A retrospective analysis of clinical pathological characteristics and prognosis of 82 patients of primary intestinal lymphoma
Introduction
The gastrointestinal tract is the most common extranodal site of involvement in Non-Hodgkin lymphoma (NHL), representing 30–45% of all extranodal lymphoma (ENL) cases. The gastric lymphoma is the predominant location for ENL (55–70%) whereas intestinal lymphoma is less frequently observed in small intestines (20–35%) and large intestines (5–10%) (1).
Nowadays, due to the lack of characteristic clinical symptom, specific serum and imaging test results, it is still difficult for physicians to make early diagnosis of primary intestinal lymphoma (PIL) which might cause the delay of treatment and affect the prognosis of patients.
In order to better master and treat this neoplasm, we make a retrospective study involving 82 patients with PIL who were diagnosed in Ruijin Hospital from 2003 to 2015. This study occurred in a single institution in China, which analyzed the clinical features, histological subtype, method of treatment and prognosis of PIL.
Methods
Eighty-two adult patients with PIL were enrolled in our retrospective study from December 2003 to June 2015. During this period, 99 patients were diagnosed with PIL in our hospital, but we excluded juvenile patients and those out of follow-up visit. Our study finally collected complete clinical, pathological and follow-up data of 82 patients with PIL. All cases were confirmed according to the pathological samples from endoscopic biopsy or surgical resection. Patients were included in current analysis if they met the following Dawson’s criteria: (I) absence of palpable superficial lymphadenopathy; (II) normal leukocyte and differential counts; (III) non-enlargement of mediastinal lymph nodes on chest X-ray; (IV) no grossly demonstrable involvement beyond the affected segment of the intestine and its regional mesenteric lymph nodes at the time of diagnosis; and (V) absence of tumor involvement of the liver and spleen (2). All patients were performed with immunohistochemical detection. And if tumor shows one or more B cell, markers were identified as IBC; and if the tumor shows one or more T cell, markers were identified as ITCL. Furthermore, the accurate immunophenotypic subtype was identified by the World Health Organization (WHO) classification of tumors of the hematopoietic and lymphoid tissues in 2008 (3). And the staging of those patients was confirmed by Lugano staging system for gastrointestinal lymphoma (4). The Lugano staging system was concluded by physical examination, radiological imaging, positron emission tomography/computed tomography (PET/CT) and the pathological result by endoscopic biopsy and the surgical sample. In our study, we divided patients into two groups (stage I/II and stage III/IV) for a comparative analysis.
The follow-up data of the 99 PIL patients were obtained through medical records of hospitalization, telephonic communication or in person at the clinic. A total of 82 out of the 99 cases completed the follow-up and the follow-up rate was 82.8%. The follow-up data began with the first day of diagnosis and ended up with the last connection with patients or relatives of patients. And the deadline of follow-up was September 30, 2015.
Statistical analysis
The comparative analysis between intestinal B-cell lymphoma (IBCL) and ITCL were tested by χ2 test. We used overall survival (OS) to evaluate the prognosis of patients with PIL. OS was defined as the interval from the date of diagnosis to the date of death from any cause or the last follow-up date. All deaths from other causes were recorded as censored. OS was estimated using the Kaplan-Meier product-limit method and was compared by means of the log-rank test. Cox’s proportional hazard regression analysis was used to evaluate prognostic factors. The following clinical and pathological factors were chosen for survival analysis: gender, age of onset (<60 or ≥60 years), B symptom (presence or absence), complication (obstruction and perforation included), phenotype (IBCL or ITCL), location (small intestines, ileocecal region, large intestines, colon and rectum, or multiple sites), Lugano stage (Stage I/II or Stage III/IV) and treatment (surgery alone, chemotherapy alone, surgery and chemotherapy combined or neither surgery nor chemotherapy). P<0.05 was considered to indicate a statistical difference. The statistical data were obtained using an SPSS software package (SPSS 21.0, IBM, Chicago, Illinois, USA).
