
A rare case of primary spinal peripheral T cell lymphoma presents as type-B symptoms
Introduction
In non-Hodgkin’s lymphoma, bone is secondarily involved in 7–25%. While only 1% of non-Hodgkin’s lymphomas primarily originate from bone (1). Further, disease primarily from vertebral only account for 1.7% of all the primary bone lymphomas (2). Primary vertebral and spinal non-Hodgkin’s lymphoma had been described in small case series, which often presented with extradural spinal cord compression. Additionally, immunophenotype of spinal lymphoma in previous studies mostly be diffuse large B cell (3), peripheral T cell lymphoma is extremely rare. In this paper, we present an unusual case of primary spinal peripheral T cell lymphoma in a 23-year-old male, which on initial clinical and radiological examination was suggestive of a spinal infection.
Case presentation
A 23-year-old man was admitted with type-B symptoms and low back pain for more than 1 month. The type-B symptoms were presents with intermittent high fever, the highest temperature was more than 40 °C. There was no obvious heating rule, and the temperature would rise back within 2 hours after defervescence using various drugs. Night sweats and progressive weight loss were also obvious. However, low back pain was not serious which could be smothered without anodynes.
On physical examination, higher mental functions and cranial nerves were normal. Pain due to palpation and percussion of the spine was positive in fourth lumbar vertebra. Examination of motor strength revealed no deficit on both lower limbs. There were no increased or reduced reflex levels, and Babinski’s sign was negative on both sides. The general medical examination did not show any further pathology.
Laboratory examinations following hospitalized revealed no positive finding, with the exception of a significant rise in CRP and ESR. Radiographs of the lumbar spine revealed no destruction of the bone. However, computed tomography (CT) and magnetic resonance imaging (MRI) scans of the lumbar spine with contrast revealed a mass lesion (4.1 cm × 6.0 cm × 5.9 cm) at the right of L3–5 vertebra, in which inhomogeneous calcifications were observed. L4 vertebrae was destroyed and another mass lesion was observed in epidural at L4 level, which caused spinal canal stenosis. The lesions were slightly hypo-intense on T1 and T2 weighted images and displayed heterogeneous enhancement on post-contrast images. No clear boundary was observed between lesions and surrounding tissue (Figure 1). Skeletal imaging revealed abnormal isotopic accumulation at L4 vertebra. Bone marrow aspiration revealed no positive finding.

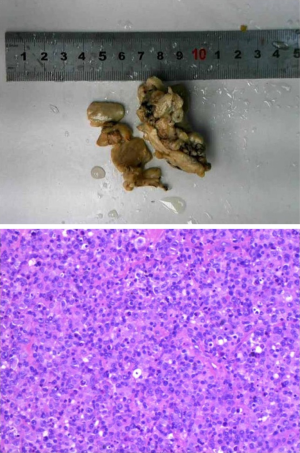
In order to identify the diagnosis, we performed a biopsy of the lesion. Unfortunately, there was no positive result, and the ongoing pain and fever forced us to open surgery eventually. Surgery was performed several days following admission. A posterior approach was used to decompress and internally fix, and excision of the lesion was performed from the anterior approach. Intraoperatively, the lesion was densely adherent to the musculus psoas major and inferior venae cava and the margins were unclear. The lesion was flesh-like without pus. The result of rapid pathologic examination described it as a round cell malignant tumor. This result was unexpected prior to surgery. Therefore, excision of the lesions was not as thorough.
Histopathological examination reported malignant lymphoma combined with large necrotic areas (Figure 2). Immunohistochemistry results were positive for cluster of differentiation CD45RO, CD3, CD2, CD45, CD43, Vim, CD38, Mum-1 and Ki67 (60%), and were negative for PLAP, CD117, CK-P, CK7, CD20, CD79a, PAX-5, CD5, CD23, CD30, ALK, CD138, Oct3/4, p53 and PAS. The diagnosis was non-Hodgkin’s lymphoma, with an unspecified peripheral T cell lymphoma immunophenotype.
Subsequently, patient received systematic examinations, including brain MRI, lung CT, abdomen CT, pelvis CT and cerebrospinal fluid examinations. All the imaging examinations failed to show additional evidence of disease. The cerebrospinal fluid was free of lymphoma cells.
According to the clinical manifestation and pathological results, the patient was staged as IE in the Ann Arbor staging system. The patient received systemic chemotherapy with cyclophosphamide, adriamycin, vincristine and prednisolone for six cycles and local radiotherapy following surgery. The fever was controlled immediately once chemotherapy was initiated. Follow up observation was regularly carried for a long time. Lumbar MRI was performed monthly, and whole body bone radionuclide imaging was performed every 3 months. Other checks will be carried out if necessary at the same time. All the disease varieties and emergency situations will be recorded and timely treated. At the follow-up of 3 months after surgery, low back pain was completely relieved. No neurological deficit was observed during the therapeutic process. No signs of lymphoma recurrence were found during follow-up. However, the patient died 1 year after the spinal surgery due to a severe pulmonary infection without an associated progression of disease.
