
Acute respiratory distress syndrome secondary to carbon dioxide gas embolism after single-port robotic-assisted perineal radical prostatectomy: a case report
Introduction
In recent years, robotic-assisted surgery has contributed to the resurgence of radical perineal prostatectomy (RPP). It has been shown in most reports that single-port robotic-assisted perineal radical prostatectomy (spRAPP) is not inferior in terms of perioperative, oncologic, and functional outcomes compared to conventional robotic-assisted radical prostatectomy (1,2). However, few complications associated with this procedure have been reported.
Acute respiratory distress syndrome (ARDS) is the leading cause of death in perioperative and intensive care settings. And its high morbidity and mortality rate have gained public attention because of its prevalence in patients with coronavirus disease 2019 (COVID-19) (3). Carbon dioxide (CO2) gas embolism, mainly resulting in significant symptoms or complications, is not common in the past. However, this has been increasingly reported due to the widespread availability of laparoscopic surgery in recent years (4,5). So far, we have not found the exact literature that reported ARDS secondary to CO2 gas embolism. In this paper, we wrote a case of ARDS secondary to CO2 gas embolism after spRAPP, the first report in the literature. We present the following article in accordance with the CARE reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-727/rc).
Case presentation
A 64-year-old man was diagnosed with prostate cancer (PCa) by transrectal prostate biopsy, with a Gleason grade of 3+4. His body mass index was 20.1 kg/m2. The blood and urine tests showed no remarkable results, and the emission computed tomography (ECT) indicated no apparent signs of bone metastases. Moreover, the cardiopulmonary function showed no obvious abnormality. In addition, he had a history of diabetes with reasonable blood sugar control. And he underwent laparoscopic appendectomy 11 years ago. The prostatectomy was scheduled 6 weeks after the prostate biopsy. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
The patient was planned to receive a spRAPP after he had informed consent. He was placed in an exaggerated lithotomy position with a 15–30° Trendelenburg tilt. A catheter was inserted into the left radial artery to monitor arterial blood pressure, and a large-bore venous catheter was indwelled into the right external jugular vein before anesthesia. Propofol (130 mg) and sufentanil (40 mg) were used to induce general anesthesia and cisatracurium (20 mg) for neuromuscular blockade. Continuous propofol (4–6 mg/kg per hour) and remifentanil (0.1–0.2 µg/kg per minute) infusions were used to maintain anesthesia. The ventilator was set to volume control mode, with a breathing frequency of 12 beats/min, a ratio of inhalation to exhalation of 1:2, and a tidal volume of 8.3 mL/kg. A 3–5 cm inverted U-shaped incision was made 2 cm above the midpoint of the line connecting the two ischial tuberosities. The disposable incision-protective retractor fixator (Angel Medical Care, Nantong, Jiangsu, China) was placed between the skin and perineal fascia to maintain airtightness. And the CO2 insufflation pressure was maintained at 12 mmHg using the AirSeal constant pressure insufflation system (ConMed, Utica, New York, USA).
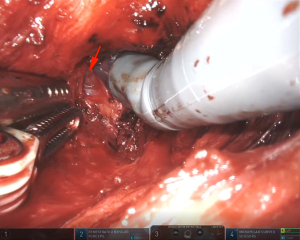
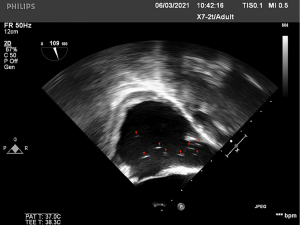
Ninety minutes after the operation, a 5-mm rupture was accidentally formed due to the venous sinus injury of the right prostate capsule (Figure 1). The view of the surgical area immediately became clear, and the bleeding of the wound stopped. However, a few minutes later, the patient’s percutaneous oxygen saturation (SpO2) decreased from 100% to 80%, and the end-tidal carbon dioxide (ETCO2) partial pressure dropped from 35 to 22 mmHg. The heart rate and arterial blood pressure were stable. The ventilator was running normally, the breathing tube was not disconnected, and there was no air leakage. The anesthesiologist immediately adjusted the inhaled air to pure oxygen, and the breathing rate increased to 14 beats/min. The breathing sounds of both lungs were normal. In addition, the aspiration was not considered because no significant amounts of sputum or vomit were found in the mouth. At the same time, the surgeon paused the surgery, retreated the AirSeal system, and packed gauze on the wound. The emergency arterial blood gas showed pH 7.206, CO2 partial pressure 72.6 mmHg, oxygen partial pressure 92.4 mmHg, and alkali remaining −1.0 mmol/L. The transesophageal echocardiography (TEE) showed persistent air bubbles in the superior vena cava and right atrium (Figure 2). After 3 minutes, the SpO2 increased to 99%. The inhaled oxygen concentration was adjusted to 65%, and the CO2 insufflation pressure was reduced to 10 mmHg. The SpO2 fluctuated at 95–99% until the end of the operation.
