
The efficacy of mindfulness-based stress reduction vs. standard or usual care in patients with breast cancer: a systematic review and meta-analysis of randomized controlled trials
Highlight box
Key findings
• MBSR was better than standard or usual care for relieving psychological stress, anxiety, depression, and sleep in patients with breast cancer.
What is known and what is new?
• MBSR has good results for anxiety and stress of breast cancer patients.
• MBSR also has good results for depression and sleep in patients with breast cancer.
What is the implication, and what should change now?
• Future research needs to verify the role of MBSR in breast cancer patients by using standardized intervention programs and unified evaluation methods of outcome indicators.
Introduction
Breast cancer is the most common malignant tumor with the highest incidence in women (1,2), and both the incidence and mortality of breast cancer have shown a gradual upward trend. Due to the disease itself or the adverse effects of cancer treatment, breast cancer patients are prone to negative emotions such as anxiety, depression, and stress, which seriously affect their quality of life (QOL), even lead to further deterioration and recurrence of the disease, increase the mortality of breast cancer, and seriously affect the prognosis (3,4). Therefore, improving the mental health of breast cancer patients is essential for improving the survival rate and QOL of patients (5).
Mindfulness-based stress reduction (MBSR) therapy includes mindful eating, meditation, body scanning, yoga, non-judgmental attitudes, stressors, and emotional management to enhance the ability of patients to co-exist with difficult situations, and improve their QOL (6-8). The MBSR program was developed by John Kabat Zinn of the University of Massachusetts School of Medicine (USA), and is increasingly being used as an alternative intervention for cancer patients (9,10).
Recent studies on the use of MBSR in the treatment of breast cancer patients have discussed the physical and psychological effects (11-14). MBSR has good results for anxiety and stress of breast cancer patients, but the effect on depression and QOL differed, and a unified conclusion has not yet been formed. Huang’s research (15) suggested that MBSR could also improve QOL and depression, while Zhang’s research (16) suggested that there was insufficient evidence for MBSR to improve the overall QOL. Schell’s research (17) suggested that MBSR may have little difference in anxiety or depression compared with standard or usual care in the long run. The reason for controversy may be that the number of cases included in different studies was small, and the assessment tools for mental health were different. We adopt the method of meta-analysis to expand the sample size, and conducted subgroup analysis for different evaluation tools, which can well solve the limitations of the single research.
We conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) on the effect of MBSR on the mental health and QOL of breast cancer patients to objectively evaluate the intervention effect of MBSR as the basis for the application of MBSR in the treatment of breast cancer patients. We present the following article in accordance with the PRISMA reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2530/rc).
Methods
Literature search strategy
MEDLINE (PubMed), Cochrane Database, Web of Science, Embase, China National Knowledge Infrastructure (CNKI), China Scientific Journal Database (VIP) and Wanfang Database were searched for eligible papers published up until September 2022. We used the following keywords: (I) mindfulness-based stress reduction; (II) mindfulness meditation; (III) breast cancer; (IV) breast neoplasm. The search strategy was adapted to each database using variations of the keywords, using wildcard symbols and Boolean operators to combine the terms. There were no restrictions on the language of publication. We also reviewed the reference lists of potentially relevant articles to find studies that our search strategy may have missed.
Study selection
Studies meeting the following criteria were considered for inclusion: (I) inclusion only of patients diagnosed with breast cancer; (II) RCT; (III) using MBSR as an intervention, MBSR was a systematic group decompression method that last for 6–8 weeks, which included mindfulness meditation, body awareness, mindfulness walking, mindfulness yoga and mindfulness relaxation techniques; (IV) comparison of MBSR with standard or usual care (no specific treatment or wait-list control); (V) reporting the indicators evaluating efficacy, such as depression, stress, anxiety, fatigue, sleep and QOL. The major exclusion criteria were: (I) not meeting the inclusion criteria; (II) letters, abstracts, reviews, or meta-analysis; (III) the outcomes of interest were not reported or impossible to use; (IV) duplicate article.
