
Is there still a role for tremelimumab in the treatment of cancer?
It was surprising to first learn, at the 2008 ASCO annual meeting, that the phase III trial of tremelimumab for the treatment of advanced melanoma did not have a positive result with regard to its primary endpoint. After very promising data in phase II studies, the difference in overall survival (OS) between the tremelimumab and standard of care control (temozolomide or dacarbazine) arms was not statistically significant (11.8 versus 10.7 months). Despite this, at that point in time, an OS of 11.8 months for advanced melanoma patients seemed exceptional, given the historical median OS of 6-8 months for these patients (1).
Around this time, there were great expectations regarding the treatment of melanoma with anti-cytotoxic T lymphocyte-associated antigen-4 (CTLA-4) blocking therapies. Defeating the tumor through potentiating the immune system has long been the dream of the immune-oncologist, especially those dedicated to the treatment of melanoma. Unfortunately, several studies had previously failed to demonstrate efficacy of an immunotherapeutic approach (primarily vaccination) in curing this cancer (2) and had discouraged even the strongest supporter of immunotherapy. In the same period, the first data from phase II studies of ipilimumab began to appear and were the basis of some innovative concepts such as the immune-related response criteria (irRC) (3) and algorithms for the management of toxicity (4). Of course, these concepts were not known until after the tremelimumab study had first reported.
Now the final results of the tremelimumab phase III trial by Ribas et al. have been published in full (5). In the 655 enrolled patients, the median OS was 12.6 months for tremelimumab and 10.7 months (confirmed) for temozolomide or dacarbazine. Objective response rates (ORR) were similar in the two arms, 10.7% with tremelimumab and 9.8% with chemotherapy. The survival rates after 2 and 3 years were 26.4% and 20.7% in patients treated with tremelimumab. The probability of progression-free survival (PFS) at 6 months was similar in the two arms: 20.3% with tremelimumab and 18.1% with chemotherapy. However, duration of response was clearly longer in the anti-CTLA-4 arm (35.8 vs. 13.7 months).
Looking at these data, the first notable observation is the similarity between those for tremelimumab and those previously seen with ipilimumab. In fact, the median OS of 12.6 months with tremelimumab in this study is actually better than those seen with ipilimumab in either the MDX010-020 (6) or CA184-024 trials (7). The 2- and 3-year survival rates with tremelimumab are also consistent with those reported for ipilimumab (Table 1). In addition, the lack of any significant differences between treatment arms in surrogates outcomes (ORR and PFS at six months) in the tremelimumab study was also seen with ipilimumab. Moreover, the safety profile of tremelimumab is similar to that of ipilimumab, with only minor differences in the percentages of patients reporting adverse events.
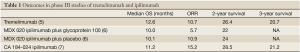
Full table
So if these tremelimumab results are not so different from those seen with ipilimumab, why was the study negative? The second key observation is the remarkable 10.7-month survival achieved in the dacarbazine/temozolomide treatment arm. An explanation for this may lie with two main contributory factors. The first is that patients with LDH >2× ULN were excluded from the study, meaning the trial may have selected patients likely to have better outcomes. This could have had the effect of reducing any difference in survival between the two groups. In fact, another recent phase III trial that also excluded patients with LDH >2× ULN reported an identical median OS of 10.7 months with dacarbazine (versus the new chemotherapeutic agent, abraxane) (8). A second factor that may also help explain the better than expected survival in the control arm is that 14% of chemotherapy-treated patients received ipilimumab after disease progression.
Another observation is that the median OS of 12.6 months with tremelimumab was obtained with a schedule of treatment that provided an infusion every 90 days with a dosage of 15 mg/kg for up to 4 cycles. The previous phase II trial had reported no apparent difference between two different regimens (10 mg/kg once monthly and 15 mg/kg once every 3 months) with regard to response rate or survival (although there was a trend toward increased toxicity with 10 mg/kg once monthly) (9). However, results of the ipilimumab trials with a once every three weeks schedule raised questions over the suitability of this particular long-term schedule. The median duration of treatment in the tremelimumab arm was 3.0 months and about 60% of patients treated with tremelimumab received just one cycle of treatment. The explanation given for this is that the irRC were not known when this study was designed, and the assessment was scheduled at week 12, before starting the second administration of anti-CTLA-4. However, we now know that anti-CTLA-4 therapy has a slow onset of action and that around 10% of patients who appear to have progressive disease after starting treatment will actually have a subsequent response. Despite the use of every 90-days infusion and the fact that about the 60% of patients received just a single cycle of tremelimumab, an important result in term of overall survival was still achieved.
In conclusion, in analysing the seemingly disappointing result of the tremelimumab phase III trial, we have to consider several points: the unexpectedly good outcome in the control arm, possibly due to the enrollment of patients with a more favourable prognosis and use of ipilimumab in some, and the use of a potentially sub-optimal 90-days schedule of treatment in the tremelimumab arm. However, even despite these factors, achieving a median OS of 12.6 months is deserving of respect and, overall, these data support the view that tremelimumab may have a role in the treatment of cancer, not only of melanoma.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.3978/j.issn.2218-676X.2013.02.02). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Korn EL, Liu PY, Lee SJ, et al. Meta-analysis of phase II cooperative group trials in metastatic stage IV melanoma to determine progression-free and overall survival benchmarks for future phase II trials. J Clin Oncol 2008;26:527-34. [PubMed]
- Eggermont AM. Therapeutic vaccines in solid tumours: can they be harmful? Eur J Cancer 2009;45:2087-90. [PubMed]
- Wolchok JD, Hoos A, O’Day S, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res 2009;15:7412-20. [PubMed]
- Boasberg P, Hamid O, O’Day S. Ipilimumab: unleashing the power of the immune system through CTLA-4 blockade. Semin Oncol 2010;37:440-9. [PubMed]
- Ribas A, Kefford R, Marshall MA, et al. Phase III Randomized Clinical Trial Comparing Tremelimumab With Standard-of-Care Chemotherapy in Patients With Advanced Melanoma. J Clin Oncol 2013;31:616-22. [PubMed]
- Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 2010;363:711-23. [PubMed]
- Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med 2011;364:2517-26. [PubMed]
- Hersh E, Del Vecchio M, Brown M, et al. Phase 3, randomized, open-label, multicenter trial of nab-paclitaxel (nab-P) versus dacarbazine (DTIC) in previously untreated patients with metastatic malignant melanoma (MMM). Pigment Cell Melanoma Res 2012;25:863.
- Camacho LH, Antonia S, Sosman J, et al. Phase I/II trial of tremelimumab in patients with metastatic melanoma. J Clin Oncol 2009;27:1075-81. [PubMed]


