
Epidemiology characteristics of ethnic minority colorectal cancer in Yunnan in Southwestern China
Introduction
Colorectal cancer (CRC) including colon cancer and rectal cancer is a common malignant tumor. The incidence and mortality of this cancer are both ranked as third among malignant tumors (1,2). Although the threat of CRC in China is not as severe as in developed countries, an upward trend has been seen in recent years. According to the most recent data from the National Central Cancer Registry of China (NCCRC), the total number of CRC cases increased from 347,900 (199,700 males and 148,200 females) to 376,300 (215,700 males and 160,600 females) in the period from 2009 to 2011 (3,4). Moreover, according to the 2016 Global Burden of Diseases Study, CRC-related cases and deaths in China are currently 392,800 and 167,100, respectively, with a predicted increase by 2025 to 642,300 and 221,100, respectively (5).
The pathogenesis of CRC is mainly attributed to colorectal adenoma, inflammatory bowel disease, and familial hereditary polyposis. In particular, colorectal adenocarcinoma (CRA), a pathological type of CRC, accounts for 85–90% of CRC precancerous lesions (6). A large number of etiology studies have shown that the development of CRA is a multi-stage, multi-step, multi-gene participation process resulting from a synergy of environmental, dietary, lifestyle, and genetic factors (7).
Nowadays, few effective methods for CRC screening exist. The most common screening methods are relatively obvious physical changes such as fecal occult blood and polyps, although these clinical signs cannot completely prevent the occurrence of CRC (8). Some genetic screening techniques for CRC, such as the screening for mutations in B-Raf proto-oncogene, serine/threonine kinase (BRAF), MutL homolog 1 (MLH1), KRAS Proto-Oncogene, GTPase (K-RAS), the APC regulator of the WNT signaling pathway (APC) and tumor protein p53 (P53), Phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA), and SMAD family member 4 (SMAD4), can be used to identify potential high-risk factors for CRC (9-11). Furthermore, carcinoembryonic antigen (CEA) is a new marker of CRA which was originally found to be expressed in the fetal intestine, liver, and pancreas at 8-20 weeks in adults when tumors manifest. Positive serum CEA is present in gastrointestinal tumors and is found in 70% to 90% of patients with CRA (12). Similar tumor antigens include carbohydrate antigens (CA) such as CA50, CA19-9, CA242 and CA724 (13,14). However, these genetic screening techniques are not yet widely available for screening for CRC prevention due to the immature technology and substandard medical level in Yunnan.
CRA has become a public health problem in China, owing to the changes seen in modern lifestyles and dietary habits, with its rapidly rising incidence and mortality. China is a multi-ethnic country with more than 1.3 billion people and 56 ethnic groups, and Yunnan is a region that contains 25 of them. Most of the ethnic groups have their social settlements, unique customs, and lifestyles. Such a special population composition enables systematic research on CRC to be performed in Yunnan taking into account socio-cultural and biological factors, which have great practical significance for the effective prevention and early diagnosis of CRC. In this study, 1,016 cases of CRC patients from Yunnan Cancer Hospital in the period from 2013 to 2018 were collected and summarized to explore the relationship between special lifestyle and CRC among the ethnic minority population. The results could provide a scientific basis for identifying the risk factors of CRC and for the establishment of practical etiological blockade and prevention and treatment measures.
Methods
Materials
A total of 1,016 patients with CRA, comprising 587 males and 429 females aged 30 to 79 years old, were involved in this study. Clinical data were collected by Yunnan Cancer Hospital from January 2013 to December 2018. The diagnosis of colon cancer and rectal cancer in each patient was confirmed by pathological biopsy. In addition, 1,001 patients with non-tumor colon diseases were also recruited from Yunnan Cancer Hospital between January 2013 and December 2018. These patients comprised 576 males and 425 females, aged from 28–80 years old, with an average age of (55.30±12.69) years old. There were no significant differences in age, gender or ethnic composition, educational background or other conventional data between the colon cancer patients and the matched patients.