Data extraction
Two independent reviewers (HYW and FFL) performed the study selection, data extraction and quality assessment; and disagreements were resolved by consensus or consulting a third reviewer. The following data were extracted: name of primary author, country of study, design, number of participants in each arm, patients’ ages [mean or median and standard deviation (SD) or range if available], characteristics of intervention, and study duration.
Quality assessment
The methodological quality of the included RCTs was assessed by the Cochrane Collaboration Risk of Bias Tool (Review Manager 5.4), which included selection, performance, detection, attrition, reporting, and other biases. According to the probability of occurrence of bias risk, it can be divided into three levels: high risk, unclear risk, and low risk. After reading the full text, the author look for relevant content in the full text according to the seven items of quality evaluation. If the description was clear, it was judged as “low risk”, if the description was vague, it was judged as “unclear risk”, and if there was no relevant description, it was judged as “high risk”. For quality evaluation, two researchers (YHW and FHZ) shall independently extract data and cross check them. In case of disagreement, a third party shall be consulted for assistance in judgment.
Statistical analysis
Meta-analysis was performed by Review Manager 5.4 provided by Cochrane (Oxford, UK). The original data of outcome variables for continuous data were extracted from the included literature in the form of mean and SD. Mean difference (MD) was used for pooled continuous variables, risk ratio (RR) was used for pooled classification variables, and 95% confidence interval (CI) was used for both types of indicator. Considering that our outcome variables were tested using different questionnaires, we used the standardized mean difference (SMD) and subgroup analysis. We evaluated the degree of statistical heterogeneity and inconsistency by chi-squared test and I2 statistics. Heterogeneity was considered significant at P<0.05. In detail, I2 values of <50% indicated moderate heterogeneity, and ≥50% high heterogeneity. If it was high heterogeneity, it was necessary to explore the source of heterogeneity through subgroup analysis or sensitivity analysis. The fixed-effects model was used with the moderate heterogeneity; otherwise the random-effects model was used. We assessed potential publication bias by examining funnel plots and using Egger’s test when >10 studies were included in the meta-analysis. P value was used to detect statistical difference, and when P<0.05, the difference was statistically significant.
Results
Search process
The database search identified 974 articles, which were reduced to 925 records after removing duplicates. After screening the tittles and abstracts, an additional 831 records were excluded and a further 80 articles were excluded based on study design, insufficient relevant data, or review. Finally, 14 studies met our inclusion criteria for the present meta-analysis (18-31). The results of the search process are shown as a flowchart in Figure 1.

Characteristics of included studies
The baseline characteristics of the patients included in the meta-analysis are reported in Table 1. The total study sample size was 2,224 (range, 18–336; 1,138 in intervention group, 1,086 in control group). The follow-up time ranged from 6 weeks to 12 months. All studies were published in the English language: seven studies from the USA, and the other seven from China, UK, Demark, Sweden, Iran, and South Korea.
