
An unusual clearance of primary pediatric fibrosarcoma of the right parietal lobe after surgery and radiation therapy
Introduction
To our knowledge, only a few reports on PPF, especially patients with good prognosis, have been published in the English literature. With poor overall outcome of this rare disease, increased awareness which may lead to an earlier stage of diagnosis. In hope of neurological damage are reversible and more effective palliation may be achieved. Recognition and diagnosis are both clinically important for therapeutic prognosis and preoperative counseling. Postoperative radiotherapy may be beneficial for young patients.
Case presentation
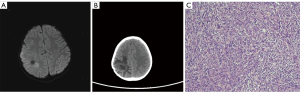
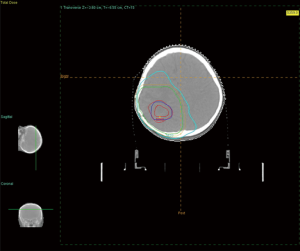
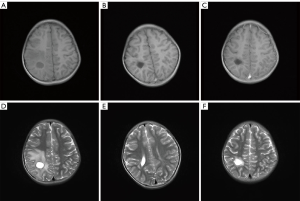
A 5-year-old Han Chinese girl was admitted on October 24, 2012 because of tics of the limbs and foaming at the mouth without other complications a week prior to admission. The symptom disappeared in 5 min. She did not complain of tinnitus, headache, nausea, vomiting, or loss of consciousness. No anomalous manifestations of the nervous system was found during physical examination. The patient’s family history and medical record was not significant. A space-occupying lesion was seen in the right parietal lobe by magnetic resonance imaging (MRI), which was considered as astrocytoma or parasite infection. Occupying lesion resection was suggested to clear the symptoms and determine the pathology. A 2 cm × 2 cm × 2 cm subdural tumor tissue was observed at 2 cm deep during the surgical procedure. The tissue was leathery in texture and with rich blood supply. The tumor was totally removed by intracranial microsurgery. Pathological results showed the possibility of spindle cell tumor (right parietal lobe, 2.2 cm × 1.2 cm × 0.6 cm), Vim (++), S100 (+), GFAP (−), Olig-2 (−), NF (−), Neu-N (+/−), CD34 (++), CD56 (−), Ki-67 (approximately 5%) (+), EMA (−), SMA (−), and Actin (−). The case was diagnosed as primary fibrosarcoma according to pathology and clinical symptoms. The girl received a PET/CT scan within one month post surgery and showed no sign of tumor residue. Additionally, the cranial MRI showed an oval cystic lesion in the left parietal lobe. The lesion measured approximately 1.45 cm × 1.76 cm and surrounded by patchy edema stoves. Diffusion weighted imaging showed slightly high-signal lesions in the left parietal lobe, and no abnormal signal intensity was noted in the rest of the brain (Figure 1). Postoperative radiotherapy (50.4 Gy/28 f) was then recommended. The first radiotherapy accumulated to 34.2 Gy/19 f, and then locally increased reduced-field radiotherapy was added to reach total volume (Figure 2). The girl did not complain of special side effects, except for local alopecia, during the therapy. The girl was reexamined by MRI twice a year, and the results showed no recurrence and metastases (Figure 3). The girl has a disease-free survival to date since first diagnosis and treatment.
Discussion
Primary cerebral fibrosarcoma of is very rare, especially in children, the average incidence of which is 1.5% of all central nervous system neoplasms (1). Postoperative recurrence and metastases had been documented in previous studies as a tendency. More than 20 cases of primary fibrosarcomas of the brain that were not secondary to radiotherapy have been reported in the past two decades. Local recurrence but not metastasis was detected by Massier 7 months after gross total resection (2). Li et al. described local tumor recurrence 3 months postoperatively and metastases 22 months after gross resection of a patient with primary pediatric fibrosarcoma (PPF) (3).
Poor prognosis has been reported for patients with primary intracranial fibrosarcoma. However, in our case, no radiographic recurrence and metastases were found in MRI, and the patient has a completely clinical clearance until 3 years after therapy until reported. We treated our patient using a combined multimodality approach, which included surgery and radiotherapy. The treatment options for patients with systemic malignancy increased and have resulted in prolonged survival, which lead to diagnoses of various metastatic diseases that have previously been infrequent. It is considered that intracranial fibrosarcomas is intrinsically aggressive lesions and should be treated forcefully with multimodality measures. Hence, the decision for surgical interventions and adjuvant treatment are still ambiguous.
