
Dietary vitamin D intake and risk of non-small cell lung cancer: a matched case-control study
Introduction
Lung cancer is the leading cause of malignant tumor-related deaths, and non-small cell lung cancer (NSCLC) reportedly comprises approximately 85% of all lung cancer cases (1). Lung cancer is believed to be caused by the interaction of both environment and hereditary factors. Environmental inventions targeting dietary and lifestyle may be the major means for preventing lung cancer. Vitamin D (Vit D) is a steroid-derived vitamin and its metabolites in cancer have become highly regarded recently (2-7). Vit D exerted important functions in tumor development by regulating cell proliferation, facilitating apoptosis, promoting cell differentiation, and inhibiting angiogenesis (8,9), as well as the optimal 25(OH)D concentration for preventing and surviving cancer appears to be above 75–100 nmol/L (10). Epidemiological studies indicated that serum Vit D level was inversely associated with lung cancer development and prognosis (11-13). However, reports are lacking on the association between dietary intake of Vit D and the risk of lung cancer in Chinese populations. Here we performed a 1:1 matched case control study to investigate the association between dietary Vit D and the risk of NSCLC in the Qingdao area.
Methods
A total of 200 NSCLC patients (153 men, 47 women) who were admitted to the Affiliated Hospital of Qingdao University, Qingdao Hiser hospital, and Pingdu City Hospital of Traditional Chinese Medicine were recruited between December 2014 and March 2015 according to the diagnostic criteria of the “Standard for Diagnosis and Treatment of Primary Lung Cancer by the Ministry of Health” issued in 2011. All of the patients were diagnosed with primary lung cancer by pathologic examination, and the diagnoses included squamous cell carcinoma in 102 patients (51%), adenocarcinoma in 93 (46.5%), adenosquamous carcinoma in 4 (2%), and carcinoid in 1 (1%). Tumor stages were classified according to the International Association for the Study of Lung Cancer (IASLC 2009), 7th edition and included: stage I in 39 patients (19.5%), stage II in 57 (28.5%), stage III in 93 (46.5%), and stage IV in 11 (5.5%). All of the patients were diagnosed within 1 month prior to completing the interview and questionnaire. The exclusion criteria included: (I) insufficient liver and kidney functions, diabetes, thyroid dysfunction, and other nutrient metabolism disorders; (II) taking Vit D supplements; and (III) receiving glucocorticoid treatment. A total of 200 age (±3 years) and sex-matched controls from three hospitals were also included. All participants provided written informed consent. The study was approved by the Institutional Ethics Committee of Medical College of Qingdao University.
Face-to-face interviews were conducted to collect general and dietary information. The food intake information during the past 1 year was collected using a food frequency questionnaire (FFQ) designed for residents in north China which has been proven reliability and validity (14). The FFQ includes 81 total items in seven frequency categories as follows: (I) almost never eat or drink; (II) less than once per week; (III) once a week; (IV) 2–3 times per week; (V) 4–6 times per week; (VI) once a day; (VII) twice or more per day. The amount of food was estimated using a collection of illustrative pictures of food or dishware to which the participants referred for guidance.
Statistical analysis
The questionnaire was uploaded and checked by two persons in EpiData 3.1, and analyses by SPSS version 17.0 software (SPSS Inc, Chicago, IL, USA). The t test or χ2 test was utilized to compare data of the patients and healthy controls. The case control set was divided into quartiles by Vit D daily intake. The association between Vit D intake (Q1–Q4) and NSCLC risk was analyzed by logistic regression. The value of Q1 was set as a reference, the odds ratios (OR), adjusted OR and 95% confidence intervals (CI) of the other groups were calculated. Multivariate conditional logistic regression analysis was used to adjust for age, gender, body mass index, education level, profession, family income, smoking, secondary smoking, drinking, outdoor activities, family tumor history.
Results
General information
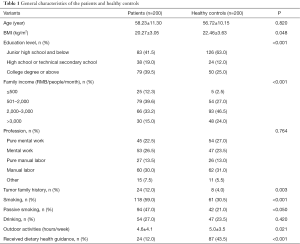
The average ages of the patients and healthy controls were 58.23±11.30 and 56.72±10.15 years, respectively; there were no significant differences in age, sex, or profession between the two groups (Table 1). Compared with the healthy controls, the patients had relatively lower body mass index (P=0.048), higher education level (P<0.001), less family income (P<0.001), spent less time engaging in outdoor activities (P=0.021), and were less likely to receive dietary guidance (P<0.001). Meanwhile, a family tumor history (P=0.003), smoking (P<0.001), and secondary smoking (P<0.05) were more commonly found in patients than in controls.