Table 1
| Study | Country | Study design | Treatment | No. of patients | Age (years)* | Study duration | Follow-up | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | |||||||
| Bränström, 2012 | Sweden | RCT | MBSR | Wait-list | 32 | 39 | NR | NR | Apr 2007 and Mar 2008 | 6 months | ||
| Hoffman, 2012 | UK | RCT | MBSR | Wait-list | 114 | 115 | 49.0±9.26 | 50.1±9.14 | 2005 to 2006 | 14 weeks | ||
| Lee, 2017 | South Korea | RCT | MBSR | Usual care | 9 | 9 | 52 [35–64] | 57 [37–67] | May 2013 to Aug 2013 | 8 weeks | ||
| Lengacher, 2016 | USA | RCT | MBSR | Usual care | 167 | 155 | 56.5 ± 10.2 | 57.6±9.2 | Apr 2009 to Mar 2013 | 12 weeks | ||
| Boyle, 2017 | USA | RCT | MBSR | Wait-list | 39 | 32 | 46 [28–60] | 48 [31–60] | 2014 to 2015 | 3 months | ||
| Sarenmalm, 2017 | Sweden | RCT | MBSR | Blank | 62 | 52 | 57.2±10.2 | NR | 3 months | |||
| Lengacher, 2014 | USA | RCT | MBSR | Usual care | 40 | 42 | 57.2±9.2 | Mar 2006 to Jul 2007 | 6 weeks | |||
| Witek Janusek, 2019 | USA | RCT | MBSR | Active control | 84 | 80 | 55.0±10.1 | 55.2±10.1 | Oct 2008 to Jan 2014 | 6 months | ||
| Bower, 2015 | USA | RCT | MBSR | Wait-list | 39 | 32 | 46.1 [28.4–60] | 47.7 [31.1–59.6] | NR | 3 months | ||
| Würtzen, 2013 | Denmark | RCT | MBSR | Usual care | 168 | 168 | 53.9±10.1 | 54.4±10.5 | Jun 2007 to Jul 2009 | 12 months | ||
| Lengacher, 2021 | USA | RCT | MBSR | Usual care | 165 | 155 | NR | NR | Apr 2009 to Mar 2013 | 12 weeks | ||
| Reich, 2017 | USA | RCT | MBSR | Usual care | 167 | 155 | 56.5±10.2 | 57.6±9.2 | Apr 2009 to Mar 2013 | 12 weeks | ||
| Zhang, 2017 | China | RCT | MBSR | Usual care | 30 | 30 | 48.67±8.49 | 46.00±5.12 | 2014 to 2015 | 3 months | ||
| Mirmahmoodi, 2020 | Iran | RCT | MBSR | Usual care | 22 | 22 | 44.14±11.19 | 45.62±10.11 | Aug 2017 to Nov 2019 | 8 weeks | ||
*, data are presented as median ± SD or as median [range]. RCT, randomized controlled trial; MBSR, mindfulness-based stress reduction; NR, not reported; SD, standard deviation.
Results of quality assessment
The results of methodological quality assessment of each risk of bias item for each included trial are shown in Figure 2. The quality of studies included in the review was evaluated by two independent reviewers, with differences resolved by consensus or through a third reviewer if required. A summary of all types of bias in each study is shown in Figure 3. Five studies showed the reporting bias among articles was high, and one study showed the high risk of performance bias, none of the included studies contained two high risk bias, indicating that the quality of the included articles were acceptable.
Meta-analysis for outcomes
Depression
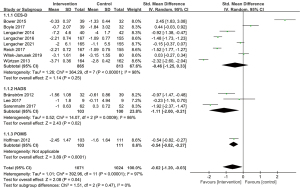
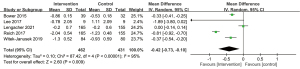
For depression, three instruments were used to assess the outcomes: the Center for Epidemiologic Studies Depression Scale (CES-D) (32), the Hospital Anxiety and Depression Scale (HADS) (33), and the Profile of Mood States score (POMS) (34). We did subgroup analyses for the different instruments, and the meta-analysis showed that although the MD in the subgroup of the CES-D had no statistical significance (P=0.25), the total SMD showed statistical significance between the intervention and control groups [SMD, −0.62; 95% CI: (−1.20, −0.03); P=0.04; random-effects model] (Figure 4).
Stress
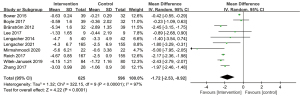
For stress, the Perceived Stress Scale (35) was used in 10 studies, with a total sample size of 1,221 patients. The intervention group showed a significantly stress reduction compared with the control group [MD, −1.72; 95% CI: (−2.53, −0.92); P<0.0001; random-effects model], and there was significant heterogeneity among the included studies (I2=97%; P<0.0001) (Figure 5).