Methodology
Yunnan Cancer Hospital collected all cases of diagnosed CRA from 2013 to 2018, and these cases were compared according to gender, age group, ethnic group, and regions.
Grouping
Cases were divided according to gender into male and female groups. By age, cases were divided into 3 groups: those under 40 years of age, those aged between 40 and 60 years of age, and those above 60 years of age. According to the prefecture group, there were a total of 16 geographical groups: 8 prefecture-level cities in Yunnan (Kunming, Qujing, Yuxi, Zhaotong, Baoshan, Lijiang, Pu’er, and Lincang), and 8 autonomous prefectures (Dehong Dai Jingpo Autonomous Prefecture, Dali Bai Autonomous Prefecture, Chuxiong Yi Autonomous Prefecture, Honghe Hani and Yi Autonomous Prefecture, Wenshan Zhuang and Miao Autonomous Prefecture, Xishuangbanna Dai Autonomous Prefecture, Nujiang Yi Autonomous Prefecture, and Diqing Tibetan Autonomous Prefecture).
Statistical methods
Data were processed by Epidata 3.1 for entry and grouping, and statistical analysis was performed by SPSS 17.0. The comparison between the data groups was performed by the x2 test, and P≤0.05 was considered statistically significant.
Results
Ethnic and gender distribution of CRC patients
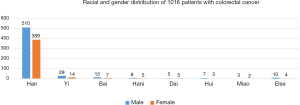
Among the 1,016 patients with CRC, 587 (57.78%) were male, and 429 (42.22%) were female, and the ratio of male to female was 1.37:1. A total of 899 (88.48%) of the patients were Han and 117 (11.52%) were from ethnic minorities, including 43 Yi, 22 Bai, 13 Hani, 10 Dai, 10 Hui, 5 Miao, and 14 of other ethnic groups (Jingpo, Yi, Zhuang, Naxi, Laz, Pumi, Buyi, and Wa people). In terms of ethnic groups, Han showed a higher incidence of CRC among males than females, which may relate to differences in living habits between men and women (Figure 1). More research is needed to conduct further analysis and verification.
Age and regional distribution of CRC patients
Among the 1,016 patients with CRC, 72 (7.1%) were 40 years old or younger, 447 (44.0%) were distributed in the 40-to-60-year age range, and 497 (48.9%) were older than 60 years of age. The chi-square test indicated that the composition ratio of CRC patients in the different age groups was significantly different and enhanced significantly with age, showing the higher age, the higher incidence. Furthermore, more significance was shown in ethnic minority groups, and the incidence rates of different age groups were also different and statistically significant (P<0.05) (Tables 1 and 2).
Table 1
| Group | Age (year) |
|---|---|
| Male | |
| Mean | 55.23 |
| Median | 57 |
| Mode | 62 |
| Female | |
| Mean | 54.05 |
| Median | 54 |
| Mode | 54 |
| Total | |
| Mean | 54.77 |
| Median | 55 |
| Mode | 62 |
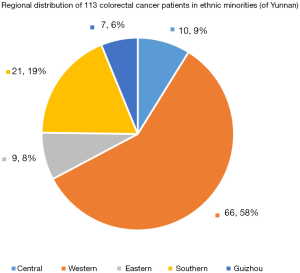
The distribution of 113 CRC cases (4 of the 117 cases were in Guizhou) among ethnic minorities in Yunnan is shown in Figure 2: 66 cases (58%) were in western Yunnan, 21 cases (19%) in southern Yunnan, 10 cases (9%) in central Yunnan, 9 cases (8%) in eastern Yunnan, and 7 cases in Guizhou (6%). Ethnic minorities in Yunnan mainly live in western Yunnan, which covers the largest area. These results taken together indicate that there are more minority patients with CRC in western Yunnan (Figure 2).