Results
Patient characteristics
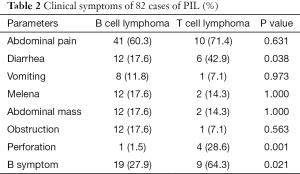
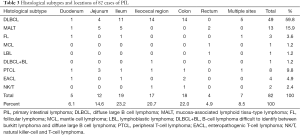
From December 2003 to June 2015, a total of 82 patients with PIL were enrolled in our study. The characteristics of patients are summarized in Table 1 and Table 2. The study cohort consisted of 53 men and 29 women (the ratio was 1.8:1) with a median age of 59.5 years (range, 18–81 years). Regarding histological subtype classification, IBCL accounted for 82.9% and ITCL accounted for 17.1%. PIL mostly occurred in small intestines (45.1, duodenum, jejunum and ileum included), followed by colon and rectum (26.8%), ileocecal region (20.7%) and multiple sites (7.3%). Most patients had localized disease with earlier Lugano stage I/II (92.7%) while a small part of patients (7.3%) had further involvement with Lugano stage III/IV. Between the group of IBCL and ITCL, there is no statistic difference for the proportion of gender and Lugano stage.
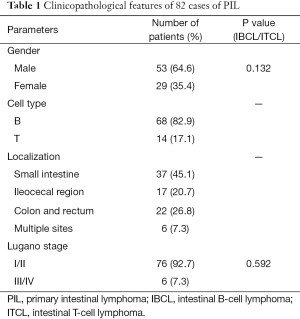
Full table
Full table
The clinical symptoms of PIL were unspecific which contain abdominal pain, diarrhea, vomiting, melena, abdominal mass, obstruction, perforation, B symptom etc. B symptom is defined as: fever 38 °C above, for three consecutive days or more without infection reason; weight loss more than 10% in 6 months and night sweat. A conclusion can be drawn from Table 2 that in the group of ITCL, the proportion of diarrhea, perforation and B symptom is higher than the group of IBCL, which has a statistic difference (P<0.05).
Histological subtype and locations
The various histological subtype along the anatomic sites are shown in Table 3. According to the WHO classification, in the group of IBCL, 49 cases were classified as DLBCL which was the predominant histological subtype, followed by 13 as MALT, 3 as follicular lymphoma (FL). Mantle cell lymphoma (MCL), lymphoblastic lymphoma (LBL) and B-cell lymphoma difficult to identify between burkitt lymphoma and diffuse large B cell lymphoma (DLBCL + BL) all have only one case. The other group of ITCL includes 8 of peripheral T-cell lymphoma (PTCL), 4 of enteropathogenic T-cell lymphoma (EACL), 2 of natural killer-cell and T-cell lymphoma (NK/T). From the study we also concluded that PIL mostly occurred in ileum (23.2%), followed by colon (22.0%), ileocecal region (20.7%), jejunum (14.6%), multiple sites (8.5%), duodenum (6.1%) and rectum (4.9%).
Full table
Prognostic factors
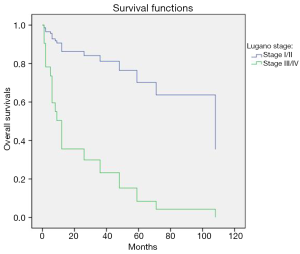
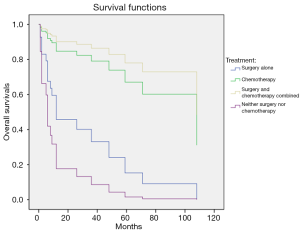
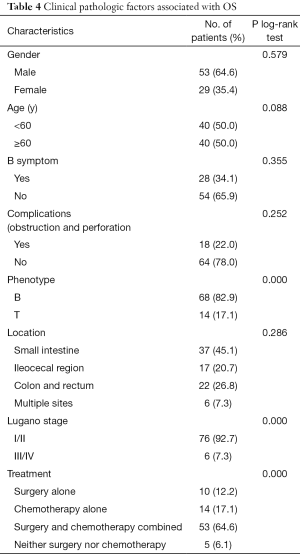
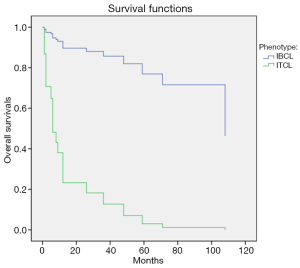
Univariate analysis using Kaplan-Meier product-limit method was compared by means of the log-rank test. The results indicated that Lugano stage, immunophenotype and the method of treatment were significant predictive factors for better patient survival (P=0.003, 0.000 and 0.000, respectively, Table 4).