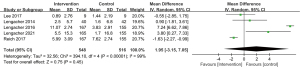
Anxiety
To assess anxiety, the State Trait Anxiety Inventory-State (STAI-S) (36), HADS, POMS, and the Revised Symptom-Checklist-90 (SCL-90-r) (37) were used in 9 studies involving 1,532 patients. The results of subgroup analyses of the four groups showed statistical significance, and the total results also showed that intervention group had a better improvement in anxiety control than the control group [SMD, −1.36; 95% CI: (−2.13, −0.60); P=0.0005; random-effects model], with significant heterogeneity between subgroups (I2=98%, P<0.00001) (Figure 6).
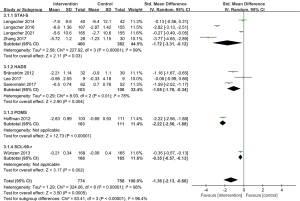
Fatigue
For fatigue, the 6 studies containing 1,413 patients were evaluated by the Fatigue Symptom Inventory and POMS. There was no significant difference between groups regarding fatigue reduction [SMD, −0.97; 95% CI: (−2.24, 0.31); P=0.14; random-effects model]. The pooled study was heterogeneous (I2=99%; P<0.00001) (Figure 7).
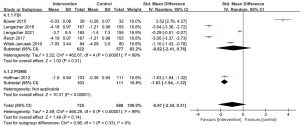
Sleep
Sleep disturbances were assessed using the instrument of the Pittsburg Sleep Quality Index in 14 included studies. The pooled results showed that the intervention group had a better improvement in sleep disturbance than the control group [MD, −0.42; 95% CI: (−0.73, −0.10); P=0.009; random-effects model], with significant heterogeneity (I2=95%; P<0.00001) (Figure 8).
QOL
For QOL, the 5 studies involving 1,064 patients were evaluated by the Medical Outcomes Study Short Form Health Survey. Meta-analysis showed no significant difference between groups regarding QOL improvement [MD, 1.95; 95% CI: (−3.15, 7.05); P=0.45; random-effects model] (Figure 9).
Publication bias
Publication bias was evaluated by visually inspecting funnel plots when at least 10 studies were included in the meta-analysis; two funnel plots were produced for the outcomes of depression and stress. Although they showed irregularity (Figure 10), the Egger’s test for quantitative detection of publication bias showed that bias was not statistically significant (depression, P=0.734; stress, P=0.282).
Discussion
Our study results showed that compared with standard or usual care, MBSR can effectively relieve psychological stress [MD, −1.72; 95% CI: (−2.53, −0.92); P<0.0001] and anxiety [SMD, −1.36; 95% CI: (−2.13, −0.60); P=0.0005] of breast cancer patients. MBSR can help patients to consciously perceive the present, guide them to establish positive physical reactions and emotions, cultivate acceptance, patience, trust, and other attitudes, and thereby improving patients’ cognitive level (38,39).
Breast cancer patients have different levels of depression, and for the loss of female characteristics after breast cancer surgery especially, the psychological response can be even higher than for the cancer (40,41). Studies have shown that providing relevant knowledge about breast cancer on websites and online consultations can effectively reduce the depression level of patients in the long term (42,43). Therefore, future research needs to include the use of digital technology. Compared with standard or usual care, we found that MBSR can improve the depression [SMD, −0.62; 95% CI: (−1.20, −0.03); P=0.04] of breast cancer patients, which is consistent with the results of other meta-analysis such as Haller et al. (44) and Hoffman et al. (19).
In addition, we found that MBSR improved the sleep status [MD, −0.42; 95% CI: (−0.73, −0.10); P=0.009] of breast cancer patients, but had no significant effect on fatigue [SMD, −0.97; 95% CI: (−2.24, 0.31); P=0.14] or QOL [MD, 1.95; 95% CI: (−3.15, 7.05); P=0.45]. In the meta-analysis of Haller et al. (44), MBSR did improve the long-term QOL. The reason for these discrepant findings may be that the process is gradual, so the short-term effect of MBSR on QOL may not be significant (43,45). Future research needs to extend the time of both intervention and follow-up, and use the internet for comprehensive nursing interventions in multiple directions to improve the long-term QOL of breast cancer patients (46,47).