Lifestyle habits of minority patients with CRC
Based on the information above, we found that the incidence of CRC in ethnic minorities is similar to that in the Han population. The number of CRC patients over 40 years old made up more than 90% of the total number, which backs up the fact that there is a higher incidence of CRC in older patients. However, the proportions of male and female patients with CRC were significantly out of balance, and the proportion of male patients was higher, which could be attributed to the unique lifestyle of ethnic minorities (Figure 1, Table 2).
Table 2
| Classification | Han | Minority | Total | P |
|---|---|---|---|---|
| Age | <0.05 | |||
| ≥60 | 445 (43.8) | 52 (5.1) | 497 (48.9) | |
| 40–60 | 405 (39.9) | 42 (4.1) | 447 (44.0) | |
| ≤40 | 53 (5.2) | 19 (1.9) | 72 (7.1) | |
| Total | 903 (88.9) | 113 (11.1) | 1,016 |
We, therefore, investigated the history of tobacco, alcohol, and family diseases in patients from ethnic minorities. In these cases, a higher prevalence of tobacco consumption was observed in the Yi people whose smoking history does not exceed 50 years and 10 cigarettes per day, followed by the Bai, Hani, Hui, Naxi, and Zhuang groups. In addition to the smoking habits of ethnic minorities in Yunnan, alcohol consumption history is also not negligible. In the cases of CRC patients examined, the Bai, Hani, Hui, and Naxi people were shown to be consuming an increasing amount of alcohol daily. The results showed that long-term smoking and drinking are significantly associated with the incidence of CRC, and this is more significant in ethnic minorities (P<0.05) (Table 3).
Table 3
| Factors | Minority | Han | Han cancer-free | x2 | P |
|---|---|---|---|---|---|
| History of smoking >5 years (>10 cigarettes per day) | 33.8 | <0.05 | |||
| Yes | 38 (33.6) | 152 (16.8) | 114 (12.7) | ||
| No | 75 (66.4) | 751 (83.1) | 781 (87.3) | ||
| Drinking history>5 years (>0.1 kg per day) | 17.4 | <0.05 | |||
| Yes | 26 (23.0) | 132 (14.6) | 94 (10.5) | ||
| No | 87 (77.0) | 771 (85.4) | 801 (89.5) |
CRC complaint symptoms
One reason why patients with CRC experienced a high rate of mortality is the high incidence and the undetectability of the disease. Most patients are already at the advanced stage when they receive their diagnosis, which brings great difficulties in terms of treatment and prognosis. We analyzed 82 cases of newly diagnosed rectal cancer with initial diagnosis and complaints from 2016–2018. According to the patient complaints, 45 cases (54.9%) were diagnosed due to fecal occult blood; 25 cases (30.5%) were diagnosed due to abdominal pain, diarrhea, digestive tract discomfort, and similar issues; 7 cases (8.5%) were diagnosed due to difficulty passing stools and/or constipation; and a very small number of patients (6.1%) were diagnosed due to coughing and coughing up blood, rectal occupation, loss of consciousness, and other symptoms (Table 4).
Table 4
| Variable | Complaint symptoms | Total | |||
|---|---|---|---|---|---|
| Fecal occult blood | Stomach ache | Poor stool | Other symptoms* | ||
| Cases | 45 | 25 | 7 | 5 | 82 |
| Percentage | 54.9% | 30.5% | 8.5% | 6.1% | 100% |
*Other symptoms include: cough and blood cough, rectal space, loss of consciousness, etc.
Discussion
CRC is attributed to several pathologic factors, including hereditary conditions, inflammatory bowel disease, smoking, excessive drinking, sustained exposure to red, processed meat (mainly processed four-legged animal meat), obesity, and diabetes (15,16). Although China is not a country with a high incidence of CRC, the incidence of CRC has shown a rapid upward trend in recent years (17). Therefore, the epidemiological investigation of CRC in Yunnan, a region with a high concentration of ethnic minorities, may facilitate our understanding of the etiology of this malignant disease and consequently help to reduce the incidence of CRC in Yunnan minority areas.
