
Comparison of bronchial methylene blue staining and modified inflation-deflation method in identifying the intersegmental plane during lung segmentectomy
Introduction
With the widespread application of computed tomography (CT) screening, an increasing number of cases of early-stage lung cancer characterized by ground-glass nodules are being detected (1). Currently, anatomic lobectomy is the standard procedure used to treat non-small-cell lung cancer (2). Recently, a number of clinical studies have been published, including JCOG0802/WJOG4607L and CALGB/ALLIANCE 140503, which have shown that anatomic segmentectomy can achieve a comparable oncological effect and preserve lung function to a greater degree than lobectomy in patients with early-stage lung cancer (3-6). As such, anatomic pulmonary segmentectomy has become a popular surgical option in the field of thoracic surgery.
Due to the lack of anatomical marks between the lung segments, intersegmental plane (ISP) identification is still one of the main difficulties of anatomic segmentectomy. Researchers have developed a variety of methods to identify the ISP, such as the inflation-deflation method, systemic injection of indocyanine green, injection of endobronchial dye, three-dimensional simulation using multidetector CT, and virtual-assisted lung mapping (7-9). The modified inflation-deflation method relies on the reabsorption of oxygen by pulmonary arteries to reveal the ISP, it is a commonly used method because it does not require special materials and instruments (10). Moreover, the bronchial methylene blue staining method is performed by injecting methylene blue solution into the segmental bronchus to reveal the ISP. It was developed by our team in 2015 and has since become a commonly used method at our medical center. The rapid and simple identification of the ISP makes it potential to be widely used in lung segmentectomy (11).
Although the advantages of both methods are well documented, few studies have compared these methods with each other. In fact, publications describing the bronchial methylene blue staining method are scarce. In the current study, we retrospectively compared the data of patients who underwent the endobronchial methylene blue staining method with the data of patients who underwent the modified inflation-deflation method. We also present our experience of the methylene blue staining method in identifying the ISP during thoracoscopic anatomic pulmonary segmentectomy to provide a reference for clinical application. We present the following article in accordance with the STROBE reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-1428/rc).
Methods
Study design
This study was conducted in accordance with the Declaration of Helsinki (2013 revision). The study was approved by Ethics Committee of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (No. 0565) and individual consent for this retrospective analysis was waived.
We reviewed the data of 112 patients who underwent thoracoscopic anatomic pulmonary segmentectomy performed by the same medical group between June 2020 and September 2021 in the Department of Thoracic Surgery, Union Hospital (Wuhan, China). Of them, 62 patients underwent the endobronchial methylene blue staining method (methylene blue group), while 50 patients underwent the modified inflation-deflation method (modified inflation-deflation group). Methylene blue injection (Jiangsu Jumpcan Pharmaceutical, Jiangsu, China; drug approval number: H32024827, China Food and Drug Administration) is commonly used in the clinical setting.
The inclusion criteria were as follows: (I) peripheral nodules ≤2 cm in diameter, together with at least one of the following factors: pathological confirmation of adenocarcinoma in situ (AIS), nodules with ≥50% ground-glass appearance on CT, or a tumor doubling time of ≥400 days according to radiologic surveillance; (II) no evidence of lymph nodes or distant metastases; (III) marginal cardiopulmonary reserve or multiple comorbidities limiting the option of lobectomy (12). Exclusion criteria included the presence of other metastatic disease, comorbidities in cardiovascular, lung, kidney and other important organ that cannot tolerate surgery. Complex combined subsegmental resections were also not included in this study.
Preoperative assessment and operative procedure
All procedures were performed by the same surgical team. All procedural steps were the same between the two groups, except for the ISP identification method. Before surgery, all patients underwent enhanced thin-section (≤1 mm) chest CT examinations, followed by three-dimensional reconstruction to identify the location of the nodule, pulmonary bronchi, and vessels of the target segment. Then, the surgical simulation of segmentectomy was performed according to the three-dimensionally reconstructed images to ensure that the tumor resection margin was ≥2 cm or greater than the maximum diameter of the tumor.