Our study has some limitations. Firstly, although the MBSR included in the study was essentially based on the theoretical framework of John Kabat Zinn’s mindfulness therapy, the specific implementation schemes are not completely consistent, which may have a certain effect on heterogeneity. Secondly, the included studies were heterogeneous. The subjects were from different countries (i.e., China, the USA, South Korea, Sweden, Denmark, and Iran) where the acceptance of MBSR will differ according to cultural backgrounds. In addition, the intervention time and follow-up time in this study were relatively short. Future research should include short, medium, and long-term follow-up to observe the effect of MBSR at different stages in the lives of breast cancer patients.
Conclusions
MBSR achieved preliminary affirmation in alleviating the stress, anxiety, depression, and sleep quality of breast cancer patients. However, its effect on fatigue and QOL were not significant, and further research and verification are needed. Therefore, future research needs to analyze standardized intervention programs, and unified evaluation methods of outcome indicators to verify the effect of MBSR in breast cancer patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2530/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2530/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Adair F, Berg J, Joubert L, et al. Long-term followup of breast cancer patients: the 30-year report. Cancer 1974;33:1145-50. [Crossref] [PubMed]
- Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: an independent review. Lancet 2012;380:1778-86. [Crossref] [PubMed]
- Greer S, Morris T, Pettingale KW. Psychological response to breast cancer: effect on outcome. Lancet 1979;2:785-7. [Crossref] [PubMed]
- Huang Y, Li Q, Zhou F, et al. Effectiveness of internet-based support interventions on patients with breast cancer: a systematic review and narrative synthesis. BMJ Open 2022;12:e057664. [Crossref] [PubMed]
- Reeves MJ, Newcomb PA, Remington PL, et al. Body mass and breast cancer. Relationship between method of detection and stage of disease. Cancer 1996;77:301-7. [Crossref] [PubMed]
- Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion 2010;10:83-91. [Crossref] [PubMed]
- Chan SH, Lui D, Chan H, et al. Effects of mindfulness-based intervention programs on sleep among people with common mental disorders: A systematic review and meta-analysis. World J Psychiatry 2022;12:636-50. [Crossref] [PubMed]
- Ghandi F, Sadeghi A, Bakhtyari M, et al. Comparing the Efficacy of Mindfulness-Based Stress Reduction Therapy with Emotion Regulation Treatment on Quality of Life and Symptoms of Irritable Bowel Syndrome. Iran J Psychiatry 2018;13:175-83. [PubMed]
- Chayadi E, Baes N, Kiropoulos L. The effects of mindfulness-based interventions on symptoms of depression, anxiety, and cancer-related fatigue in oncology patients: A systematic review and meta-analysis. PLoS One 2022;17:e0269519. [Crossref] [PubMed]
- McCloy K, Hughes C, Dunwoody L, et al. Effects of mindfulness-based interventions on fatigue and psychological wellbeing in women with cancer: A systematic review and meta-analysis of randomised control trials. Psychooncology 2022;31:1821-34. [Crossref] [PubMed]
- Schellekens MP, Jansen ET, Willemse HH, et al. A qualitative study on mindfulness-based stress reduction for breast cancer patients: how women experience participating with fellow patients. Support Care Cancer 2016;24:1813-20. [Crossref] [PubMed]
- Huang J, Shi L. The effectiveness of mindfulness-based stress reduction (MBSR) for survivors of breast cancer: study protocol for a randomized controlled trial. Trials 2016;17:209. [Crossref] [PubMed]