The results of this analysis showed that there was a significant difference in the ratio of males to females (1.37:1) among 1,016 patients with CRC. In Han patients, the ratio was 1.31:1, which was greater than that of the patients from ethnic minority populations. The incidence of CRC in males was significantly higher than in females, and this difference may be due to lifestyle habits. Most men in Yunnan have smoking and drinking habits, and these unhealthy behaviors are even more prevalent among ethnic minorities. We investigated tobacco and alcohol consumption history among 117 patients from ethnic minorities. Of these, 14 ethnic minorities with no history of family disease had a history of tobacco and alcohol consumption, and 43 Yi CRC patients, of whom 29 were male. Among these 29 cancer cases, 11cases had smoking history, 6 cases own drinking history, and the proportion of tobacco and alcohol history is higher. The traditions of the Yi and Hani people include hookah and barbecuing, whereas the diets of Bai and Yi people include lots of fermented, pickled raw food, strong tea, and white wine. These unhealthy living habits may be the cause of the high incidence of CRC among ethnic populations.
The high incidence of CRC closely related to modern diet habits. The diets of many ethnic minorities include a raw food diet, and long-term exposure leads to greater damage to the digestive tract. Many epidemiological investigations have shown that foods with saturated fat are associated with the incidence of CRC and that healthy eating habits can help to prevent CRC (18). A large number of studies have shown that long-term consumption of saturated fatty acid-foods could increase the incidence of CRC, as evidenced by the positive correlation between food intake frequency and CRC risk (19-22). Although a few studies have shown that there is not necessarily a link between the two, more research studies have supported the idea (23). Food with a high content of saturated fatty acid is highly common in Yunnan. Long-term consumption of high-protein dairy products increases the risk of CRC. Long-term drinking and smoking are also considered as high-risk factors for CRC. Studies have shown that alcohol exposure, regardless of the consumption amount, and long-term smoking can significantly increase the chances of developing multiple digestive tract cancers, including CRC (24-26). The risk to the Yunnan ethnic minority is increased because tobacco and alcohol consumption have featured in the history of Yunnan for a considerable amount of time, and it may also be related to the various traditions in ethnic minority cultures. Tobacco and alcohol cultural habits passed down from generation to generation are deeply rooted, especially among men who have a low level of education and have been greatly influenced by the previous generation. Digestive system disorders in the aging population, associated with the harsh diet of tobacco and alcohol, increase the risk of CRC. The CRC incidence in ethnic minorities is thus higher than that in the Han population, and such a difference was more significant when males and females were compared.
The National Cancer Network and the American Cancer Society have reported that individuals are at higher risk to CRC if they have a history of colorectal adenomas or pedunculated serrated polyps, abdominal or pelvic radiotherapy, CRC, or inflammatory bowel disease, or a history of the disease in their family (27). According to the Asia-Pacific Colorectal Cancer Working Group, the Chinese Society of Clinical Oncology, and several American cancer organizations, the general risk population should be screened for CRC upon reaching the age of 50, and people with normal risk should have a colonoscopy every 10 years or an annual fecal immuno-chemical test (FIT), while high-risk groups require different screening standards and guidelines based on different risk factors (28-30). According to the records and statistical analysis of 1016 cases in Yunnan Cancer Hospital from 2013 to 2018, the incidence of CRC was higher among the older group. The number of CRC patients over 60 years of age accounted for almost 50% of the total number of cases, and the average age of the affected population was 54.77 years old, which is consistent with the trend of many epidemiological statistics for CRC in China. Combined with the distribution of ethnic minorities in Yunnan Province, the total population of Yunnan Yi people is 4.79 million, and most of them settle across Yunnan. The Bai people have a population of 1.81 million, and their main settlement is Dali. Honghe Prefecture and Pu’er City are the main settlements of the Hani population (total population of 1.49 million). The Dai people (total population of 1.19 million) are mainly settled in the Dehong Prefecture and the Xishuangbanna Prefecture. The Hui people (total population of 720,000) settle throughout Yunnan. Interestingly, the distribution of rectal cancer was consistent with the proportion of the population of each ethnic group, and there was no obvious specificity in the ratio distribution of patients according to the distribution characteristics of the ethnic groups.