Our patient presents some unique characteristics compared with previous reports. There are few cases of de novo fibrosarcoma with documented early natural history in literature. This case has a concrete documentation that a parenchymal brain fibrosarcoma developed de novo and progressed from a 5-mm hyperintense nodule on T2-weighted MRI to a 5-cm mass within a 12-month period. Several published cases of fibrosarcoma described a short interval to tumor recurrence following surgical resection and radiation therapy (4-6). The intrinsically aggressive tumor biology was possibly influenced or aggravated by the effects of irradiation on tumor differentiation (7-9). Recently, Giridhar et al. provided Egyptian experience of intracranial fibrosarcoma treated with adjuvant radiation and temozolomide. The addition of chemotherapy added new insights of practice (10).
In our case, the diagnosis of primary intracranial fibrosarcoma was based on a systemic tumor survey as well as on morphological and immunohistochemical studies. The diagnosis was confirmed by the morphological features of the spindle cells in a fascicular pattern and the prominent vimentin positivity. The high cellularity and high mitotic rate demonstrated that the tumor was a high-grade fibrosarcoma. Although MRI has become the most widely used diagnostic modality of choice for brain occupation, PPF may not always be distinguished from similar radiological features of other diseases in this way.
Acknowledgments
Funding: This work was supported by the Natural Science Foundation of China (No. 81272504, No. 81472809), Innovation Team [No. LJ201123 (EH11)], A Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD) (JX10231801), grants from Key Academic Discipline of Jiangsu Province “Medical Aspects of Specific Environments”, Six Major Talent Peak Project of Jiangsu Province (2013-WSN-040), and “333” Project of Jiangsu Province [BRA2012210 (RS12)].
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.07.09). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Muzumdar D, Michaud J, Ventureyra EC. Primary giant congential infantile fibrosarcoma of the scalp: case report and review of literature. Childs Nerv Syst 2006;22:300-4. [Crossref] [PubMed]
- Massier A, Scheithauer BW, Taylor HC, et al. Sclerosing epithelioid fibrosarcoma of the pituitary. Endocr Pathol 2007;18:233-8. [Crossref] [PubMed]
- Li ZJ, Sun P, Guo Y, et al. Primary pituitary fibrosarcoma presenting with multiple metastases: a case report and literature review. Neurol India 2010;58:316-8. [Crossref] [PubMed]
- Erguvan-Onal R, Onal C, Gürlek A, et al. Metastatic fibrosarcoma of the brain: transformation from conventional to epithelioid form--case report. Neurol Med Chir (Tokyo) 2004;44:497-501. [Crossref] [PubMed]
- Bisogno G, Roganovic J, Carli M, et al. Primary intracranial fibrosarcoma. Childs Nerv Syst 2002;18:648-51. [Crossref] [PubMed]
- Torres G, Petit F, Vilchez V, et al. Primary cerebral fibrosarcoma in a child. Clin Neuropathol 2007;26:284-7. [Crossref] [PubMed]
- Fraser RW, Limentani SA, Dollar JD, et al. Recurrent primary fibrosarcoma of the brain treated with the GliaSite brachytherapy system: case report. Surg Neurol 2003;60:579-83; discussion 583-4. [Crossref] [PubMed]
- Abe T, Kamida T, Goda M, et al. Intracranial infiltration by recurrent scalp dermatofibrosarcoma protuberans. J Clin Neurosci 2009;16:1358-60. [Crossref] [PubMed]
- Tun K, Ozen O, Kaptanoglu E, et al. Primary intracranial low-grade fibromyxoid sarcoma (Evans tumor). J Clin Neurosci 2008;15:1298-301. [Crossref] [PubMed]
- Giridhar P, Mallick S, Haresh KP, et al. Intracranial fibrosarcoma treated with adjuvant radiation and temozolomide: Report of a case and review of all published cases. J Egypt Natl Canc Inst 2016;28:111-6. [Crossref] [PubMed]