At the moment of the extubation, the patient’s SpO2 dropped to 88%, with shortness of breath and extensive rales in both lungs. After giving the positive pressure mask ventilation and inhaling pure oxygen, the patient’s SpO2 could reach 100%, but after changing to 45% inhaled oxygen concentration for a few minutes, the SpO2 gradually decreased to less than 90%. So, the patient was suspected of having developed adult ARDS and was transferred to the intensive care unit (ICU) for further treatment.
The patient received positive pressure ventilation with a breathing mask. The ventilator was set to S/T mode, inspired positive airway pressure (IPAP) 14 cmH2O, expiratory positive airway pressure (EPAP) 5 cmH2O, inhaled oxygen concentration 65%, and the patient’s SpO2 kept stable at 98%. After 12 hours, the respiratory therapist adjusted the respiratory parameters as IPAP 20 cmH2O, EPAP 10 cmH2O, the inhaled oxygen concentration 45%, and the patient’s SpO2 was about 99%. At the same time, the patient’s blood pressure decreased; the lowest blood pressure was 92/57 mmHg. Dopamine and norepinephrine were given simultaneously to maintain blood pressure stability. Moreover, the chest radiograph showed mild exudates in both middle lungs and pneumatization of the soft tissue of the chest wall 2 hours after the surgery (Figure 3A). And it developed into the progression of bilateral lung exudation 12 hours later (Figure 3B). Sixty hours after the surgery, the pulmonary imaging performance was the most serious (Figure 3C) and recovered at 84 hours after (Figure 3D). Pulmonary embolism was ruled out 12 hours postoperatively by lung computed tomography pulmonary angiogram (CTPA) (Figure 4). The postoperative artery blood gas results are shown in Table 1. The patient also received antibiotics, expectorant, and anticoagulant and was transferred out of the ICU 4 days after the surgery. The patient’s subsequent recovery was satisfactory and without complications, and he was discharged 9 days postoperatively.
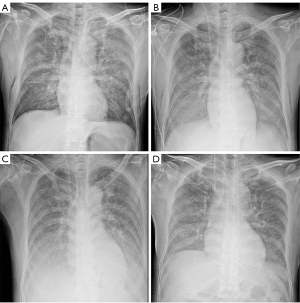
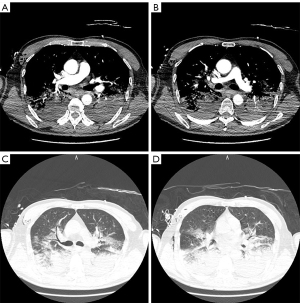
Table 1
| Variables | 2 hours | 4 hours | 8 hours | 14 hours | 30 hours | 36 hours |
|---|---|---|---|---|---|---|
| PH | 7.325 | 7.317 | 7.287 | 7.343 | 7.372 | 7.416 |
| pCO2 (mmHg) | 48.0 | 40.0 | 43.1 | 34.0 | 42.5 | 44.0 |
| pO2 (mmHg) | 61.0 | 100.0 | 74.4.0 | 86.0 | 100.4 | 115.0 |
| HCO3− (mmol/L) | 25.0 | 20.6 | 18.9 | 18.7 | 23.4 | 27.8 |
| FiO2 (%) | 65 | 65 | 65 | 45 | 45 | 45 |
| P/F | 94 | 154 | 114 | 191 | 223 | 256 |
ARDS, acute respiratory distress syndrome; CO2, carbon dioxide; PH, potential of hydrogen; pCO2, partial pressure of CO2; pO2, partial pressure of oxygen; HCO3−, bicarbonate; FiO2, fraction of inspiration oxygen; P/F, oxygenation index.