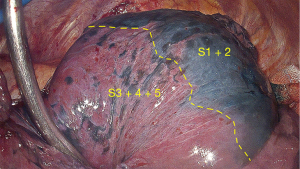
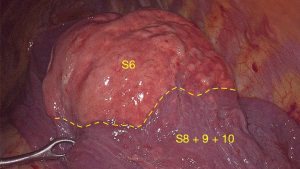
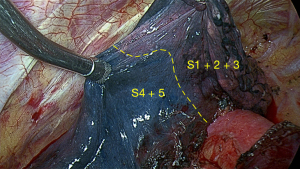
Surgery was performed under general anesthesia using double-lumen tracheal intubation with the patient in the lateral decubitus position. The two-port technique to perform segmentectomy via video-assisted thoracoscopic surgery was used. The operation port (3 cm) was at the fourth intercostal space of the mid-axillary line, and the observation port (1 cm) was at the seventh or eighth intercostal space of the posterior axillary line. Using the preoperative three-dimensionally reconstructed images, we accurately identified and dissected the target segmental arteries, veins, and bronchi. The ISP was visualized using the bronchial methylene blue staining method or the modified inflation-deflation method. In the methylene blue group, after the target segmental vessels and bronchi were dissected, the methylene blue diluent was injected into the target segmental bronchi using an intravenous needle connected to a 20-mL syringe. The needle was held using hemostatic forceps to control the puncture angle and depth. The injection rate was approximately 0.2 mL per second. After the injection of methylene blue dilute solution, the ISP could be visualized (Figure 1). Based on our previous experience, 2 mL methylene blue diluted with 20 mL physiological saline can be used to clearly visualize the ISP without affecting the search for pure ground-glass nodules in surgical specimens. The volume of methylene blue injected into each pulmonary segment was approximately 8–10 mL. In addition, the injection needle was positioned at a puncture angle of approximately 10–15° to the bronchus, and the puncture depth was approximately 0.5 cm. In the modified inflation-deflation group, after the target segmental vessels and bronchi were dissected, the collapsed lung was fully inflated with pure oxygen by the anesthesiologist, followed by single lung ventilation until the ISP appeared (Figure 2). Finally, the ISP was divided using electrocautery (monopolar cautery) and stapling.
The resected segment was kept in a specimen bag, and the N1 and N2 lymph nodes were sampled to evaluate the possibility of nodal metastases. If there was evidence of lymph node involvement, lobectomy and systemic lymph node dissection were performed. After surgery, an 18-Fr thoracic drainage tube was placed in the chest cavity, and the thoracic cavity drainage was recorded every morning after surgery. The chest drainage tube was removed when the output volume was <200 mL within 24 hours and the lung had expanded on chest X-ray. The patients were discharged without symptoms of discomfort 12 hours after chest drainage tube removal.
Timing of ISP (TISP) identification
The TISP identification was recorded during surgery. In the methylene blue group, the TISP identification began when the surgeon started to inject the diluted methylene blue solution into the bronchus of the dissociated target segment after dissection of the segmental vessels and bronchi. The TISP identification end point was reached when the ISP was clearly visible. In the modified inflation-deflation group, the TISP identification began when the anesthesiologist started to re-expand the lung after dissection of the target segmental vessels and bronchi. The TISP identification end point was reached when the preserved segment was fully deflated and a stable boundary had formed between the target segment and the adjacent preserved lung segment.
Statistical analysis
All data were analyzed using SPSS software (version 24; IBM Corp., Chicago, IL, USA). Continuous data are reported as mean ± standard deviation. Variables were compared between the two groups using the independent-samples t-test. The correlations between variables were analyzed using Pearson’s correlation coefficient. A P value of <0.05 was considered statistically significant.
Results
A total of 112 patients who underwent segmentectomy were included in this study. Of these, 62 underwent the bronchial methylene blue staining method, while 50 underwent the modified inflation-deflation method. As shown in Table 1, there were no significant differences between the two groups in age, sex, smoking history, preoperative pulmonary function [forced expiratory volume in 1 second (FEV1)], or tumor size. The types of segmentectomy in the two groups are shown in Table 2. For basal segment resection, the bronchial methylene blue staining method was used slightly more frequently than the modified inflation-deflation method, because with the latter method, the already small operating space will become even smaller when the lungs are re-inflated.
Table 1
| Characteristics | Methylene group (n=62) | Modified inflation-deflation group (n=50) | P value |
|---|---|---|---|
| Age (years) | 53.06±13.04 | 53.72±11.68 | 0.782 |
| Gender, n | 0.481 | ||
| Male | 22 | 21 | |
| Female | 40 | 29 | |
| Smoking history, n | 0.315 | ||
| Yes | 6 | 8 | |
| No | 56 | 42 | |
| Preoperative FEV1 (L) | 2.69±0.64 | 2.70±0.60 | 0.938 |
| Tumor size (mm) | 13.16±0.43 | 12.12±0.36 | 0.171 |
Continuous data are reported as mean ± standard deviation. FEV1, forced expiratory volume in 1 second.