Full table
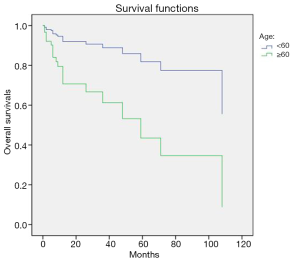
Furthermore, we select the factors whose P value is under 0.1 according to the univariate analysis to make a multivariate analysis. The factors included age of onset, Lugano stage, phenotype and treatment and all had statistical differences in multivariate analysis. A conclusion could be drawn that younger age of onset (<60 years), Lugano stage I/II, IBCL and treatment based on surgery and chemotherapy were significant predictive factors (P=0.005, 0.005, 0.000 and 0.000, respectively, Figures 1,2,3,4).
Discussion
In recent decades, the incidence of PIL augments gradually. The etiology of PIL is not clear, on the one hand it perhaps results from the virus infection, genetic variation, other chronic intestinal infection, etc. On the other hand, the treatment of immunosuppressive drugs, infection of HIV, organ transplantation, autoimmune diseases, immunodeficiency diseases, and inflammatory bowel diseases may increase the incidence of PIL obviously (5).
This retrospective study analyzed the clinical features, histological subtype, treatment and prognosis of PIL in China. In our research, the median age of patients at diagnosis was 59.5 years (range, 18–81 years). The patients with PIL tend to be middle-to-old age population. The male to female ratio was 1.8:1. According to the histological subtype classification, IBCL accounted for 82.9% and ITCL accounted for 17.1%. The incidence of IBCL was much higher than T-cell lymphoma. And DLBCL was the predominant histological subtype followed by MALT and PTCL. Furthermore, in our study the proportion of DLBCL (n=49, 59.8%) was significantly higher than MALT (n=13, 15.9%) and PTCL (n=8, 9.8%). One study of PIL in Korea had a similar result with our study. In their research, the median age was 56 years (range, 15–92 years) and the male to female ratio was 1.8:1. The main subtype was DLBCL followed by MALT and PTCL (6).
In our study, most patients had earlier Lugano stage I/II (n=76, 92.7%) which revealed that PIL predominantly presents as a localized disease. This result was strongly supported by the previous studies (1,7-10).
In terms of location, in our study the small intestine was the most common site (n=37, 45.1%), followed by colon and rectum (n=22, 26.8%), ileocecal region (n=17, 20.7%) and multiple sites (n=6, 7.3%). Another study of anatomic sites with PIL in China turned out similarly as above (11). However, the result is in disagreement with other previous studies (10,12,13) which revealed that the colon was the most common site. And there are also another conclusion that the ileocecal region is the predominate site (6,7).
Regarding the clinical symptoms of PIL, including abdominal pain, diarrhea, vomiting, melena, abdominal mass, obstruction, perforation, B symptom etc., we can draw a conclusion that in the group of ITCL, the proportion of diarrhea, perforation and B symptom is higher than the group of B cell lineage lymphoma (P<0.05). The prevalence of perforation and diarrhea in ITCL may be due to the invasion of ITCL to the vascular wall, causing vascular occlusion and ischemic necrosis, and finally resulted in perforation and diarrhea (14).
In this study, we used univariate and multivariate analyses to analyze OS for patients with PIL with regard to numerous clinicopathologic factors. In univariate analysis, Lugano stage, immunophenotype and treatment significantly influenced OS in patients with PIL. Application of the multivariate Cox proportion hazard model revealed that besides factors above, the OS was also dependent on the age of onset. The younger age of onset (<60 years) had a better prognosis in the multivariate Cox proportion hazard model. The advanced international research also indicated the age was the independent factor of prognosis (10).
Considering about the survival benefit, IBCL had a better prognosis than ITCL which was the same to the previous studies (6,15-17). The better prognosis of IBCL may be due to the following reasons: in IBCL the indolent Lymphoma has a higher proportion such as MALT and FL etc. These tumors have a lower growth rate and take a longer time to form the neoplasm. Furthermore the majority of ITCL has a higher malignant degree and rapid progress of growth which might cause the poorer prognosis than IBCL.
