
Emerging molecular pathways and targets in neuroendocrine prostate cancer
Introduction
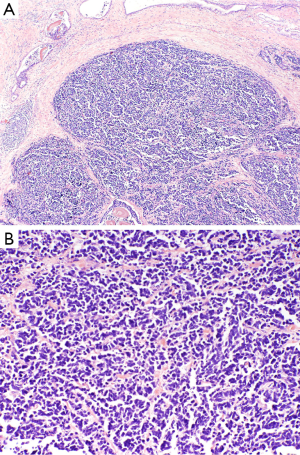
Small cell prostate cancer remains a poorly understood, aggressive form of prostate cancer that comprises less than 2% of prostate cancer diagnoses (1-6). Small cell prostate cancer remains a histological diagnosis and develops either de novo in patients with no prior history of prostate adenocarcinoma or, more commonly, in the setting of a patient with castrate resistant prostate cancer (Figure 1). The molecular underpinnings that determine which patients develop small cell prostate cancer in the de novo or castrate-resistant setting are not well defined although significant research is ongoing.
Mutations
Among the genetic mutations most commonly described in small cell prostate cancer, p53 and TMPRSS2-ERG are most common (1-6). TMPRSS2-ERG rearrangements are present in approximately half of small cell prostate cancer cases and are of particular value as they are not seen in other forms of small cell carcinomas (1-6). Interestingly, recent research has reported that TMPRSS2-ERG rearrangements can be associated with androgen receptor upregulation which may be associated with disease progression (7-10). Aurora kinase A (AURKA) and N-myc (NMYC) mutations are more commonly reported in small cell prostate cancer than in traditional prostatic adenocarcinoma, with a recent study reporting that 40% of small cell prostate cancer cases compared with 5% of prostatic adenocarcinoma had associated AURKA and NMYC overexpression (11). Further studies have suggested that up to 65% of small cell prostate cancer specimens and 86% of metastatic small cell prostate cancer specimens have AURKA amplification (12).
A recent article by Lee et al. provided the first pre-clinical study demonstrating the role that overexpression of NMYC maintains in the development of small cell prostate cancer (13). In this study the researchers examined human epithelial prostate cancer cells—a first as prior studies have almost exclusively studied xenografts. The researchers isolated benign prostate tissue from prostatectomy specimens and enforced expression of NMYC with eventual development of both adenocarcinoma and small cell prostate cancer in the previously benign prostate tissue. They further demonstrated that the tumors generated by NMYC over expression were both invasive and lacking androgen receptor expression, rendering the tumor castrate resistant (13).
Development
Multiple theories for the development of small cell prostate cancer exist. Many argue in favor of a divergent clonal evolution in which small cell prostate cancer develops from castrate resistant prostatic adenocarcinoma through epigenetic changes associated with cell plasticity and androgen receptor signaling (14). Alternatively, researchers have suggested that small cell prostate cancer represents dedifferentiation of adenocarcinoma, which is supported by the common finding of concomitant small cell prostate cancer with prostatic adenocarcinoma (15-17). Finally, research has suggested that the basal progenitor cells of the prostate may give rise to both traditional prostatic adenocarcinoma and the neuroendocrine cells observed in small cell prostate cancer (17-20).
In their recent study, Lee et al. report that the progenitor cells for adenocarcinoma in the prostate were able to transform into small cell prostate cancer when there was overexpression of NMYC, which supports the theory of a common basal progenitor cell (13). Furthermore, they report that increased expression of the malignant cells in the setting of castrate resistance results in further propagation of the small cell prostate cancer as opposed to adenocarcinoma (13). They propose that NMYC overexpression may enable stem cell progenitors to repopulate prostatic based tumors after treatment. Significant research is still required to fully understand the mechanisms underlying the development of small cell prostate cancer.
