
Promise of vandetanib, a FDA-approved RET kinase inhibitor, for the treatment of RET fusion-positive lung adenocarcinoma
The advent of precision lung cancer medicine, involving the treatment of tumors with EGFR and ALK oncogene aberrations with drugs that inhibit EGFR and ALK kinase activities, respectively, is potentially transformative for lung cancer patients. In 2012, oncogenic fusion of the RET gene, a driver of thyroid carcinogenesis, was re-discovered in a small subset of lung cancer by several groups (1-3). In-flame fusion of the RET tyrosine kinase gene with kinesin family member 5B (KIF5B) or coiled-coil domain containing 6 (CCDC6) genes, resulting in constitutive activation of the RET oncogene product, was identified as a novel oncogenic aberration in 1–2% of non-small cell carcinomas (NSCLCs), mainly in those with a histology of lung adenocarcinoma (LADC). These and a subsequent study demonstrated that the RET fusion gene has tumor-driving activity in vitro and in vivo (1-4). Up to now, a few other genes, including nuclear-receptor coactivator 4 (NCOA), tripartite-motif containing 33 (TRIM33), cutlike homeobox 1 (CUX1), KIAA1468 and KIAA1217 [also known as SKT, the human homolog of murine Skt (Sickle tail)], have been identified as other fusion partners of RET in NSCLC patients (5,6). In all these RET fusions, the coiled-coil domains of the partner proteins induce dimerization of the RET fusion protein, resulting in constitutive activation of RET kinase. The KIF5B-RET fusion is specific to lung cancer, while the CCDC6-RET fusion or the NCOA-RET fusion is common to both lung and thyroid cancers. RET fusions tend to be detected in young, female, and/or never/light-smoker patients with NSCLC (2,3,7-9).
It is noteworthy that the growth of RET fusion-positive tumor cells in vitro and in vivo can be suppressed by existing tyrosine kinase inhibitors (TKIs) that target RET protein, such as vandetanib, cabozantinib, and alectinib (4,7,10-13). Therefore, targeting the RET fusion with these agents holds promise for the treatment of NSCLC with RET kinase gene fusions, following the success for NSCLC with ALK kinase gene fusions (14). Our recent exome sequencing study indicated that lung cancers with RET or ALK fusions develop with exclusive dependence on oncogene fusions (15), suggesting that it is worthwhile examining the efficacy of RET-TKI monotherapy in lung cancer patients. Unfortunately, RET fusion-positive cases constitute only a small subset of all NSCLC cases. Positive tumors often show well- or moderately-differentiated histological features, similar to those carrying EGFR mutations, while, in some cases, such as those with the CCDC6-RET fusion, mucinous cribriform features similar to those of ALK fusion-positive tumors are observed (2,7-9). In addition, immune-histochemical staining of RET protein does not allow us to distinguish RET fusion-positive cases from others (3). Therefore, histological and immune-histological methods cannot be used for diagnosis. Thus, genetic tests, including fluorescence in situ hybridization, reverse transcription-PCR, and next-generation sequencing, are needed to identify RET fusion-positive NSCLC.
In a recent paper by Falchook et al. (16), vandetanib, a RET-TKI approved for the treatment of medullary thyroid carcinoma by the US Food and Drug Administration (FDA), was used to treat a patient with CCDC6-RET fusion-positive LADC. The patient was a 36-year-old, never-smoking woman, which is a characteristic of patients with this type of cancer up until now (2,3,7-9). She had widely metastatic lung cancer and was positive for the RET fusion as diagnosed by next-generation sequencing of a neck lymph node tumor sample by Foundation Medicine (Cambridge, MA, USA), one of the groups who discovered the RET fusion in lung cancer (1). The results of the study strongly indicated that vandetanib is a promising TKI for the treatment of this type of tumor. A Computed Tomography (CT) scan after 6 weeks of treatment demonstrated a dramatic response in the size of a large tumor mass in the left supraclavicular fossa, and CT scans at 11 weeks demonstrated a 76% decrease in tumor size as measured by RECIST version 1.1.
Currently, at least seven clinical trials are ongoing worldwide to examine the therapeutic utility of RET-TKIs against RET fusion-positive NSCLC (Table 1). All the studies have single-arm open-label designs, with the response rate as the primary endpoint; only RET fusion-positive NSCLC patients have been enrolled and all are being treated only with RET-TKIs. The trials are coupled with genetic screening, as exemplified by the Japanese study “LURET (UMIN000010095)”, which is coupled to the nation-wide screening program “SCRUM-Japan” (11,17). Preliminary results of one of the trials (NCT01639508 in Table 1) have been published. Cabozantinib, another FDA-approved RET-TKI, was found to have antitumor activity in all of the three patients participating in the study (18). Falchook’s case report (16), as well as another previous case report (19), indicated that not only cabozantinib but also vandetanib has potential for the treatment of RET fusion-positive NSCLC. In fact, vandetanib is being tested in two of the eight clinical trials (UMIN000010095 and NCT01823068 in Table 1) and promising results were reported (20). Taken together, these studies suggest that precision lung cancer medicine will be vastly improved by the addition of vandetanib as a therapeutic modality for patients with RET fusion-positive LADC.
