Do statins improve the survival time after esophagectomy? —a propensity score matching study
Introduction
Esophageal cancer is the 8th common malignant tumor and the 6th common cancer-related cause death worldwide, especially in undeveloped regions (1,2). Esophageal squamous cell carcinoma (ESCC) is the most common type and male is about twice as likely as women (3). Esophagectomy combined with radiotherapy or/and chemotherapy is the main treatment, especially in the rapid development of minimally invasive esophagectomy (MIE) (4), however the prognosis is far from satisfaction, and the five-year survival rate of esophageal cancer is still 18.4% (5). Studies suggested statins (HMG-CoA reductase inhibitors) improve the prognosis of esophageal cancer patients (6-8). We reviewed and compared the prognosis of 27 statins users with that of 711 non-users in our database using propensity score matching analyses.
Methods
Patients data were retrospectively collected from the HIS (Hospital Information System, Version 5.0, Neusoft Co., Ltd, ShenYang, China) and the survival information was acquired by the patient returned to the hospital for postoperative reviews or telephone interviews based on a well-constructed questionnaire. The staging criteria is referred to the eighth edition of the American Joint Committee on Cancer (AJCC) Cancer Staging Manual for epithelial cancers of the esophagus and esophagogastric junction (9). Inclusion criteria includes patients with a primarily confirmed pathological diagnosis of esophageal cancer and underwent esophagectomy from January 2013 to June 2017, however patients with previous stomach surgery and/or with distant metastasis were excluded. The variables (sex, age, BMI, type II diabetes, cardiovascular comorbidity) were collected from medical records, other variables (tumor type, differentiation, cTNM) were searched from the pathologic reports from professors of pathology.
Statistical methods
All statistical analyses were operated with IBM SPSS Statistics 24.0 statistical software program (IBM SPSS Inc. Chicago, IL, USA). Continuous variables (age and BMI) were summarized as mean (SD) if normally distributed, otherwise median (IQR), moreover, T-test for normally distributed continuous variables and Wilcoxon signed-rank test for non-normally distributed variables. Categorical variables (type II diabetes, lymph node metastasis, cardiovascular comorbidity, tumor type, differentiation and cTNM) were compared using Chi-square test. Based on sex, age, BMI, type II diabetes, cardiovascular comorbidity, tumor type, differentiation and cTNM, a propensity score matching (PSM) analysis between 27 statins users and 711 non-users were conducted using SPSS. After PSM, the survival curves of the two matched groups (statins users and non-users) were plotted using Kaplan-Meier method and analyzed using Breslow test with SPSS.
Results
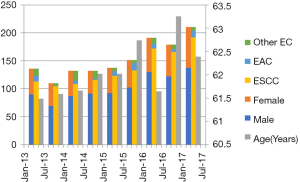
We retrospectively reviewed the data of 1,378 patients who underwent esophagectomy from January 2013 to June 2017 in our department. The characteristics of our patients were in line with that of previously reported, ESCC accounting for about 90% of the cases with a sex ratio of 2:1 (Male: Female) (3,10,11). The histological type and male-female ratio of patients with esophageal cancer did not change obviously, however, there were growth trends in the number and age of them (Figure 1).
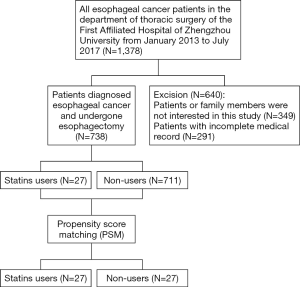
After excluding 349 patients missing (patients or family members are not interested in this experiment and refuse to participate at the telephone conversations) and 291 patients with incomplete medical record, 738 patients were eligible for further analyses, including 27 cases of statins users. Finally, 27 pairs esophageal cancer patients were matched after PSM analyses (Figure 2).
Before PSM, the sex (male), age, type II diabetes and cardiovascular comorbidity of statins users group (N=27) and non-users group (N=711) were statistically different, and there were no statistical differences between all control variables in the two groups after PSM (Table 1).