With regard to geographical distribution characteristics, there were 66 patients from ethnic minorities in western Yunnan. Western Yunnan was shown to be an area with a high incidence of CRC among ethnic minorities, and the 14 ethnic minorities in this region also matched this trend. The age distribution studies showed that 50–60 years old is the key age for screening and prevention of CRC in ethnic minorities, and a few high-risk groups should even be screened from 30–40 years old or earlier.
Internationally, there are four accepted protocols for the screening and diagnosis of CRC: (I) fecal occult blood test, which specifically detects the number of red blood cells in feces and is the most widely used method along with high sensitivity and specificity; (II) colonoscopy of rectal polyps (adenomas) to prevent disease progression; (III) fiber sigmoidoscopy, mainly for individuals who do not want to have a full colonoscopy; (IV) immunological fecal occult blood test—a fecal DNA test (Colo-guard), mainly to detect fecal KARS mutation, NDRG family member 4 (NDRG4) deletion, bone morphogenetic protein 3 (BMP3), and Syndecan-2 methylation indicators, while performing a fecal occult blood experiment (31,32). According to the 82 new cases in 2016–2018, fecal occult blood, abdominal pain, and diarrhea are the main symptoms of CRC in patients in Yunnan. The high mortality of CRC can be attributed to the difficulties surrounding early detection, as for many patients, the window for the most effective therapy is closed before they are diagnosed (33). Traditional ideas and concepts can deeply influence ethnic minority cultures, and so the concept of disease is weak among some ethnic minority populations. As a result, the awareness of risk symptoms among some groups is low, and physical examinations are rarely carried out regularly. Many cases of CRC complications (e.g., blood in stools or abdominal pain) or physical discomfort can appear for 1 year before admission to the hospital, resulting in delayed diagnosis and seriously compromising the treatment effect. In addition, Yunnan is located near Chinese southwestern border, the poor geographical environment of minority residential areas and inconvenient transportation led many patients to miss the best treatment time.
CRC prevention is divided into two levels: primary prevention and secondary prevention. Since the incidence of CRC is complex and diverse, primary prevention is the main focus. Indeed, preventive measures against specific causes in different regions can effectively reduce the incidence of diseases from the root causes. If primary prevention is not possible, secondary prevention can effectively reduce the mortality rate of CRC and reduce the loss of life. According to a domestic medical center study, the recurrence rate of progressive colorectal adenomas is as high as 59.46% within the first year and 78.07% within 5 years, with the recurrence concentrated at 1–2 years after polypectomy (34). At the European Society for Medical Oncology Asian Conference 2019 (ESMO Asia 2019), Professor Alberto Sobrero pointed out that to reduce the mortality of CRC, increasing the additional cure rate of adjuvant treatment is an important breakthrough. According to relevant statistics, the postoperative adjuvant treatment benefit of stage 2 colon cancer is about 2% to 5%, the benefit of stage 3 colon cancer is about 15%, and the recurrence period of CRC patients is as long as 8 years. As for the treatment of CRC, precision medicine requires the identification of a clear gene or a change in a signal pathway and treating the specific gene or a signal pathway as soon as possible. From this perspective, little progress has been made in the treatment of CRC.