- Zainal NZ, Booth S, Huppert FA. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: a meta-analysis. Psychooncology 2013;22:1457-65. [Crossref] [PubMed]
- Wang SJ, Chang YC, Hu WY, et al. The Comparative Effect of Reduced Mindfulness-Based Stress on Heart Rate Variability among Patients with Breast Cancer. Int J Environ Res Public Health 2022;19:6537. [Crossref] [PubMed]
- Huang HP, He M, Wang HY, et al. A meta-analysis of the benefits of mindfulness-based stress reduction (MBSR) on psychological function among breast cancer (BC) survivors. Breast Cancer 2016;23:568-76. [Crossref] [PubMed]
- Zhang Q, Zhao H, Zheng Y. Effectiveness of mindfulness-based stress reduction (MBSR) on symptom variables and health-related quality of life in breast cancer patients-a systematic review and meta-analysis. Support Care Cancer 2019;27:771-81. [Crossref] [PubMed]
- Schell LK, Monsef I, Wöckel A, et al. Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database Syst Rev 2019;3:CD011518. [Crossref] [PubMed]
- Bränström R, Kvillemo P, Moskowitz JT. A randomized study of the effects of mindfulness training on psychological well-being and symptoms of stress in patients treated for cancer at 6-month follow-up. Int J Behav Med 2012;19:535-42. [Crossref] [PubMed]
- Hoffman CJ, Ersser SJ, Hopkinson JB, et al. Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: a randomized, controlled trial. J Clin Oncol 2012;30:1335-42. [Crossref] [PubMed]
- Lee CE, Kim S, Kim S, et al. Effects of a Mindfulness-Based Stress Reduction Program on the Physical and Psychological Status and Quality of Life in Patients With Metastatic Breast Cancer. Holist Nurs Pract 2017;31:260-9. [Crossref] [PubMed]
- Lengacher CA, Reich RR, Paterson CL, et al. Examination of Broad Symptom Improvement Resulting From Mindfulness-Based Stress Reduction in Breast Cancer Survivors: A Randomized Controlled Trial. J Clin Oncol 2016;34:2827-34. [Crossref] [PubMed]
- Boyle CC, Stanton AL, Ganz PA, et al. Improvements in emotion regulation following mindfulness meditation: Effects on depressive symptoms and perceived stress in younger breast cancer survivors. J Consult Clin Psychol 2017;85:397-402. [Crossref] [PubMed]
- Kenne Sarenmalm E, Mårtensson LB, Andersson BA, et al. Mindfulness and its efficacy for psychological and biological responses in women with breast cancer. Cancer Med 2017;6:1108-22. [Crossref] [PubMed]
- Lengacher CA, Shelton MM, Reich RR, et al. Mindfulness based stress reduction (MBSR(BC)) in breast cancer: evaluating fear of recurrence (FOR) as a mediator of psychological and physical symptoms in a randomized control trial (RCT). J Behav Med 2014;37:185-95. [Crossref] [PubMed]
- Witek Janusek L, Tell D, Mathews HL. Mindfulness based stress reduction provides psychological benefit and restores immune function of women newly diagnosed with breast cancer: A randomized trial with active control. Brain Behav Immun 2019;80:358-73. [Crossref] [PubMed]
- Bower JE, Crosswell AD, Stanton AL, et al. Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial. Cancer 2015;121:1231-40. [Crossref] [PubMed]
- Würtzen H, Dalton SO, Elsass P, et al. Mindfulness significantly reduces self-reported levels of anxiety and depression: results of a randomised controlled trial among 336 Danish women treated for stage I-III breast cancer. Eur J Cancer 2013;49:1365-73. [Crossref] [PubMed]
- Lengacher CA, Gruss LF, Kip KE, et al. Mindfulness-based stress reduction for breast cancer survivors (MBSR(BC)): evaluating mediators of psychological and physical outcomes in a large randomized controlled trial. J Behav Med 2021;44:591-604. [Crossref] [PubMed]
- Reich RR, Lengacher CA, Alinat CB, et al. Mindfulness-Based Stress Reduction in Post-treatment Breast Cancer Patients: Immediate and Sustained Effects Across Multiple Symptom Clusters. J Pain Symptom Manage 2017;53:85-95. [Crossref] [PubMed]