Discussion
Radical prostatectomy is the primary treatment for limited PCa. With the popularity of robotic-assisted surgery and the improvement of patients’ demands for surgical injury, rehabilitation, and aesthetics, single-port robotic-assisted radical prostatectomy is now increasingly used in clinical practice. It has been shown in some reports that spRAPP may be an alternative treatment for localized PCa patients with complex surgical histories with oncological and functional outcomes similar to those of conventional surgical approaches (6). spRAPP is a complex surgery, however, few complications associated with this procedure have been reported.
CO2 embolism is one of the most severe complications of laparoscopic surgery, although with a low incidence. However, the high mortality rate should not be underestimated. According to the reported literature, the incidence of severe CO2 embolism was less than 1%, but the mortality rate could reach 28% (7). However, it has also been shown that the overall incidence of intraoperative venous gas embolization was 38% and 69% in laparoscopic radical prostatectomy and cholecystectomy, respectively (8). One obvious mechanism of gas entering the vascular system is the open connection of the vein to the environment when the venous pressure is lower than the ambient pressure. Thus, a surgical area over the heart with low venous pressure is a risk factor for gas embolism (9). In this case, the patient was placed in a “head low” position intraoperatively, which may have increased the risk of gas embolism. Tiny CO2 bubbles in most blood vessels do not cause clinical symptoms. In addition, CO2 was easily dissolved in the blood, which caused a lot of intraoperative CO2 embolism not to be detected. In recent years, due to TEE monitoring methods, the report of CO2 embolism in laparoscopic surgery has also increased.
Intraoperative CO2 embolism is mainly seen in two situations: first, the pneumoperitoneum needle is inserted directly into a blood vessel; second, CO2 enters the circulatory system through ruptured vessels like the inferior vena cava after injury to the blood vessel during surgery (10). Generally, if gas embolism is suspected, TEE should be performed immediately. TEE is currently considered the gold standard for the detection of gas embolism with which even very small amounts of air can be reliably detected (9). As far as we know, CO2 gas embolization during spRAPP has not been reported in the literature. In this report, after the prostatic plexus was damaged, the bleeding of the surgical area stopped immediately, following the decreasing of the patient’s SpO2 and ETCO2. Still, the blood pressure and heart rate were normal. The presence of air bubbles in the superior vena cava and right atrium by TEE indicated the diagnosis of CO2 embolism. CO2 emboli could block the right ventricular outflow tract and result in decreased ETCO2, hypoxemia, hypercapnia, and high airway resistance. The clinical severity of CO2 embolism depended on the amount and velocity of gas entering the vessel. When CO2 volume reaches >2 mL/kg, it could be fetal (9).
In this case, the CO2 insufflation pressure was 12 mmHg at the time of venous plexus injury. However, we did not decrease the insufflation pressure promptly due to the lack of gas embolization experience. Instead, we continued the procedure with a clear view of the surgical area. A few minutes later, the patient suffered a CO2 gas embolism. Accordingly, the anesthesiologist adjusted the inhaled air to pure oxygen. Meanwhile, the surgeon paused the surgery, retreated the AirSeal system, and packed gauze on the wound. After the SpO2 increased to 99%, the inhaled oxygen concentration was adjusted to 65%, and the CO2 insufflation pressure was reduced to 10 mmHg until the end of the operation. Ever since this incident, we have paid more attention to the occurrence of gas embolism during spRAPP. In case of an apparent venous plexus injury, we would promptly reduce the CO2 insufflation pressure and seal the venous rupture. We have not encountered any CO2 gas embolism cases since then.
ARDS was defined as a clinical syndrome of acute hypoxemia, bilateral infiltration on chest X-ray, without left atrial hypertension. The degree of hypoxemia was evaluated by the ratio of partial pressure of oxygen to fraction of inspiration oxygen (PaO2/FiO2). To assess the prognosis of ARDS, the Berlin Definition divided the severity of ARDS into three grades: mild (200 mmHg < PaO2/FiO2 ≤300 mmHg), moderate (100 mmHg < PaO2/FiO2 ≤200 mmHg), and severe (PaO2/FiO2 ≤100 mmHg) (11). A meta-analysis of 4,188 patients with ARDS explored the relationship between the severity of ARDS and clinical outcomes (12). It indicated that in-hospital mortality rates were 27% and 32% for mild and moderate ARDS patients and 45% for those severe. Among those survivors, the mean duration of mechanical ventilation was 5 days for mild ARDS, and 7 and 9 days for moderate and severe ARDS. However, the treatment of ARDS remained a challenge. At present, the treatment was based on lung-protective mechanical ventilation to avoid additional lung damage caused by ventilator-associated lung injury. Low tidal volumes (<6 mL/kg) ventilation combined with limited inspiratory plateau pressures were required to prevent lung hyperinflation and barotrauma. In addition, a high level of positive end-expiratory airway pressure was used to avoid the lung damage caused by the shear forces generated by the periodic opening and collapse of the alveoli (13).