Table 1
| Variables | Before matching | P value | After matching | P value | ||
|---|---|---|---|---|---|---|
| Stains users, N=27 | Non-users, N=711 | Stains users, N=27 | Non-users, N=27 | |||
| Male (%) | 24 (88.89%) | 477 (67.09%) | 0.017 | 24 (88.89%) | 24 (88.89%) | 1.000 |
| Age [IQR] or (SD) | 66.00 [62.00, 72.00] | 63.00 [58.00, 68.00] | 0.025 | 66.04 (6.86) | 65.48 (6.89) | 0.768 |
| BMI (SD) | 24.38 (3.94) | 23.67 (3.42) | 0.289 | 24.38 (3.94) | 24.57 (3.47) | 0.849 |
| Type II diabetes (%) | 5 (18.52%) | 40 (5.63%) | 0.019 | 5 (18.52%) | 4 (14.81%) | 1.000 |
| Cardiovascular comorbidity (%) | 27 (100%) | 108 (15.19%) | 0.000 | 27 (100%) | 27 (100%) | 1.000 |
| Lymph node metastasis (%) | 11 (40.74%) | 221 (31.08%) | 0.289 | 11 (40.74%) | 12 (44.44%) | 0.783 |
| Type of tumor | 0.121 | 1.000 | ||||
| ESCC | 23 (85.19%) | 660 (92.83%) | 23 (85.19%) | 22 (81.48%) | ||
| EAC | 4 (14.81%) | 37 (5.20%) | 4 (14.81%) | 5 (18.52%) | ||
| Others | 0 (0%) | 14 (1.97%) | 0 (0%) | 0 (0%) | ||
| Differentiation of tumor (%) | 0.061 | 0.958 | ||||
| Low | 2 (7.41%) | 178 (25.04%) | 2 (7.41%) | 2 (7.41%) | ||
| Middle | 15 (55.56%) | 370 (52.04%) | 15 (55.56%) | 16 (59.26%) | ||
| High | 10 (37.04%) | 163 (22.93%) | 10 (37.04%) | 9 (33.33%) | ||
| cTNM (%) | 0.297 | 0.970 | ||||
| 0 | 2 (7.41%) | 103 (14.49%) | 2 (7.41%) | 2 (7.41%) | ||
| I | 3 (11.11%) | 114 (16.03%) | 3 (11.11%) | 2 (7.41%) | ||
| II | 11 (40.74%) | 333 (46.84%) | 11 (40.74%) | 12 (44.44%) | ||
| III | 11 (40.74%) | 160 (22.50%) | 11 (40.74%) | 11 (40.74%) | ||
| IV | 0 (0%) | 1 (0.14%) | 0 (0%) | 0 (0%) | ||
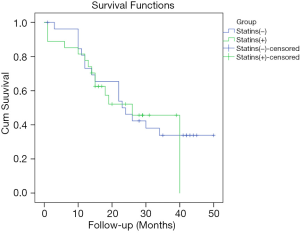
After PSM, we followed the 27 pairs patients by the questionnaire through telephone and compared survival data. With the fellow-up time of 14–50 months, the survival analysis and comparison of the two matched groups were showed in Figure 3. The survival curves were preformed using Kaplan-Meier method and there is no statistical difference between the two matched groups regarding overall survival with P values of 0.816 via Breslow (Generalized Wilcoxon) test, in other words, our data showed statins use for more than one year before esophagectomy do not improve their survival time in our center (Figure 3).
Discussion
After PSM, all statins use patients were matched with non-users and the variables of the matched groups were no statistical difference. After 50 months of follow-up, the survival analysis showed that statins use for more than one year before esophagectomy does not improve the survival time in esophageal cancer patients.
