillary lymph nodes are evaluated during neoadjuvant chemotherapy (NC). These significant findings are in line with various issues that arise throughout the diagnostic procedure, such as allergic reactions, potential teratogenic effects that should be avoided during pregnancy, or patients who are sensitive to this label. Additionally, studies have shown that SLNB performed after induction therapy has a higher false negative rate (11), even though this does not fall under the technique's contraindications, which include patients with inflammatory breast disease and those who have clinically positive axillary nodes.
Huo et al. [2022] (10) also demonstrated the wide range of benefits of SLNB, which justifies its current use in clinical practice. Notably, SLNB causes less damage to the nerves and lymphatic tissues. According to the information they reported, axillary lymph node dissection, which is much more invasive, causes lymphoedema with arm swelling and movement restrictions that significantly lower quality of life, but less than 5% after SLNB (12,13). In addition to being functionally tested by studies that injected probes and observed that the breast drain into the same sentinel node and injection into the dermis or breast parenchyma was immaterial, this technique was also shown to be feasible in other types of cancer, such as parotid tumors, penile cancer, and melanoma (14).
With the help of a bibliometric analysis, Huo et al. [2022] (10) have demonstrated that the SLNB may be regarded as a reliable, safe method that gives patients with early-stage breast cancer an accurate representation of their nodal metastases. Lastly, more studies are still needed to improve the comprehensive of treatment approaches and the development of techniques, thus, directly impacting in the quality of life of oncological patients, in which bibliometric studies can be one of these approaches among the current scenario of a massive number of daily publications.
Acknowledgments
Funding: Researchers are funded by
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Translational Cancer Research. The article did not undergo external peer review.
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2120/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Silva JDDE, de Oliveira RR, da Silva MT, et al. Breast Cancer Mortality in Young Women in Brazil. Front Oncol 2021;10:569933. [Crossref] [PubMed]
- Teles RHG, Yano RS, Villarinho NJ, et al. Advances in Breast Cancer Management and Extracellular Vesicle Research, a Bibliometric Analysis. Curr Oncol 2021;28:4504-20. [Crossref] [PubMed]
- Manoel Alves J, Handerson Gomes Teles R, do Valle Gomes Gatto C, et al. Mapping Research in the Obesity, Adipose Tissue, and MicroRNA Field: A Bibliometric Analysis. Cells 2019;8:1581. [Crossref] [PubMed]
- Teles RHG, Moralles HF, Cominetti MR. Global trends in nanomedicine research on triple negative breast cancer: a bibliometric analysis. Int J Nanomedicine 2018;13:2321-36. [Crossref] [PubMed]
- Donthu N, Kumar S, Mukherjee D, et al. How to conduct a bibliometric analysis: An overview and guidelines. J Bus Res 2021;133:285-96. [Crossref]
- Zahoor S, Haji A, Battoo A, et al. Sentinel Lymph Node Biopsy in Breast Cancer: A Clinical Review and Update. J Breast Cancer 2017;20:217-27. [Crossref] [PubMed]
- Qian CN, Mei Y, Zhang J. Cancer metastasis: issues and challenges. Chin J Cancer 2017;36:38. [Crossref] [PubMed]
- Filippakis GM, Zografos G. Contraindications of sentinel lymph node biopsy: are there any really? World J Surg Oncol 2007;5:10. [Crossref] [PubMed]
- Huo Y, Fan T, Chen S, et al. Thematic trends and knowledge structure map of sentinel lymph node biopsy for breast cancer: a bibliometric analysis from 2010 to 2019. Transl Cancer Res 2022; [Crossref] [PubMed]
- Kuehn T, Bauerfeind I, Fehm T, et al. Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol 2013;14:609-18. [Crossref] [PubMed]
- Arisio R, Borella F, Porpiglia M, et al. Axillary Dissection vs. no Axillary Dissection in Breast Cancer Patients With Positive Sentinel Lymph Node: A Single Institution Experience. In Vivo 2019;33:1941-7. [Crossref] [PubMed]
- Hennigs A, Köpke M, Feißt M, et al. Which patients with sentinel node-positive breast cancer after breast conservation still receive completion axillary lymph node dissection in routine clinical practice? Breast Cancer Res Treat 2019;173:429-38. [Crossref] [PubMed]
- D'Angelo-Donovan DD, Dickson-Witmer D, Petrelli NJ. Sentinel lymph node biopsy in breast cancer: a history and current clinical recommendations. Surg Oncol 2012;21:196-200. [Crossref] [PubMed]