In this report, the patient experienced dyspnea, decreased SpO2, and unstable hemodynamics 1 hour after the operation. The chest X-ray showed bilateral pulmonary edema, and the ratio of PaO2/FiO2 was 114 mmHg. These results all suggested the occurrence of moderate ARDS. The patient received positive pressure face mask ventilation with a positive end-expiratory pressure (PEEP) of 10 cmH2O. Pulmonary imaging manifestations progressively worsened over the next 3 days, and at 60 hours reached the worst, 84 hours after surgery, the abnormal clinical manifestations gradually disappeared. In this case, the ARDS caused by CO2 embolism seemed to have a shorter course and faster recovery than those reported in the literature, which may be related to the short duration of CO2 embolism, minor damage to the lungs, easy removal of CO2 in the blood.
This case was the first report of postoperative ARDS caused by CO2 embolization during spRAPP. We believe that anesthesiologists’ and surgeons’ early detection of CO2 embolism during surgery was the key to effective treatment. Once the gas embolism leads to the occurrence of ARDS, it is necessary to treat this acute disease with intensive care intervention and comprehensive treatment based on a protective pulmonary ventilation strategy as soon as possible.
Acknowledgments
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-727/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-727/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tuğcu V, Ekşi M, Sahin S, et al. Robot-assisted radical perineal prostatectomy: a review of 95 cases. BJU Int 2020;125:573-8. [Crossref] [PubMed]
- Lenfant L, Garisto J, Sawczyn G, et al. Robot-assisted Radical Prostatectomy Using Single-port Perineal Approach: Technique and Single-surgeon Matched-paired Comparative Outcomes. Eur Urol 2021;79:384-92. [Crossref] [PubMed]
- Coleman MH, Aldrich JM. Acute Respiratory Distress Syndrome: Ventilator Management and Rescue Therapies. Crit Care Clin 2021;37:851-66. [Crossref] [PubMed]
- Zhang J, Zhao J, Fei Y, et al. Successful outcome of massive carbon dioxide embolism during laparoscopic hepatectomy. Laparoscopic, Endoscopic and Robotic Surgery 2020;3:52-5. [Crossref]
- Orhurhu VJ, Gao CC, Ku C. Carbon Dioxide Embolism. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 1, 2022.
- Minafra P, Carbonara U, Vitarelli A, et al. Robotic radical perineal prostatectomy: tradition and evolution in the robotic era. Curr Opin Urol 2021;31:11-7. [Crossref] [PubMed]
- Neudecker J, Sauerland S, Neugebauer E, et al. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc 2002;16:1121-43. [Crossref] [PubMed]
- Jin D, Liu M, Huang J, et al. Gas embolism under standard versus low pneumoperitoneum pressure during laparoscopic liver resection (GASES): study protocol for a randomized controlled trial. Trials 2021;22:807. [Crossref] [PubMed]
- Michels P, Meyer EC, Brandes IF, et al. Intraoperative vascular air embolism: Evidence for risks, diagnostics and treatment. Anaesthesist 2021;70:361-75. [Crossref] [PubMed]
- Abraham MA, Jose R, Paul MJ. Seesawing end-tidal carbon dioxide: portent of critical carbon dioxide embolism in retroperitoneoscopy. BMJ Case Rep 2018;2018:bcr-2017-219397. [Crossref] [PubMed]
- ARDS Definition Task Force. Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012;307:2526-33. [PubMed]
- Riviello ED, Kiviri W, Twagirumugabe T, et al. Hospital Incidence and Outcomes of the Acute Respiratory Distress Syndrome Using the Kigali Modification of the Berlin Definition. Am J Respir Crit Care Med 2016;193:52-9. [Crossref] [PubMed]
- Williams GW, Berg NK, Reskallah A, et al. Acute Respiratory Distress Syndrome. Anesthesiology 2021;134:270-82. [Crossref] [PubMed]