Full table
Inverse association between daily dietary Vit D and NSCLC
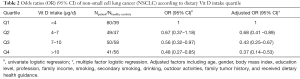
The daily intakes of Vit D were 5.4±1.2 and 7.5±1.6 µg for patients and healthy controls, respectively, and the daily mean intake of Vit D from dietary sources was lower in patients than in healthy controls (P<0.001). The incidence OR of NSCLC was gradually decreased along with the increase of daily dietary Vit D intake, indicating that dietary Vit D was a protective factor for NSCLC. The association between Vit D intake and NSCLC remained unchanged after the adjustment for confounding factors including age, gender, body mass index, education level, profession, family income, smoking, secondary smoking, drinking, outdoor activities, family tumor history, and received dietary health guidance (Table 2).
Full table
Stratification analysis
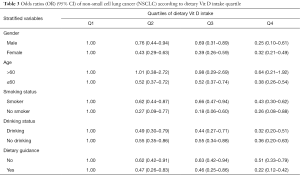
The stratification analysis indicated that Vit D intake was inverse associated with NSCLC in the ≤60 years old group, while no association in the >60 years old group. There was an consistently inverse association between dietary Vit D intake and NSCLC when stratified by other factors including smoking, drinking, and dietary guidance received (Table 3).
Full table
Discussion
Our findings indicated that the OR of NSCLC was decreased along with the increase in dietary Vit D intake, implying that Vit D deficiency might be a risk factor for NSCLC. The inverse association between Vit D and NSCLC remained unchanged when the confounding factors were adjusted, including age, gender, body mass index, education level, profession, family income, smoking, secondary smoking, drinking, outdoor activities, family tumor history, and received dietary health guidance. This finding was consistent with other studies. Cheng et al. found that serum Vit D level was negatively correlated with death rate in non-smoking lung cancer patients (15). Zhou reported that serum 25(OH)D level and Vit D intake were positively associated with total survival period of patients with early-stage NSCLC (16). A meta-analysis of prospective studies conducted by Chen suggested that 25(OH)D may be associated with reduced risk of lung cancer (12). It was also reported that Vit D acquired by solar ultraviolet-B (UVB) exposure could decrease one’s risk of lung cancer; for instance, Chen found that mortality rates for lung cancer were inversely correlated with ambient UVB (17); Grant reported that the UVB index, which formed by lip cancer less lung cancer standardized incidence radios, was significantly inversely correlated with lung cancer (18). Above studies presented indirect evidence that dietary Vit D could decrease the risk of lung cancer.
Major studies reported that Vit D exerted its anti-cancer effects by targeting cancer or normal cells with the potential to transform into cancer cells. The anti-tumor mechanism of Vit D might be associated with its abilities to suppress cellular proliferation, promote cellular apoptosis, and inhibit angiogenesis (8,19). Vit D also regulates immune function, inhibits the production of prostaglandin, protease, and pro-inflammatory cytokines, all of which are mediators that can promote tumor development and progression (19,20). Shin et al. recently showed that Vit D deficiency was closely associated with epidermal growth factor receptor (EGFR) mutation in patients with adenocarcinoma (21). All these findings indicate a novel direction for Vit D anti-cancer mechanism research.
UVB exposure is normally the major source of Vit D for humans; however, Vit D deficiency is reportedly as low as 40% in residents of Northeast China (22). Therefore, dietary Vit D is the major source for people living at high latitudes or during winter or spring. Qingdao and Dalian are located north of 36 and 39 degrees latitude, respectively, and the Vit D deficiency rates for people from the Dalian area were reportedly 40% (22). The consumption of sea fish as food more than four times a week by Japanese women was reported to effectively prevent Vit D deficiency (23). Therefore, from the perspective of cancer prevention, the increased ingestion of dietary Vit D-rich food such as fish, animal liver, dairy products, and mushrooms was recommended in addition to increased daylight exposure.
Conclusions
This study indicated that dietary Vit D intake insufficiency might be a risk factor for NSCLC. But, this study’s retrospective nature may not completely exclude the bias introduced by participant recall, and serum Vit D levels were not determined. Therefore, further cohort studies are needed to investigate whether insufficient dietary Vit D intake increases one’s risk of lung cancer.