Epidermal growth factor receptor (EGFR pathway) targeted drugs cetuximab and panitumumab block this pathway to have an anti-tumor effect (35). This is the first meaningful, targeted drug developed in the field of CRC, and it is also the only drug in the field of CRC that can be considered ad precision treatment. However, cetuximab alone is not an effective treatment for advanced BRAF mutant colon cancer, so a VIC scheme (verofinib, irinotecan, and cetuximab) is required to block EGFR signals at the source (36). Blocking BRAF is also recommended by the guidelines of both the National Comprehensive Cancer Network (NCCN) and the Chinese Society of Clinical Oncology (CSCO), and BRAF inhibitors combined with EGFR monoclonal antibodies are recommended to treat patients with advanced BRAF mutant CRC (37). Also, a “full block” treatment idea was proposed in the BEACON study that EGFR monoclonal antibody + BRAF inhibitor + MEK inhibitor was used to achieve EGFR full-path blockade to prevent BRAF from being activated by CRAF bypass (38). This would be a new treatment model for treating BRAF mutations in advanced CRC. The practice results of precision medicine have also suggested dividing the population according to molecular markers and then adding specific drugs, such as targeted drugs and immunotherapy drugs to specific groups based on previous standard treatments. This practice breaks the traditional concept of tumor treatment and also promotes a new transformation of the clinical treatment of tumors. Although the postoperative treatment of CRC is expected to improve, the prevention of CRC remains the most pressing issue.
In summary, CRC in Yunnan had a high incidence in older people, and this was more obvious in ethnic minorities. The incidence in males was also much higher among ethnic minorities than among the Han population. Combined with the results of our analysis, the high incidence of CRC in Yunnan is strongly related to lifestyle habits. In particular, higher tobacco and alcohol use has been observed in ethnic minority males than in the Han population, and the difference between men and women was also more significant. Therefore, the prevention and treatment of CRC among ethnic minorities in Yunnan should be focused on changing dietary and lifestyle habits, such as reducing tobacco and alcohol consumption and maintaining a balanced diet. Other priorities are improving awareness of disease prevention and control, and medical institutions effectively applying relevant screening criteria to screen different age groups according to different risk groups. Both patients and doctors should prioritize early screening and regular check for common tumor markers, to reduce the incidence and mortality of CRC and provide a basis for CRC treatment and prognosis improvement in Yunnan.
Acknowledgments
Funding: This work was supported by grants from
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2020.02.63). SW reports grants from the National Social Science Foundation of China, grants from the National Natural Science Foundation of China, during the conduct of the study; QT reports grants from the National Social Science Foundation of China, grants from the National Natural Science Foundation of China, during the conduct of the study; DF reports grants from the National Social Science Foundation of China, grants from the National Natural Science Foundation of China, during the conduct of the study; ZH reports grants from the National Social Science Foundation of China, grants from the National Natural Science Foundation of China, during the conduct of the study; WS reports grants from the National Social Science Foundation of China, grants from the National Natural Science Foundation of China, during the conduct of the study; YC reports grants from the National Social Science Foundation of China, grants from the National Natural Science Foundation of China, during the conduct of the study.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by Medical Ethics Committee of Kunming Medical University and written informed consent was obtained from all patients. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- GLOBOCAN 2018. International Agency for Research on Cancer. WHO 2018. Available online: http://gco.iarc.fr/, 2019.
- Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. [Crossref] [PubMed]
- Chen W, Zheng R, Zhang S, et al. Cancer incidence and mortality in China, 2013. Cancer Letters 2017;401:63-71. [Crossref] [PubMed]
- Pan R, Zhu M, Yu C, et al. Cancer incidence and mortality: A cohort study in China, 2008-2013. Int J Cancer 2017;141:1315-23. [Crossref] [PubMed]
- Zhang L, Cao F, Zhang G, et al. Trends in and Predictions of Colorectal Cancer Incidence and Mortality in China From 1990 to 2025. Front Oncol 2019;9:98. [Crossref] [PubMed]
- Diagnosis, Treatment Guidelines For Colorectal Cancer Working Group C. Chinese Society of Clinical Oncology (CSCO) diagnosis and treatment guidelines for colorectal cancer 2018 (English version). Chin J Cancer Res 2019;31:117-34. [Crossref] [PubMed]
- Thrumurthy SG, Thrumurthy SS, et al. Colorectal adenocarcinoma: risks, prevention and diagnosis. BMJ 2016;354:i3590. [Crossref] [PubMed]
- Bray C, Bell LN, Liang H, et al. Colorectal Cancer Screening. WMJ 2017;116:27-33. [PubMed]
- Midthun L, Shaheen S, Deisch J, et al. Concomitant KRAS and BRAF mutations in colorectal cancer. J Gastrointest Oncol 2019;10:577-81. [Crossref] [PubMed]
- Batista WR, Santos G. Immunoexpression of TS, p53, COX2, EGFR, MSH6 and MLH1 biomarkers and its correlation with degree of differentiation, tumor staging and prognostic factors in colorectal adenocarcinoma: a retrospective longitudinal study. Sao Paulo Med J 2019;137:33-8. [Crossref] [PubMed]
- Moghadamnia F, Ghoraeian P, Minaeian S, et al. MicroRNA Expression and Correlation with mRNA Levels of Colorectal Cancer-Related Genes. J Gastrointest Cancer 2020;51:271-9. [Crossref] [PubMed]
- Campos-da-Paz M, Dorea JG, Galdino AS, et al. Carcinoembryonic Antigen (CEA) and Hepatic Metastasis in Colorectal Cancer: Update on Biomarker for Clinical and Biotechnological Approaches. Recent Pat Biotechnol 2018;12:269-79. [Crossref] [PubMed]
- Shan M, Tian Q, Zhang L. Serum CA50 levels in patients with cancers and other diseases. Prog Mol Biol Transl Sci 2019;162:187-98. [Crossref] [PubMed]
- Gao Y, Wang J, Zhou Y, et al. Evaluation of Serum CEA, CA19-9, CA72-4, CA125 and Ferritin as Diagnostic Markers and Factors of Clinical Parameters for Colorectal Cancer. Sci Rep 2018;8:2732. [Crossref] [PubMed]
- Kim J, Lee J, Oh JH, et al. Plasma inflammatory biomarkers and modifiable lifestyle factors associated with colorectal cancer risk. Clin Nutr 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Shaukat A, Dostal A, Menk J, et al. BMI Is a Risk Factor for Colorectal Cancer Mortality. Dig Dis Sci 2017;62:2511-7. [Crossref] [PubMed]
- Zhu J, Tan Z, Hollis-Hansen K, et al. Epidemiological Trends in Colorectal Cancer in China: An Ecological Study. Dig Dis Sci 2017;62:235-43. [Crossref] [PubMed]
- Gröschel C, Prinz-Wohlgenannt M, Mesteri I, et al. Switching to a Healthy Diet Prevents the Detrimental Effects of Western Diet in a Colitis-Associated Colorectal Cancer Model. Nutrients 2019; [Crossref] [PubMed]
- Mehta RS, Song M, Nishihara R, et al. Dietary Patterns and Risk of Colorectal Cancer: Analysis by Tumor Location and Molecular Subtypes. Gastroenterology 2017;152:1944-53.e1. [Crossref] [PubMed]
- Rada-Fernandez de Jauregui D, Evans CEL, Jones P, et al. Common dietary patterns and risk of cancers of the colon and rectum: Analysis from the United Kingdom Women's Cohort Study (UKWCS). Int J Cancer 2018;143:773-81. [Crossref] [PubMed]