- Zhang JY, Zhou YQ, Feng ZW, et al. Randomized controlled trial of mindfulness-based stress reduction (MBSR) on posttraumatic growth of Chinese breast cancer survivors. Psychol Health Med 2017;22:94-109. [Crossref] [PubMed]
- Mirmahmoodi M, Mangalian P, Ahmadi A, et al. The Effect of Mindfulness-Based Stress Reduction Group Counseling on Psychological and Inflammatory Responses of the Women With Breast Cancer. Integr Cancer Ther 2020;19:1534735420946819. [Crossref] [PubMed]
- Beekman AT, Deeg DJ, Van Limbeek J, et al. Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): results from a community-based sample of older subjects in The Netherlands. Psychol Med 1997;27:231-5. [Crossref] [PubMed]
- Cosco TD, Doyle F, Ward M, et al. Latent structure of the Hospital Anxiety And Depression Scale: a 10-year systematic review. J Psychosom Res 2012;72:180-4. [Crossref] [PubMed]
- Shichiri K, Shibuya M, Watanabe M, et al. Correlations between the Profile of Mood States (POMS) and the WHOQOL-26 among Japanese University Students. Health 2016;8:416-20. [Crossref]
- Ezzati A, Jiang J, Katz MJ, et al. Validation of the Perceived Stress Scale in a community sample of older adults. Int J Geriatr Psychiatry 2014;29:645-52. [Crossref] [PubMed]
- Bieling PJ, Antony MM, Swinson RP. The State-Trait Anxiety Inventory, Trait version: structure and content re-examined. Behav Res Ther 1998;36:777-88. [Crossref] [PubMed]
- Gomez R, Stavropoulos V, Zarate D, et al. Symptom Checklist-90-Revised: A structural examination in relation to family functioning. PLoS One 2021;16:e0247902. [Crossref] [PubMed]
- Nyklícek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Ann Behav Med 2008;35:331-40. [Crossref] [PubMed]
- Hatchard T, Penta S, Mioduzsewski O, et al. Increased gray matter following mindfulness-based stress reduction in breast cancer survivors with chronic neuropathic pain: preliminary evidence using voxel-based morphometry. Acta Neurol Belg 2022;122:735-43. [Crossref] [PubMed]
- Tacón AM, Caldera YM, Ronaghan C. Mindfulness-Based Stress Reduction in women with breast cancer. Fam Syst Health 2004;22:193-203. [Crossref]
- Robb SW, Benson K, Middleton L, et al. Mindfulness-based stress reduction teachers, practice characteristics, cancer incidence, and health: a nationwide ecological description. BMC Complement Altern Med 2015;15:24. [Crossref] [PubMed]
- Henderson VP, Massion AO, Clemow L, et al. A randomized controlled trial of mindfulness-based stress reduction for women with early-stage breast cancer receiving radiotherapy. Integr Cancer Ther 2013;12:404-13. [Crossref] [PubMed]
- Matchim Y, Armer JM, Stewart BR. Effects of mindfulness-based stress reduction (MBSR) on health among breast cancer survivors. West J Nurs Res 2011;33:996-1016. [Crossref] [PubMed]
- Haller H, Winkler MM, Klose P, et al. Mindfulness-based interventions for women with breast cancer: an updated systematic review and meta-analysis. Acta Oncol 2017;56:1665-76. [Crossref] [PubMed]
- Labelle LE, Campbell TS, Carlson LE. Mindfulness-based stress reduction in oncology: Evaluating mindfulness and rumination as mediators of change in depressive symptoms. Mindfulness 2010;1:28-40. [Crossref]
- Araujo RV, Fernandes AFC, Nery IS, et al. Meditation effect on psychological stress level in women with breast cancer: a systematic review. Rev Esc Enferm USP 2019;53:e03529. [Crossref] [PubMed]
- Elimimian E, Elson L, Bilani N, et al. Long-Term Effect of a Nonrandomized Psychosocial Mindfulness-Based Intervention in Hispanic/Latina Breast Cancer Survivors. Integr Cancer Ther 2020;19:1534735419890682. [Crossref] [PubMed]
(English Language Editor: K. Brown)