Table 2
| Resected segment | Methylene blue group (n=62) | Modified inflation-deflation group (n=50) |
|---|---|---|
| Right | ||
| S1 | 10 | 6 |
| S1 + 2 | 0 | 2 |
| S2 | 9 | 8 |
| S3 | 6 | 5 |
| S6 | 2 | 2 |
| S7 + 8 | 7 | 2 |
| S8 | 0 | 1 |
| S9 + 10 | 5 | 2 |
| S10 | 1 | 0 |
| Left | ||
| S1 + 2 | 10 | 12 |
| S1 + 2 + 3 | 1 | 0 |
| S3 | 1 | 2 |
| S4 + 5 | 2 | 1 |
| S6 | 2 | 2 |
| S8 | 3 | 2 |
| S9 + 10 | 3 | 3 |
Table 3 shows the characteristics of ISP visualization. The time taken to visualize the ISP in the methylene blue group was significantly shorter than the time taken to visualize the ISP in the modified inflation-deflation group (82.94±28.08 vs. 868.20±145.89 seconds; P<0.001). In the methylene blue group, the ISP was clearly visualized in 59 patients (95.2%). The reasons for poor visualization were as follows: (I) leakage of methylene solution during puncture of the segmental bronchi in two patients and (II) coverage of the lung parenchyma surface by severe anthracosis in one patient (Figure 3). In the modified inflation-deflation group, the ISP was clearly visualized in 47 patients (94.0%). The reasons for poor visualization were as follows: (I) serious emphysema in two patients and (II) severe pleural adhesion in one patient.
Table 3
| Variables | Methylene blue group (n=62) | Modified inflation-deflation group (n=50) | P value |
|---|---|---|---|
| Time taken to visualize the inflation-deflation line (seconds) | 82.94±28.08 | 868.20±145.89 | <0.001 |
| ISP visualization, n (%) | 0.786 | ||
| Good | 59 (95.2) | 47 (94.0) | |
| Poor | 3 (4.8) | 3 (6.0) | |
| Reasons for poor visualization, n | |||
| Methylene leakage | 2 | 0 | |
| Severe anthracosis | 1 | 0 | |
| Severe pleural adhesion | 0 | 1 | |
| Emphysema | 0 | 2 |
Continuous data are reported as mean ± standard deviation. ISP, intersegmental plane.
The perioperative outcomes of the two groups are shown in Table 4. The surgical duration in the methylene blue group was significantly shorter than the surgical duration in the modified inflation-deflation group (131.69±32.05 vs. 146.08±28.11 minutes; P=0.014). There were no significant differences in the volume of blood loss, duration of postoperative drainage, duration of postoperative hospitalization, and postoperative morbidity between the two groups. In the methylene blue group, postoperative complications occurred in four patients (6.5%), including prolonged air leak (>7 days) in two patients, pleural effusion after discharge in one patient, and atrial fibrillation in one patient. In the modified inflation-deflation group, postoperative complications occurred in three patients (6.0%), including prolonged air leak (>7 days) in one patient, pleural effusion after discharge in one patient, and pulmonary infection in one patient.
Table 4
| Variables | Methylene blue group (n=62) | Modified inflation-deflation group (n=50) | P value |
|---|---|---|---|
| Surgical duration (minutes) | 131.69±32.05 | 146.08±28.11 | 0.014 |
| Blood loss (mL) | 86.40±42.50 | 89.06±80.01 | 0.822 |
| Postoperative drainage duration (days) | 3.15±0.62 | 3.30±0.93 | 0.296 |
| Postoperative hospitalization duration (days) | 5.48±2.27 | 5.32±2.24 | 0.703 |
| Complication, n (%) | 4 (6.5) | 3 (6.0) | 0.922 |
| Prolonged air leakage, n | 2 | 1 | |
| Pleural effusion after discharge, n | 1 | 1 | |
| Atrial fibrillation, n | 1 | 0 | |
| Pulmonary infection, n | 0 | 1 | |
| Mortality, n | 0 | 0 | |
| Pathological diagnosis, n (%) | |||
| Benign | 2 (3.2) | 2 (4.0) | |
| AIS | 8 (12.9) | 4 (8.0) | |
| MIA | 22 (35.5) | 18 (36.0) | |
| IAC | 30 (48.4) | 25 (50.0) | |
| Pulmonary metastasis | 0 | 1 (2.0) |
Continuous data are reported as mean ± standard deviation. AIS, adenocarcinoma in situ; MIA, minimally invasive adenocarcinoma; IAC, invasive adenocarcinoma.