Therapeutics
While understanding the pathogenesis of small cell prostate cancer remains a critical area of research, the true benefit in determining its molecular underpinnings lies in the ability to identify molecular targets upon which medications can intervene and therapeutics can be designed. The recent study by Lee et al. is therefore a significant step forward as it demonstrated that NMYC is essential in maintaining the tumor through the AURKA pathway. With this in mind, the rationale behind AURKA inhibitors as therapeutic targets is strengthened. Using CD532, a novel therapeutic that interferes with the AURKA-NMYC complex (21), Lee et al. were able to demonstrate a significant decrease in NMYC activity in human prostate epithelial cells (13). This provides evidence that the AURKA and NMYC pathways may be excellent targets in the treatment of patients with NMYC overexpression small cell prostate cancer.
Prior therapeutic interventions for small cell prostate cancer have been directed by treatments for small cell cancer of the lung. Traditionally this includes cisplatin and etoposide. A study evaluating the role of docetaxel failed to demonstrate a benefit beyond that provided by cisplatin and etoposide alone (22). Beltran et al. evaluated the role of danusertib, an AURKA inhibitor, in both prostate adenocarcinoma and small cell prostate cancer. They reported that there was increased efficacy in patients who had NMYC and AURKA overexpression (11). Additional research is being performed using MLN8237/alisertib, a different AURKA inhibitor that is undergoing investigation in the setting of small cell prostate cancer and small cell cancer of the lung, although preliminary results have not yet demonstrated significant benefit (23). The research by Lee et al. demonstrating a benefit when using CD532 lends further credence to continued evaluation of NMYC and AURKA as therapeutic targets in small cell prostate cancer (13).
Continued research into the pathogenesis of small cell prostate cancer remains essential in determining therapeutic options. Recognizing the role that TMPRSS2-ERG fusion rearrangements play in small cell prostate cancer, recent studies have examined whether poly (ADP ribose) polymerase 2 (PARP1) inhibitors, which interact with ERG in prostate cancer cells, may offer an additional drug target. A recent phase 2 clinical trial of olaparib reported that 33% (n=16/49) of metastatic prostate cancer patients responded to treatment in the setting of failed treatment with docetaxel, abiraterone, enzalutamide, or cabazitaxel (24). Although this was not limited to patients with small cell prostate cancer, it is reasonable to conclude that small cell prostate cancer patients would similarly benefit based on our current understanding of the pathogenesis of small cell prostate cancer.
Conclusions
Based on the work of Lee et al., it is increasingly evident that NMYC plays a crucial role in both the initiation and propagation of small cell prostate cancer. These findings support what has been previously suspected and proposed but never demonstrated in human epithelial prostate cancer cells. Recognizing the essential role of NMYC provides an opportunity for targeted therapeutics that may revolutionize the treatments we use in the setting of small cell prostate cancer.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Peng Zhang (Department of Urology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.07.36). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang L, Davidson DD, Montironi R, et al. Small cell carcinoma of the prostate: molecular basis and clinical implications. Histol Histopathol 2015;30:413-24. [PubMed]
- Hansel DE, Nakayama M, Luo J, et al. Shared TP53 gene mutation in morphologically and phenotypically distinct concurrent primary small cell neuroendocrine carcinoma and adenocarcinoma of the prostate. Prostate 2009;69:603-9. [Crossref] [PubMed]
- Priemer DS, Montironi R, Wang L, et al. Neuroendocrine Tumors of the Prostate: Emerging Insights from Molecular Data and Updates to the 2016 World Health Organization Classification. Endocr Pathol 2016;27:123-35. [Crossref] [PubMed]
- Williamson SR, Zhang S, Yao JL, et al. ERG-TMPRSS2 rearrangement is shared by concurrent prostatic adenocarcinoma and prostatic small cell carcinoma and absent in small cell carcinoma of the urinary bladder: evidence supporting monoclonal origin. Mod Pathol 2011;24:1120-7. [Crossref] [PubMed]
- Schelling LA, Williamson SR, Zhang S, et al. Frequent TMPRSS2-ERG rearrangement in prostatic small cell carcinoma detected by fluorescence in situ hybridization: the superiority of fluorescence in situ hybridization over ERG immunohistochemistry. Hum Pathol 2013;44:2227-33. [Crossref] [PubMed]
- Cheng L, Bostwick DG. editors. Essentials of Anatomic Pathology. 4th edition. New York: Springer, 2016.