Statins are effective in regulating lipids, anti-platelet aggregation, anti-inflammation, immunosuppression and improving vascular endothelial function though competitively inhibiting the HMG-CoA reductase (12,13). Some studies reported statins use may benefit the prognosis esophageal cancer patients. A retrospective investigation in 2016 from Alexandre and colleagues (6) reported that statins reduce the esophageal cancer-specific mortality (HR 0.61, CI: 0.38–0.96) and all-cause mortality (HR 0.63, CI: 0.43–0.92). Another retrospective study in 2017 from Cardwell and colleagues (7) showed that statins use for more than one year before diagnosis, resulting in reducing the esophageal cancer-specific mortality (HR 0.88, CI: 0.79–0.99). Recently, a retrospective study in 2018 from Nguyen and colleagues (8) found that statins use reduce the cancer-related mortality (HR 0.79, CI: 0.70–0.88) and all-cause mortality (HR 0.80, CI: 0.74–0.86) in esophageal cancer patients.
Undeniably, statins uses group in our study have many great differences than general non-users group patients. There is very few patients applying statins and only about 2% esophageal cancer patients in our data use stains for more than one year before esophagectomy. Importantly, all statins users have clear cardiovascular complications in statins users group and the average age in statins users is older than general esophageal cancer patients, and these factors may lead to a worse prognosis. Although our data indicated that statins use for more than one year before esophagectomy does not improve the postoperative survival, we cannot deny that our retrospective analyses have significant limitations. Since we are a relatively high-volume center for esophagectomy, we will spare no efforts to perform further researches, determining the effects of statins in esophageal cancer.
Conclusions
Limited data showed patients use statins for more than one year before esophagectomy does not improve the postoperative survival time.
Acknowledgments
Funding: This work was supported by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2020.03.51). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This is a retrospective observational study. Our research has been ethically reviewed, and our research met the requirements of the Ethics Committee of the First Affiliated Hospital of Zhengzhou University. Informed consent was waived. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Arnold M, Soerjomataram I, Ferlay J, et al. Global incidence of oesophageal cancer by histological subtype in 2012. Gut 2015;64:381-7. [Crossref] [PubMed]
- Haverkamp L, Seesing MF, Ruurda JP, et al. Worldwide trends in surgical techniques in the treatment of esophageal and gastroesophageal junction cancer. Dis Esophagus 2017;30:1-7. [PubMed]
- Jemal A, Ward EM, Johnson CJ, et al. Annual Report to the Nation on the Status of Cancer, 1975-2014, Featuring Survival. J Natl Cancer Inst 2017;109. [PubMed]
- Alexandre L, Clark AB, Bhutta HY, et al. Association Between Statin Use After Diagnosis of Esophageal Cancer and Survival: A Population-Based Cohort Study. Gastroenterology 2016;150:854-65.e1; quiz e16-7.
- Cardwell CR, Spence AD, Hughes CM, et al. Statin use after esophageal cancer diagnosis and survival: A population based cohort study. Cancer Epidemiol 2017;48:124-30. [Crossref] [PubMed]
- Nguyen T, Khan A, Liu Y, et al. The Association Between Statin Use After Diagnosis and Mortality Risk in Patients With Esophageal Cancer: A Retrospective Cohort Study of United States Veterans. Am J Gastroenterol 2018;113:1310-8. [Crossref] [PubMed]
- Rice T, Ishwaran H, Ferguson M, et al. Cancer of the Esophagus and Esophagogastric Junction: An Eighth Edition Staging Primer. J Thorac Oncol 2017;12:36-42.
- Lagergren J, Lagergren P. Recent developments in esophageal adenocarcinoma. CA Cancer J Clin 2013;63:232-48. [Crossref] [PubMed]
- Chen W, Zheng R, Baade P, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. [Crossref] [PubMed]
- Egom EE, Hafeez H. Biochemistry of Statins. Adv Clin Chem 2016;73:127-68. [Crossref] [PubMed]
- Sirtori CR. The pharmacology of statins. Pharmacol Res 2014;88:3-11. [Crossref] [PubMed]