Pathology confirmed complete target lesion resection with negative surgical margins. The pathological diagnoses in the methylene blue group were benign lesions [two patients (3.2%)], AIS [eight patients (12.9%)], minimally invasive adenocarcinoma (MIA) [22 patients (35.5%)], and invasive adenocarcinoma (IAC) [30 patients (48.4%)]. The pathological diagnoses in the modified inflation-deflation group were benign lesions [two patients (4.0%)], AIS [four patients (8.0%)], MIA [18 patients (36.0%)], IAC [25 patients (50.0%)], and pulmonary metastasis [one patient (2.0%)].
Discussion
For pulmonary nodules of ≤2 cm in diameter, segmentectomy is preferred over wedge resection because it allows for sufficient surgical margins and achieves superior oncological outcomes (13,14). The key to effective anatomic segmental resection is the identification and management of the ISP. In terms of perioperative outcomes, inaccurate ISP identification may lead to dysfunction of the remaining lung tissue, disproportionate ventilation and blood flow, and long-term postoperative lung leakage. Moreover, unplanned secondary surgery may be required. In terms of oncological results, inaccurate ISP identification may lead to inadequate surgical margins, which are the main cause of loco-regional recurrence and impaired long-term survival (7,15).
Currently, the methods used to identify the ISP can be divided into two categories according to the different identification paths: the transbronchial approach and the transvascular approach. The transbronchial approach is a method that utilizes the supply area of the segmental bronchus; for example, Okada et al. used a fiberoptic bronchoscope to insert continuous high-frequency ventilation into the target segment of the bronchus, allowing inflation of the target lung segment while the adjacent segment was collapsed to visualize the ISP (9). Although this method is rapid, it requires the anesthesiologist to operate the bronchoscope, and due to the presence of intersegmental Kohn’s pores, gas can diffuse through Kohn’s pores into adjacent segments, leading to failure of ISP identification. Kamiyoshihara et al. used a butterfly needle to inject oxygen into the target segment after lung deflation to reveal the ISP (16). This method avoids the need for bronchoscopic manipulation by the anesthesiologist, but it has been reported to it carries a risk of air embolism due to inadvertent air injection into the vessel (17). The bronchial methylene blue injection has been used in our center for 7 years without similar complications. Moreover, Oizumi et al. ligated the target segmental bronchi with a slip-knot after lung expansion, thereby creating an ISP between the inflated target segment and the adjacent collapsed segment (18). Sekine et al. and Oh et al. used intrabronchial injection of indocyanine green to identify the ISP, this is a transbronchial method that can quickly identify the ISP (19,20). The bronchial methylene blue staining method described in this study is another transbronchial method. Since this method was developed by our team in 2015, it has been used for ISP identification in our center (11). Compared with other transbronchial methods of ISP identification, the bronchial methylene blue staining method does not require special equipment, is simple and convenient, and can identify the ISP quickly and accurately.
The transvascular approach is a method used to identify the ISP, as determined by segmental vascular perfusion. The modified inflation-deflation method may involve multiple mechanisms, with the predominant mechanism being the vascular reabsorption of gases (10,21,22). For example, with the modified inflation-deflation method, the lung is re-expanded after segmental vascular dissection. The gas in the target segment cannot be reabsorbed by the arteries; thus, the target segment remains in an expanded state. Conversely, the gas in the adjacent segments is absorbed by the arteries; thus, the adjacent segments are in a collapsed state. These differences in the state of inflation allow the ISP to be visualized (10,21). The modified inflation-deflation method is commonly used in the clinic because it does not require any special equipment, is simple and easy to perform, and can accurately and stably delineate the ISP (23). Intravenous indocyanine green injection is an example of a transvascular approach, which can quickly and easily identify the ISP (24). Nevertheless, the ISP only appears on the surface of the lung for a few tens of seconds and then quickly vanishes, and the requirement for expensive fluorescent thoracoscopy hampers the broader use of this technique.