According to the Lugano staging system, the advanced stage III/IV had been associated with a relatively poor prognosis compared to those with early stage I/II, which was the same to the previous studies (15,17).
However, OS in different anatomic sites of PIL in our study had no statistic difference. In another study (17), OS in the small intestine and ileocecal region were significantly longer compared with rectum and multiple sites. The various results perhaps result from the different precise definition of anatomic sites and racial difference: (I) in our study, we divided cases into four groups (small intestines, ileocecal region, colon and rectum, and multiple sites); (II) the different definition of ileocecal region: in our study, ileocecal region included the terminal ileum, cecum and vermiform appendix; (III) the sample size is not large enough.
Nowadays, there is still no accurate strategy of treatment for PIL. The optimal treatment for PIL is still a work challenging and controversial. We should make the treatment plan according to the immunophenotype and clinical stage. The previous reports on the treatment results for patients with PIL indicated a superior survival in patients treated with multiple treatment including surgery, chemotherapy, and radiotherapy in comparison with patients treated with a single modality (8,18). The intestine is less suitable for radiotherapy than the stomach, so in our hospital patients with PIL were rarely treated with radiotherapy. In our study, according to the method of treatment, we divided the patients with PIL into four groups (surgery alone, chemotherapy alone, surgery plus chemotherapy and neither surgery nor chemotherapy). The result turned out that the group of patients received treatment with surgery plus chemotherapy was significantly longer than patients without surgery or chemotherapy (Figure 4). The another research of Khosla suggested that the 5-year OS rate in group of patients with surgery plus chemotherapy was higher than patients with chemotherapy alone (79.5% vs. 13.9%) (19). These findings suggest that the better outcome in the surgery plus chemotherapy group might be related to the complete resection of the bowel segment. However, the effect of surgical treatment still remains controversial. Previous studies reported that primary surgical treatment had a favorable influence on the prognosis of PIL (17,20). Primary surgical resection has been proposed as a rational treatment choice, as it simultaneously establishes the diagnosis and reduces the tumor burden (17). But there is no demonstration of the theoretical basis regarding the reason why reducing tumor burden is important in improving survival in PIL. More studies will be needed in the future to understand the reason. And due to the difficulties in preoperative pathologic diagnosis and the risk of complications requiring surgery, the use of surgical resection for PIL was widely applied. PIL are heterogeneous diseases. In our opinion, the controversial treatment may be caused by the different constitution of these subtypes, ignoring racial and environment factors.
Conclusions
The optimal management of primary lymphoma of PIL is not established. The prognosis of PIL was influenced by the disease staging, the histological type and treatment, etc. (5,21,22). In our study, younger age, earlier-stage and IBCL cases may achieve better survival benefit from the treatment of surgery plus chemotherapy. In consequence, the pathologists and clinicians should synthesize the clinical pathological information to make the early diagnosis and the proper treatment of PIL which could prolong the survival time of patients.