Discussion
Non-Hodgkin’s lymphoma is a common malignant tumor, ranking among the top 10 in all human cancer types. Non-Hodgkin’s lymphoma lesions predominantly occur in the lymph nodes, spleen, thymus and other lymphoid organs, also late viscera and bones may be involved. However, primary bone non-Hodgkin’s lymphoma is extremely rare, accounting for ~1% of all non-Hodgkin’s lymphomas (1), and the vast majority occur in short bones, including the scapula, ileum, femur and tibia. Primary non-Hodgkin’s lymphoma in vertebral locations is particularly uncommon. Previous studies indicated that it accounts for only ~1.7% of the primary bone non-Hodgkin’s lymphoma (2). A strict definition of primary bone non-Hodgkin’s lymphoma is non-Hodgkin’s lymphoma cells being found in bone tissue, whilst other sites revealed no evidence of disease (4). In the present case, pre-operative MRI and CT revealed lesions in the fourth lumbar vertebra body and paravertebral tissue, which were heterogeneously enhanced in the enhanced scanning. Inter-surgery findings and pathological analysis following surgery all supported diagnosis. At the same time, the head, chest, abdomen CT, and skeletal imaging presented no metastatic lesions, and no swollen lymph nodes were observed. Therefore, the present case meets the diagnostic criteria of primary spinal lymphoma. In a previous study, the most common pathological types of spinal non-Hodgkin’s lymphoma were diffuse large B cells (3) and few T cells. To the best of our knowledge, the present case is the first to report of such a clinical presentation.
The clinical symptoms of spinal lymphoma are normally presented as local pain and as the disease progresses the lesions will extend locally to compress spinal cord or nerve root, causing neurologic damage (5). In addition to vertebral lesions, CT or MRI usually revealed lesions in lateral vertebra or spinal epidural, which can easily be confused with spinal infection or tuberculosis. Therefore, it is easy to misdiagnose early stages of spinal non-Hodgkin’s lymphoma. The present patient predominantly exhibited uncontrolled fever, and imaging features of paravertebral lesions made it was difficult to distinguish from an abscess. Therefore, it is easy to understand why doctors originally considered spinal infection prior to surgery, although the specific pathogen was not determined. When retrospectively analyzed this case, it was hypothesized that the fever was the manifestation of type-B symptoms of lymphoma. Fever was soon brought under control when chemotherapy was used, which also confirmed the diagnosis.
Previous studies revealed that secondary spinal non-Hodgkin’s lymphoma must be treated predominantly with chemotherapy, and aided with local radiotherapy. For primary spinal, non-Hodgkin’s lymphoma, certain scholars (6) suggested local excision, followed by radiotherapy. However, the standard treatment for primary spinal non-Hodgkin’s lymphoma includes both chemotherapy and radiotherapy (5,7), as performed for the present patient. Surgical intervention is necessary in cases of unclear diagnosis and acute spinal cord compression. It is worth noting that surgery is not the routine intervention in cases, which are of a clear diagnosis.
In previous reports, another common form of spinal non-Hodgkin’s lymphoma is epidural lymphoma, causing compression of the spinal cord (8), which can cause neurological deterioration. The predominant clinical manifestations can be pain, motor weakness, sensory deficits or bowl/bladder dysfunction. If allowed to continue, this may lead to paralysis of the lower limbs. In the present case, a small lesion appeared in the spinal canal at the fourth lumbar level during treatment. However, fortunately, it did not cause any symptoms of nerve injury.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.12.19). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Becker S, Babisch J, Venbrocks R, et al. Primary non-Hodgkin lymphoma of the spine. Arch Orthop Trauma Surg 1998;117:399-401. [Crossref] [PubMed]
- Rathmell AJ, Gospodarowicz MK, Sutcliffe SB, et al. Localized extradural lymphoma: survival, relapse pattern and functional outcome. The Princess Margaret Hospital Lymphoma Group. Radiother Oncol 1992;24:14-20. [Crossref] [PubMed]
- Pinheiro RF, Rocha Filho FD, Ferreira FV, et al. Primary non-Hodgkin's lymphoma of the vertebral column. Rev Bras Hematol Hemoter 2009;31:393-6. [Crossref]
- Campo E, Swerdlow SH, Harris NL, et al. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood 2011;117:5019-32. [Crossref] [PubMed]
- Ramadan KM, Shenkier T, Sehn LH, et al. A clinicopathological retrospective study of 131 patients with primary bone lymphoma: a population-based study of successively treated cohorts from the British Columbia Cancer Agency. Ann Oncol 2007;18:129-35. [Crossref] [PubMed]
- Lyons MK, O'Neill BP, Marsh WR, et al. Primary spinal epidural non-Hodgkin's lymphoma: report of eight patients and review of the literature. Neurosurgery 1992;30:675-80. [Crossref] [PubMed]
- Zhang X, Chang CK, Song LX, et al. Primary lymphoma of bone: a case report and review of the literature. Med Oncol 2011;28:202-6. [Crossref] [PubMed]
- Ho L, Valenzuela D, Negahban A, et al. Primary spinal epidural non-Hodgkin lymphoma demonstrated by FDG PET/CT. Clin Nucl Med 2010;35:487-9. [Crossref] [PubMed]