Both transbronchial and transvascular approaches can be used to identify the ISP, but few studies have compared them. In this study, we chose the bronchial methylene blue staining method as a transbronchial approach and compared it with the modified inflation-deflation method as a transvascular approach. There were no significant differences between the two approaches in terms of the surgical procedure of the target segment vessels and bronchi. However, with the modified inflation-deflation method, we had to wait for a period of time before the ISP could be visualized. This wait time is about 15 minutes, which is also similar to previous reports (12,25). This was not the case with the bronchial methylene blue method, where the ISP could be visualized during methylene blue injection, thus reducing the anesthesia time and surgical duration. Compared with the modified inflation-deflation method, the methylene blue staining method does not require anesthesiologists to perform lung expansion and can be performed with the commonly used methylene blue injection. The modified inflation-deflation method failed to visualize the ISP in patients with special conditions, such as emphysema and severe pleural adhesion, while the methylene blue staining method failed to visualize the ISP if the injection needle was not properly punctured into the segmental bronchus. In the modified inflation-deflation group, the inflated target segment was not conducive to lesion removal via the small incision. In addition, inflation of the target segment made it difficult to palpate the lesion when it was not on the surface of the target segment. This situation did not exist in the bronchial methylene blue staining group.
Both transbronchial and transvascular methods have their advantages and disadvantages. The transbronchial method is technically easier and faster, but some scholars consider the ISPs to be inaccurate with this method because of the presence of Kohn pores and direct airway anastomosis (21). The transvascular method can accurately identify the ISP, but some scholars believe that the transbronchial method is more ideal because segmentectomy is performed based on the bronchial anatomy and the lymphatic channels from the tumor are along the bronchi (26). In the present study, both methods could accurately identify the ISP. In our experience, when attempting to identify the ISP in the upper lobes, such as the apical or posterior segments, the angle of intrabronchial methylene blue injection is difficult to control. In such cases, it is appropriate to choose the modified inflation-deflation method. Conversely, when attempting to identify the ISP in the lower lobes, such as the basal segment, the operation space decreases in size after expansion using the modified inflation-deflation method, making it difficult to remove the specimen via the small incision. In such cases, it is better to use the methylene blue staining method.
This study has some limitations that should be noted. First, it was a retrospective study with a small sample size. Second, endobronchial methylene blue injection requires a learning curve for the surgeon, but it is easy for the surgeon to master. To avoid methylene blue solution dispersion, the operator can slow down the injection speed so that if there is a dispersion of the melanin solution, it can be seen early and the puncture angle can be changed.
Conclusions
In conclusion, both the methylene blue staining method and the modified inflation-deflation method can clearly reveal the ISP. Compared with the modified inflation-deflation method, the bronchial methylene blue staining method has a faster recognition speed and a shorter surgical duration, it does not affect the size of the thoracoscopic operation space, and there is no need for the anesthesiologist to perform lung inflation. Thus, the bronchial methylene blue staining method is safe and simple, can be widely applied during thoracoscopic anatomic segmentectomy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-1428/rc
Data Sharing Statement: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-1428/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-1428/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (2013 revision). The study was approved by Ethics Committee of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (No. 0565) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang W, Qian F, Teng J, et al. Community-based lung cancer screening with low-dose CT in China: Results of the baseline screening. Lung Cancer 2018;117:20-6. [Crossref] [PubMed]
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 22-3. [Crossref] [PubMed]
- Saji H, Okada M, Tsuboi M, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 2022;399:1607-17. [Crossref] [PubMed]