Acknowledgments
Funding: This study was supported by Science and Technology Fund Project of Shanghai Jiaotong University School of Medicine (No.14XJ10014).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.07.10). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics committee of Ruijin Hospital (2016-022), Shanghai Jiao Tong University School of Medicine, and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- d'Amore F, Brincker H, Grønbaek K, et al. Non-Hodgkin's lymphoma of the gastrointestinal tract: a population-based analysis of incidence, geographic distribution, clinicopathologic presentation features, and prognosis. Danish Lymphoma Study Group. J Clin Oncol 1994;12:1673-84. [PubMed]
- Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg 1961;49:80-9. [Crossref] [PubMed]
- Vardiman JW. The World Health Organization (WHO) classification of tumors of the hematopoietic and lymphoid tissues: an overview with emphasis on the myeloid neoplasms. Chem Biol Interact 2010;184:16-20. [Crossref] [PubMed]
- Rohatiner A, d'Amore F, Coiffier B, et al. Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol 1994;5:397-400. [PubMed]
- Stanojevic GZ, Nestorovic MD, Brankovic BR, et al. Primary colorectal lymphoma: An overview. World J Gastrointest Oncol 2011;3:14-8. [Crossref] [PubMed]
- Kim SJ, Choi CW, Mun YC, et al. Multicenter retrospective analysis of 581 patients with primary intestinal non-hodgkin lymphoma from the Consortium for Improving Survival of Lymphoma (CISL). BMC Cancer 2011;11:321. [Crossref] [PubMed]
- Koch P, del Valle F, Berdel WE, et al. Primary gastrointestinal non-Hodgkin's lymphoma: I. Anatomic and histologic distribution, clinical features, and survival data of 371 patients registered in the German Multicenter Study GIT NHL 01/92. J Clin Oncol 2001;19:3861-73. [PubMed]
- Li B, Shi YK, He XH, et al. Primary non-Hodgkin lymphomas in the small and large intestine: clinicopathological characteristics and management of 40 patients. Int J Hematol 2008;87:375-81. [Crossref] [PubMed]
- Yin L, Chen CQ, Peng CH, et al. Primary small-bowel non-Hodgkin's lymphoma: a study of clinical features, pathology, management and prognosis. J Int Med Res 2007;35:406-15. [Crossref] [PubMed]
- Nakamura S, Matsumoto T, Iida M, et al. Primary gastrointestinal lymphoma in Japan: a clinicopathologic analysis of 455 patients with special reference to its time trends. Cancer 2003;97:2462-73. [Crossref] [PubMed]
- Ding W, Zhao S, Wang J, et al. Gastrointestinal Lymphoma in Southwest China: Subtype Distribution of 1,010 Cases Using the WHO (2008) Classification in a Single Institution. Acta Haematol 2016;135:21-8. [Crossref] [PubMed]
- Liang R, Todd D, Chan TK, et al. Prognostic factors for primary gastrointestinal lymphoma. Hematol Oncol 1995;13:153-63. [Crossref] [PubMed]
- Morton JE, Leyland MJ, Vaughan Hudson G, et al. Primary gastrointestinal non-Hodgkin's lymphoma: a review of 175 British National Lymphoma Investigation cases. Br J Cancer 1993;67:776-82. [Crossref] [PubMed]
- Zhu L, Wu G, Ghimire P, et al. CT features of peripheral T-cell lymphoma in the gastrointestinal tract in Chinese population and literature review. J Med Imaging Radiat Oncol 2012;56:143-50. [Crossref] [PubMed]
- Gou HF, Zang J, Jiang M, et al. Clinical prognostic analysis of 116 patients with primary intestinal non-Hodgkin lymphoma. Med Oncol 2012;29:227-34. [Crossref] [PubMed]
- Wang GB, Xu GL, Luo GY, et al. Primary intestinal non-Hodgkin's lymphoma: a clinicopathologic analysis of 81 patients. World J Gastroenterol 2011;17:4625-31. [Crossref] [PubMed]
- Lee J, Kim WS, Kim K, et al. Intestinal lymphoma: exploration of the prognostic factors and the optimal treatment. Leuk Lymphoma 2004;45:339-44. [Crossref] [PubMed]
- Ibrahim EM, Ezzat AA, El-Weshi AN, et al. Primary intestinal diffuse large B-cell non-Hodgkin's lymphoma: clinical features, management, and prognosis of 66 patients. Ann Oncol 2001;12:53-8. [Crossref] [PubMed]
- Khosla D, Kumar R, Kapoor R, et al. A retrospective analysis of clinicopathological characteristics, treatment, and outcome of 27 patients of primary intestinal lymphomas. J Gastrointest Cancer 2013;44:417-21. [Crossref] [PubMed]
- Lee J, Kim WS, Kim K, et al. Prospective clinical study of surgical resection followed by CHOP in localized intestinal diffuse large B cell lymphoma. Leuk Res 2007;31:359-64. [Crossref] [PubMed]
- Wang SL, Liao ZX, Liu XF, et al. Primary early-stage intestinal and colonic non-Hodgkin's lymphoma: clinical features, management, and outcome of 37 patients. World J Gastroenterol 2005;11:5905-9. [Crossref] [PubMed]
- Chuang SS, Ye H, Yang SF, et al. Perforation predicts poor prognosis in patients with primary intestinal diffuse large B-cell lymphoma. Histopathology 2008;53:432-40. [Crossref] [PubMed]