Acknowledgments
Funding: This work was supported by grants from the development of medical science and technology project of Shandong Province (grant numbers: 2014WSA02034).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.07.19). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Ethics Committee of Medical College of Qingdao University of No. 20140421 and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maione P, Rossi A, Sacco PC, et al. Advances in chemotherapy in advanced non-small-cell lung cancer. Expert Opin Pharmacother 2010;11:2997-3007. [Crossref] [PubMed]
- Clark AS, Chen J, Kapoor S, et al. Pretreatment vitamin D level and response to neoadjuvant chemotherapy in women with breast cancer on the I-SPY trial (CALGB 150007/150015/ACRIN6657). Cancer Med 2014;3:693-701. [Crossref] [PubMed]
- Cai LL, Ye HM, Lv XN, et al. 25-(OH)VitD3, as a risk indicator in diagnosis of adenocarcinoma. Curr Drug Targets 2013;14:1367-76. [Crossref] [PubMed]
- Wei MY, Giovannucci EL. Vitamin D and multiple health outcomes in the Harvard cohorts. Mol Nutr Food Res 2010;54:1114-26. [PubMed]
- Obaidi J, Musallam E, Al-Ghzawi HM, et al. Vitamin D and its relationship with breast cancer: an evidence based practice paper. Glob J Health Sci 2014;7:261-6. [Crossref] [PubMed]
- Kalfeřt D, Ludvíková M, Pešta M, et al. Vitamin D in relation to head and neck cancer. Vnitr Lek 2014;60:51-8. [PubMed]
- Aguirre M, Manzano N, Salas Y, et al. Vitamin D deficiency in patients admitted to the general ward with breast, lung, and colorectal cancer in Buenos Aires, Argentina. Arch Osteoporos 2016;11:4. [Crossref] [PubMed]
- Ness RA, Miller DD, Li W. The role of vitamin D in cancer prevention. Chin J Nat Med 2015;13:481-97. [PubMed]
- Chirumbolo S. Vitamin D3 in cancer prevention and therapy: the nutritional issue. Horm Mol Biol Clin Investig 2015;23:71-8. [Crossref] [PubMed]
- Grant WB. Roles of Solar UVB and Vitamin D in Reducing Cancer Risk and Increasing Survival. Anticancer Res 2016;36:1357-70. [PubMed]
- Li R, Lou Y, Zhang W, et al. Vitamin D inhibition of lung adenocarcinoma cell proliferation in vitro. Tumour Biol 2014;35:10953-8. [Crossref] [PubMed]
- Chen GC, Zhang ZL, Wan Z, et al. Circulating 25-hydroxyvitamin D and risk of lung cancer: a dose-response meta-analysis. Cancer Causes Control 2015;26:1719-28. [Crossref] [PubMed]
- Cheng TY, Lacroix AZ, Beresford SA, et al. Vitamin D intake and lung cancer risk in the Women's Health Initiative. Am J Clin Nutr 2013;98:1002-11. [Crossref] [PubMed]
- Wang X, Sa R, Yan H. Validity and reproducibility of a food frequency questionnaire designed for residents in north China. Asia Pac J Clin Nutr 2008;17:629-34. [PubMed]
- Cheng TY, Neuhouser ML. Serum 25-hydroxyvitamin D, vitamin A, and lung cancer mortality in the US population: a potential nutrient-nutrient interaction. Cancer Causes Control 2012;23:1557-65. [Crossref] [PubMed]
- Zhou W, Heist RS, Liu G, et al. Circulating 25-hydroxyvitamin D levels predict survival in early-stage non-small-cell lung cancer patients. J Clin Oncol 2007;25:479-85. [Crossref] [PubMed]
- Chen W, Clements M, Rahman B, et al. Relationship between cancer mortality/incidence and ambient ultraviolet B irradiance in China. Cancer Causes Control 2010;21:1701-9. [Crossref] [PubMed]
- Grant WB. Role of solar UVB irradiance and smoking in cancer as inferred from cancer incidence rates by occupation in Nordic countries. Dermatoendocrinol 2014;4:203-11. [Crossref] [PubMed]
- Nakagawa K, Sasaki Y, Kato S, et al. 22-Oxa-1alpha,25-dihydroxyvitamin D3 inhibits metastasis and angiogenesis in lung cancer. Carcinogenesis 2005;26:1044-54. [Crossref] [PubMed]
- Trump DL, Muindi J, Fakih M, et al. Vitamin D compounds: clinical development as cancer therapy and prevention agents. Anticancer Res 2006;26:2551-6. [PubMed]
- Shin DY, Kim S, Park S, et al. Serum 25-hydroxyvitamin D levels correlate with EGFR mutational status in pulmonary adenocarcinoma. Endocr Relat Cancer 2014;21:715-21. [Crossref] [PubMed]
- Zhou B, Wang XH, Guo LY, et al. Vitamin D deficiency in winter related to bone loss of older people in northern China. J Clin Rehabil Tissue Eng Res 2011;15:4907-10.
- Whiting SJ, Calvo MS. Dietary recommendations to meet both endocrine and autocrine needs of Vitamin D. J Steroid Biochem Mol Biol 2005;97:7-12. [Crossref] [PubMed]


