
Long-term safety of targeted agents used to treat metastatic renal cell carcinoma: the issue is not the rate of adverse events over time, but the expertise needed to manage them
Targeted agents have revolutionized the treatment of advanced renal cell carcinoma (RCC), greatly improving the survival of patients affected with once orphan disease.
Although the median progression-free survival of patients treated in first-line, irrespective of the agent used, is between 9 to 11 months, a relevant number of patients do receive such a treatment for a longer period of time.
Thus, knowing not only acute, but also long-term toxicities of the agents we do use is mandatory and, given the data available for some of these agents (1,2), also reassuring (3).
However, in order to achieve even better results in terms of treatment duration, and thus disease control, we should try to increase the number of patients who are treated long-term.
However, one could argue that this is an almost impossible task, at least with presently available agents, since the development of acquired resistance appears to be ineluctable and tightly linked to the biology of the tumor itself (4).
Nevertheless, it is clear that too many patients discontinue first-line treatment (as well as subsequent lines), not for disease progression (or, if you want, before disease progression) due to toxicity. Is this again ineluctable?
We do think this is not the case.
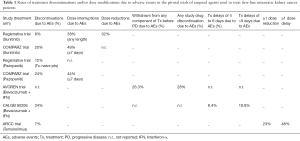
When taking a look at the rates of treatment discontinuation due to adverse events reported in pivotal trials of agents used in first-line (Table 1), we recognize that this is a huge problem, despite the fact that this trials have been conducted at experienced, referral, sites with time, experience and staff devoted to the management of these patients and their treatment.
Full table
Although it is difficult to demonstrate, the rate of treatment interruptions and discontinuations outside clinical trials is realistically higher, especially in low-volume centers.
Notwithstanding, all the above proved to have a detrimental effect on treatment’s outcome; indeed, it has been previously demonstrated that a low dose-intensity correlates with a poor prognosis in metastatic RCC patients treated with different agents (5), strengthening, from a clinical viewpoint, informations we already gathered from pharmacokinetic studies (6).
This is all but strange, since we do know, form the old times of cytotoxic chemotherapy for metastatic breast cancer (7), that a direct relationship exist between a correct dose intensity (i.e., dose per unit of time) and treatment efficacy.
Finding agents endowed by a better therapeutic index is certainly mandatory in kidney cancer as well as in many other malignancies, but exploiting at its best what we presently have, in terms of treatment armamentarium, is even more important.
For sure, dose reductions, schedule modifications and even treatment discontinuations will continue to be necessary for many cancer patients with the present array of anticancer agents (and probably also with the next generation of them), but we should be brave enough not only to say to our patients to keep treatment going, because it will be realistically better tolerated over time, but also to teach them to prevent and manage, as much as possible (which definitely means not in every case), treatment-related adverse events, both acute and chronic.
To conclude, we cannot but recall Chris Ryan’s words at the 2010 American Society of Medical Oncology annual meeting, words which were subsequently endorsed by many of us in the field of RCC (8), “use any agent you want, but use it well”.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Hong-chao He MD, PhD (Department of Urology, Shanghai Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China).
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.09.41). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Porta C, Gore ME, Rini BI, et al. Long-term Safety of Sunitinib in Metastatic Renal Cell Carcinoma. Eur Urol 2016;69:345-51. [Crossref] [PubMed]
- Hutson TE, Bellmunt J, Porta C, et al. Long-term safety of sorafenib in advanced renal cell carcinoma: follow-up of patients from phase III TARGET. Eur J Cancer 2010;46:2432-40. [Crossref] [PubMed]
- Michel C, Thibault C, Oudard S. Long-term use of sunitinib in metastatic renal cell carcinoma: no unpleasant surprises about tolerability. Transl Cancer Res 2016;5:S261-3. [Crossref]
- Buczek M, Escudier B, Bartnik E, et al. Resistance to tyrosine kinase inhibitors in clear cell renal cell carcinoma: from the patient's bed to molecular mechanisms. Biochim Biophys Acta 2014;1845:31-41.
- Porta C, Levy A, Hawkins R, et al. Impact of adverse events, treatment modifications, and dose intensity on survival among patients with advanced renal cell carcinoma treated with first-line sunitinib: a medical chart review across ten centers in five European countries. Cancer Med 2014;3:1517-26. [Crossref] [PubMed]
- Houk BE, Bello CL, Poland B, et al. Relationship between exposure to sunitinib and efficacy and tolerability endpoints in patients with cancer: results of a pharmacokinetic/pharmacodynamic meta-analysis. Cancer Chemother Pharmacol 2010;66:357-71. [Crossref] [PubMed]
- Hryniuk W, Bush H. The importance of dose intensity in chemotherapy of metastatic breast cancer. J Clin Oncol 1984;2:1281-8. [PubMed]
- Porta C. Entropy increases in kidney cancer treatment, but a bit of simplicity may emerge from chaos. Eur Urol 2011;60:1171-2. [Crossref] [PubMed]