- Cai C, Wang H, Xu Y, et al. Reactivation of androgen receptor-regulated TMPRSS2:ERG gene expression in castration-resistant prostate cancer. Cancer Res 2009;69:6027-32. [Crossref] [PubMed]
- Debes JD, Tindall DJ. Mechanisms of androgen-refractory prostate cancer. N Engl J Med 2004;351:1488-90. [Crossref] [PubMed]
- Linja MJ, Savinainen KJ, Saramäki OR, et al. Amplification and overexpression of androgen receptor gene in hormone-refractory prostate cancer. Cancer Res 2001;61:3550-5. [PubMed]
- Scher HI, Sawyers CL. Biology of progressive, castration-resistant prostate cancer: directed therapies targeting the androgen-receptor signaling axis. J Clin Oncol 2005;23:8253-61. [Crossref] [PubMed]
- Beltran H, Rickman DS, Park K, et al. Molecular characterization of neuroendocrine prostate cancer and identification of new drug targets. Cancer Discov 2011;1:487-95. [Crossref] [PubMed]
- Mosquera JM, Beltran H, Park K, et al. Concurrent AURKA and MYCN gene amplifications are harbingers of lethal treatment-related neuroendocrine prostate cancer. Neoplasia 2013;15:1-10. [Crossref] [PubMed]
- Lee JK, Phillips JW, Smith BA, et al. N-Myc Drives Neuroendocrine Prostate Cancer Initiated from Human Prostate Epithelial Cells. Cancer Cell 2016;29:536-47. [Crossref] [PubMed]
- Beltran H, Prandi D, Mosquera JM, et al. Divergent clonal evolution of castration-resistant neuroendocrine prostate cancer. Nat Med 2016;22:298-305. [Crossref] [PubMed]
- Vlachostergios PJ, Papandreou CN. Targeting neuroendocrine prostate cancer: molecular and clinical perspectives. Front Oncol 2015;5:6. [Crossref] [PubMed]
- Yao JL, Madeb R, Bourne P, et al. Small cell carcinoma of the prostate: an immunohistochemical study. Am J Surg Pathol 2006;30:705-12. [Crossref] [PubMed]
- Spiess PE, Pettaway CA, Vakar-Lopez F, et al. Treatment outcomes of small cell carcinoma of the prostate: a single-center study. Cancer 2007;110:1729-37. [Crossref] [PubMed]
- Tan HL, Sood A, Rahimi HA, et al. Rb loss is characteristic of prostatic small cell neuroendocrine carcinoma. Clin Cancer Res 2014;20:890-903. [Crossref] [PubMed]
- Beltran H, Rubin MA. New strategies in prostate cancer: translating genomics into the clinic. Clin Cancer Res 2013;19:517-23. [Crossref] [PubMed]
- Lin PC, Giannopoulou EG, Park K, et al. Epigenomic alterations in localized and advanced prostate cancer. Neoplasia 2013;15:373-83. [Crossref] [PubMed]
- Gustafson WC, Meyerowitz JG, Nekritz EA, et al. Drugging MYCN through an allosteric transition in Aurora kinase A. Cancer Cell 2014;26:414-27. [Crossref] [PubMed]
- Papandreou CN, Daliani DD, Thall PF, et al. Results of a phase II study with doxorubicin, etoposide, and cisplatin in patients with fully characterized small-cell carcinoma of the prostate. J Clin Oncol 2002;20:3072-80. [Crossref] [PubMed]
- Carver BS. Defining and Targeting the Oncogenic Drivers of Neuroendocrine Prostate Cancer. Cancer Cell 2016;29:431-2. [Crossref] [PubMed]
- Mateo J, Carreira S, Sandhu S, et al. DNA-Repair Defects and Olaparib in Metastatic Prostate Cancer. N Engl J Med 2015;373:1697-708. [Crossref] [PubMed]