- Altorki NK, Wang X, Wigle D, et al. Perioperative mortality and morbidity after sublobar versus lobar resection for early-stage non-small-cell lung cancer: post-hoc analysis of an international, randomised, phase 3 trial (CALGB/Alliance 140503). Lancet Respir Med 2018;6:915-24. [Crossref] [PubMed]
- Kodama K, Higashiyama M, Okami J, et al. Oncologic Outcomes of Segmentectomy Versus Lobectomy for Clinical T1a N0 M0 Non-Small Cell Lung Cancer. Ann Thorac Surg 2016;101:504-11. [Crossref] [PubMed]
- Chen L, Gu Z, Lin B, et al. Pulmonary function changes after thoracoscopic lobectomy versus intentional thoracoscopic segmentectomy for early-stage non-small cell lung cancer. Transl Lung Cancer Res 2021;10:4141-51. [Crossref] [PubMed]
- Andolfi M, Potenza R, Seguin-Givelet A, et al. Identification of the intersegmental plane during thoracoscopic segmentectomy: state of the art. Interact Cardiovasc Thorac Surg 2020;30:329-36. [Crossref] [PubMed]
- Misaki N, Chang SS, Gotoh M, et al. A novel method for determining adjacent lung segments with infrared thoracoscopy. J Thorac Cardiovasc Surg 2009;138:613-8. [Crossref] [PubMed]
- Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg 2007;133:753-8. [Crossref] [PubMed]
- Wang J, Xu X, Wen W, et al. Modified method for distinguishing the intersegmental border for lung segmentectomy. Thorac Cancer 2018;9:330-3. [Crossref] [PubMed]
- Zhang Z, Liao Y, Ai B, et al. Methylene blue staining: a new technique for identifying intersegmental planes in anatomic segmentectomy. Ann Thorac Surg 2015;99:238-42. [Crossref] [PubMed]
- Yang W, Liu Z, Yang C, et al. Combination of nitrous oxide and the modified inflation-deflation method for identifying the intersegmental plane in segmentectomy: A randomized controlled trial. Thorac Cancer 2021;12:1398-406. [Crossref] [PubMed]
- Dai C, Shen J, Ren Y, et al. Choice of Surgical Procedure for Patients With Non-Small-Cell Lung Cancer ≤ 1 cm or > 1 to 2 cm Among Lobectomy, Segmentectomy, and Wedge Resection: A Population-Based Study. J Clin Oncol 2016;34:3175-82. [Crossref] [PubMed]
- Paoletti L, Pastis NJ, Denlinger CE, et al. A decade of advances in treatment of early-stage lung cancer. Clin Chest Med 2011;32:827-38. [Crossref] [PubMed]
- Nakazawa S, Shimizu K, Mogi A, et al. VATS segmentectomy: past, present, and future. Gen Thorac Cardiovasc Surg 2018;66:81-90. [Crossref] [PubMed]
- Kamiyoshihara M, Kakegawa S, Ibe T, et al. Butterfly-needle video-assisted thoracoscopic segmentectomy: a retrospective review and technique in detail. Innovations (Phila) 2009;4:326-30. [Crossref] [PubMed]
- Otsuka T, Nakamura Y, Harada A, et al. Extremely rare but potential complication of diffuse brain edema due to air embolism during lung segmentectomy with selected segmental inflation technique by syringe needle during video-assisted thoracoscopic surgery. J Thorac Cardiovasc Surg 2011;142:e151-2. [Crossref] [PubMed]
- Oizumi H, Kato H, Endoh M, et al. Slip knot bronchial ligation method for thoracoscopic lung segmentectomy. Ann Thorac Surg 2014;97:1456-8. [Crossref] [PubMed]
- Sekine Y, Ko E, Oishi H, et al. A simple and effective technique for identification of intersegmental planes by infrared thoracoscopy after transbronchial injection of indocyanine green. J Thorac Cardiovasc Surg 2012;143:1330-5. [Crossref] [PubMed]
- Oh S, Suzuki K, Miyasaka Y, et al. New technique for lung segmentectomy using indocyanine green injection. Ann Thorac Surg 2013;95:2188-90. [Crossref] [PubMed]
- Fu HH, Feng Z, Li M, et al. The arterial-ligation-alone method for identifying the intersegmental plane during thoracoscopic anatomic segmentectomy. J Thorac Dis 2020;12:2343-51. [Crossref] [PubMed]
- Sun Y, Zhang Q, Wang Z, et al. Is the near-infrared fluorescence imaging with intravenous indocyanine green method for identifying the intersegmental plane concordant with the modified inflation-deflation method in lung segmentectomy? Thorac Cancer 2019;10:2013-21. [Crossref] [PubMed]
- Chen X, Zhang Z, Xu N, et al. Review of Approaches to Developing Intersegmental Plane during Segmentectomy. Thorac Cardiovasc Surg 2022;70:341-5. [Crossref] [PubMed]
- Jin Y, Wang M, Xue L, et al. Clinical Application of Near-Infrared Thoracoscopy With Indocyanine Green in Video-Assisted Thoracoscopic Anatomical Segmentectomy. Surg Innov 2019;26:473-7. [Crossref] [PubMed]
- Fan W, Yang H, Ma J, et al. Indocyanine green fluorescence-navigated thoracoscopy versus traditional inflation-deflation approach in precise uniportal segmentectomy: a short-term outcome comparative study. J Thorac Dis 2022;14:741-8. [Crossref] [PubMed]
- Funai K, Kawase A, Shimizu K, et al. Fluorescence navigation with indocyanine green for identification of intersegmental planes using a photodynamic eye camera. J Thorac Dis 2020;12:4817-24. [Crossref] [PubMed]