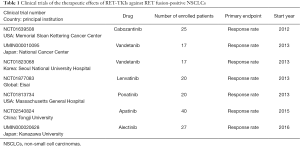
Full table
Acknowledgments
Funding: The author received a grant from Japan Agency for Medical Research and Development (16ck0106012h0003).
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Wei Xu (Division of Respiratory Disease, Department of Geriatrics, the First Affiliated Hospital of Nanjing Medical University, Nanjing, China).
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.08.10). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lipson D, Capelletti M, Yelensky R, et al. Identification of new ALK and RET gene fusions from colorectal and lung cancer biopsies. Nat Med 2012;18:382-4. [Crossref] [PubMed]
- Takeuchi K, Soda M, Togashi Y, et al. RET, ROS1 and ALK fusions in lung cancer. Nat Med 2012;18:378-81. [Crossref] [PubMed]
- Kohno T, Ichikawa H, Totoki Y, et al. KIF5B-RET fusions in lung adenocarcinoma. Nat Med 2012;18:375-7. [Crossref] [PubMed]
- Saito M. A mouse model of KIF5B-RET fusion-dependent lung tumorigenesis. Carcinogenesis 2014;35:2452-6. [Crossref] [PubMed]
- Lee MS, Kim RN. Identification of a novel partner gene, KIAA1217, fused to RET: Functional characterization and inhibitor sensitivity of two isoforms in lung adenocarcinoma. Oncotarget 2016; [Epub ahead of print]. [Crossref] [PubMed]
- Kohno T, Nakaoku T, Tsuta K, et al. Beyond ALK-RET, ROS1 and other oncogene fusions in lung cancer. Transl Lung Cancer Res 2015;4:156-64. [PubMed]
- Tsuta K, Kohno T, Yoshida A, et al. RET-rearranged non-small-cell lung carcinoma: a clinicopathological and molecular analysis. Br J Cancer 2014;110:1571-8. [Crossref] [PubMed]
- Pan Y, Zhang Y, Li Y, et al. ALK, ROS1 and RET fusions in 1139 lung adenocarcinomas: a comprehensive study of common and fusion pattern-specific clinicopathologic, histologic and cytologic features. Lung Cancer 2014;84:121-6. [Crossref] [PubMed]
- Wang R, Hu H, Pan Y, et al. RET fusions define a unique molecular and clinicopathologic subtype of non-small-cell lung cancer. J Clin Oncol 2012;30:4352-9. [Crossref] [PubMed]
- Nakaoku T, Tsuta K, Ichikawa H, et al. Druggable oncogene fusions in invasive mucinous lung adenocarcinoma. Clin Cancer Res 2014;20:3087-93. [Crossref] [PubMed]
- Kohno T, Tsuta K, Tsuchihara K, et al. RET fusion gene: translation to personalized lung cancer therapy. Cancer Sci 2013;104:1396-400. [Crossref] [PubMed]
- Suzuki M, Makinoshima H, Matsumoto S, et al. Identification of a lung adenocarcinoma cell line with CCDC6-RET fusion gene and the effect of RET inhibitors in vitro and in vivo. Cancer Sci 2013;104:896-903. [Crossref] [PubMed]
- Kodama T, Tsukaguchi T, Satoh Y, et al. Alectinib shows potent antitumor activity against RET-rearranged non-small cell lung cancer. Mol Cancer Ther 2014;13:2910-8. [Crossref] [PubMed]
- Awad MM, Shaw AT. ALK inhibitors in non-small cell lung cancer: crizotinib and beyond. Clin Adv Hematol Oncol 2014;12:429-39. [PubMed]
- Saito M, Shimada Y, Shiraishi K, et al. Development of lung adenocarcinomas with exclusive dependence on oncogene fusions. Cancer Res 2015;75:2264-71. [Crossref] [PubMed]
- Falchook GS, Ordóñez NG, Bastida CC, et al. Effect of the RET Inhibitor Vandetanib in a Patient With RET Fusion-Positive Metastatic Non-Small-Cell Lung Cancer. J Clin Oncol 2016;34:e141-4. [Crossref] [PubMed]
- Biankin AV, Piantadosi S, Hollingsworth SJ. Patient-centric trials for therapeutic development in precision oncology. Nature 2015;526:361-70. [Crossref] [PubMed]
- Drilon A, Wang L, Hasanovic A, et al. Response to Cabozantinib in patients with RET fusion-positive lung adenocarcinomas. Cancer Discov 2013;3:630-5. [Crossref] [PubMed]
- Gautschi O, Zander T, Keller FA, et al. A patient with lung adenocarcinoma and RET fusion treated with vandetanib. J Thorac Oncol 2013;8:e43-4. [Crossref] [PubMed]
- Seto T, Yoh K, Satouchi M, et al. A phase II open-label single-arm study of vandetanib in patients with advanced RET-rearranged non-small cell lung cancer (NSCLC): Luret study. J Clin Oncol 2016;34 (suppl; abstr 9012).