- Crowe W, Elliott CT, Green BD. A Review of the In Vivo Evidence Investigating the Role of Nitrite Exposure from Processed Meat Consumption in the Development of Colorectal Cancer. Nutrients 2019; [Crossref] [PubMed]
- Aglago EK, Huybrechts I, Murphy N, et al. Consumption of Fish and Long-chain n-3 Polyunsaturated Fatty Acids Is Associated With Reduced Risk of Colorectal Cancer in a Large European Cohort. Clin Gastroenterol Hepatol 2020;18:654-666.e6. [Crossref] [PubMed]
- Carr PR, Jansen L, Walter V, et al. Associations of red and processed meat with survival after colorectal cancer and differences according to timing of dietary assessment. Am J Clin Nutr 2016;103:192-200. [Crossref] [PubMed]
- Rossi M, Jahanzaib Anwar M. Colorectal Cancer and Alcohol Consumption-Populations to Molecules. Cancers (Basel) 2018; [Crossref] [PubMed]
- Fagunwa IO, Loughrey MB, Coleman HG. Alcohol, smoking and the risk of premalignant and malignant colorectal neoplasms. Best Pract Res Clin Gastroenterol 2017;31:561-8. [Crossref] [PubMed]
- Wang Y, Yang H, Shen CJ, et al. Association between alcohol consumption and colorectal cancer risk: a case-control study in the Han Chinese population. Eur J Cancer Prev 2018;27:433-7. [Crossref] [PubMed]
- Zhenjun W, Liyuan F. Colorectal cancer screening consensus and controversy. J Clin Surg 2018;26:721-3.
- Wolf AMD, Fontham ETH, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin 2018;68:250-81. [Crossref] [PubMed]
- Rex DK, Boland CR, Dominitz JA, et al. Colorectal Cancer Screening: Recommendations for Physicians and Patients From the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2017;153:307-23. [Crossref] [PubMed]
- Maida M, Macaluso FS, Ianiro G, et al. Screening of colorectal cancer: present and future. Expert Rev Anticancer Ther 2017;17:1131-46. [Crossref] [PubMed]
- Helsingen LM, Vandvik PO, Jodal HC, et al. Colorectal cancer screening with faecal immunochemical testing, sigmoidoscopy or colonoscopy: a clinical practice guideline. BMJ 2019;367:l5515. [Crossref] [PubMed]
- Niu F, Wen J, Fu X, et al. Stool DNA Test of Methylated Syndecan-2 for the Early Detection of Colorectal Neoplasia. Cancer Epidemiol Biomarkers Prev 2017;26:1411-9. [Crossref] [PubMed]
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-86. [Crossref] [PubMed]
- Gao QY, Chen HM, Sheng JQ, et al. The first year follow-up after colorectal adenoma polypectomy is important: a multiple-center study in symptomatic hospital-based individuals in China. Front Med China 2010;4:436-42. [Crossref] [PubMed]
- Huxley N, Crathorne L, Varley-Campbell J, et al. The clinical effectiveness and cost-effectiveness of cetuximab (review of technology appraisal no. 176) and panitumumab (partial review of technology appraisal no. 240) for previously untreated metastatic colorectal cancer: a systematic review and economic evaluation. Health Technol Assess 2017;21:1-294. [Crossref] [PubMed]
- Hong DS, Morris VK, El Osta B, et al. Phase IB Study of Vemurafenib in Combination with Irinotecan and Cetuximab in Patients with Metastatic Colorectal Cancer with BRAFV600E Mutation. Cancer Discov 2016;6:1352-65. [Crossref] [PubMed]
- Wu Z, Huang M, Gong Y, et al. BRAF and EGFR inhibitors synergize to increase cytotoxic effects and decrease stem cell capacities in BRAF(V600E)-mutant colorectal cancer cells. Acta Biochim Biophys Sin (Shanghai) 2018;50:355-61. [Crossref] [PubMed]
- Corcoran RB, Andre T, Atreya CE, et al. Combined BRAF, EGFR, and MEK Inhibition in Patients with BRAF(V600E)-Mutant Colorectal Cancer. Cancer Discov 2018;8:428-43. [Crossref] [PubMed]


