
Hypofractionated radiotherapy for elderly breast cancer patients: from early stages disease to local palliation for unresectable disease
Introduction
The EORTC elderly task force found agreement in defining elderly patient as people being more than 70 years of age, when considering accrual in clinical trials, even though it is known that chronological age is not always corelated to the performance and functional status (1). Despite the high incidence of cancer in this group, older patients have been underrepresented in clinical trials that set the standards for care in oncology practice (2). Consequently, there is absence of clear guidelines in this population. The International Society of Geriatric Oncology (SIOG) recommendations suggested to extrapolate the evidence coming from younger population when evidence in older population is lacking (3). However patient specific factors need to be taken into consideration when making a treatment decision.
Principles in decision-making tools for radiation therapy in elderly
There is a lack of consensus on the most optimal tool to assess geriatric patients. The most commonly one used is the Comprehensive Geriatric Assessment (CGA), which helps in selecting patients for complex interventions. However, this one may be difficult to use in the routine oncology clinic. The EORTC has proposed the use of the Elderly minimum dataset data (MinDS) for selection of patients in clinical trials (1). More handy tools are required. At this time, the most pragmatic assessment is done by using age, combined with the performance status, the status of comorbities, along with the clinician’s guess estimate of 10 years or longer expectancy of life.
Omission of radiotherapy or hypofractionated radiotherapy for early breast cancer (EBC) in the elderly
Radiotherapy reduces recurrence in breast cancer. But some randomized clinical trials reported that omission of radiotherapy is a reasonable and safe option in early stage breast cancer luminal type (4-7) (Table 1). All these studies confirmed that in early stage breast cancer, luminal type and aged more than 70 years, addition of irradiation to tamoxifen reduced local recurrence by only small absolute value the risk of local recurrence and did not add any survival benefit. However, in these trials omitting radiotherapy, the experimental arm used mainly tamoxifen as adjuvant endocrine therapy. This medical treatment could be associated with toxicity in the elderly such as thromboembolisms, hot flashes and small risk of endometrial cancers. Therefore patients may not be willing to pursue 5 years of tamoxifen or the medication compliance could be quite low (8).
Table 1
| Study | Patient selection criteria | Study arms | Results and comments |
|---|---|---|---|
| Blamey et al. (BASO II trial) (4) | <2 cm, grade 1 or good prognosis special type, node negative, tamoxifen for 5 years | With or without radiotherapy and with or without tamoxifen | Local recurrence (LR) after WLE alone was 1.9% per annum (PA) versus 0.7% with RT alone and 0.8% with tamoxifen alone |
| Radiation doses 40 Gy in 15 fractions and 50 Gy in 25 fractions | |||
| Fyles et al. (5) | ≥50, T1-T2 (<5 cm), node-negative and took tamoxifen for 5 years | 40 Gy in 16 fractions. Boost 12.5 Gy in 5 fractions | • LR at 5 years in tamoxifen plus irradiation versus tamoxifen alone was 0.6% versus 7.7% |
| • In tumors <2 cm, LR was 3.6% versus 15.2% at 8 years | |||
| • Sub analysis of patients ≥60 years, LR was not significantly different (0% versus 1.2%) | |||
| Kunkler et al. (PRIME II Trial) (7) | ≥65, hormone receptor-positive, axillary node-negative, T1-T2 (<3 cm), clear margins, either grade 3 or lymphovascular invasion, (both, were not permitted) and received adjuvant endocrine treatment | 40–50 Gy in 15–25 fractions) or no radiotherapy | After median follow-up of 5 years (IQR 3.84–6.05), ipsilateral breast tumour recurrence was 1.3% (95% CI: 0.2–2.3); (n=5) in women assigned to whole-breast radiotherapy and 4·1% (2.4–5.7; n=26) in those assigned no radiotherapy (P=0.0002). 5-year overall survival was 93.9% (95% CI: 91.8–96.0) in both groups |
Elderly patient with early stage breast cancer, who deny endocrine therapy, not likely to be compliant to, or possess contra indications to endocrine therapy, or have intermediate to high risks of local recurrence, would be considered for adjuvant radiotherapy as a part of breast conserving therapy.
In some of the clinical studies mentioned above (Table 1), patients were treated with hypo-fractionated radiotherapy regimen. An updated Cochrane Systematic review concluded that for adjuvant radiotherapy post breast conserving surgery, altered fraction size regimens (greater than 2 Gy per fraction and total dose delivered over 3 weeks) had no detrimental effect on local recurrence, was associated with decreased acute toxicity and did not seem to affect breast appearance, late toxicity or patient‐reported quality‐of‐life patients (9). One of the recommendation of the Choosing Wisely American Society for Radiation Oncology (ASTRO), updated in 2018 is to propose shorter schedule (3 weeks) for whole breast radiotherapy post breast conserving surgery, in particular for women age above 50 years old. In United Kingdom and in Canada, and for women of all age, the standard regimen for whole breast radiotherapy post breast conserving surgery is hypofractionated dose of 40–42.56 Gy in 15–16 fractions (10).
Another phase 2 trial has studied use of an abbreviated hypofractionation regimens delivering 34 Gy in 10 fractions after BCS. This study had accrued patients up to 75 years of age, and reports feasibility and acceptable toxicity of shorter course radiation (11). Long term results of phase 2 studies had published experiences with 40 Gy in 10 fractions as well as 35 Gy in 7 fractions demonstrating similar toxicity and local control (12,13). The grade 2 fibrosis rate was 5.9% versus 6.7%.
Some elderly women, ages above 80 years old may find the 2–3 weeks regimens cumbersome and may decline radiotherapy treatments. Use of newer technology to reduce toxicity as well as escalate doses are being studied. Also, the use of more abbreviated hypofractionated radiotherapy have been evaluated in clinical studies.
In 2009, the Institute Curie, Paris reported its experience about 50 women aged ≥70 years with nonmetastatic stage T1 or T2 tumors treated between 1995 and 1999 by breast-conserving surgery and adjuvant abbreviated hypofractionated radiation schedule delivering a total dose of 32.5 Gy (five fractions of 6.5 Gy, once weekly) with no subsequent boost. During the same period of time, 317 women were treated with a standard radiation schedule 50 Gy in 5 weeks. With a median follow-up of 93 months, the 7-year cause-specific survival, locoregional recurrence-free survival, and metastases-free survival were not different between the 2 radiation regimen groups (14).
This type of abbreviated hypofractionated radiation schedule has been prospectively evaluating in a large randomised clinical trial (FAST trial), conducted in United Kingdom. Patients in this trial were randomly assigned to 1 of 3 regimens of whole-breast radiation therapy following breast-conserving surgery: conventional treatment with 50 Gy of radiation delivered in 25 daily 2-Gy fractions delivered over 5 weeks; or hypofractionated treatment with 1 of 2 doses: 30 Gy delivered in 5 once-weekly fractions of 6 Gy each, or 28.5 Gy delivered in 5 once-weekly fractions of 5.7 Gy each. In the 30 Gy in 5 fractions of 6 Gy arm, 16.5% of patients and in the 28.5 Gy in 5 fractions of 5.7 Gy, 13.5% of patients respectively were ≥70 years of age. At 3 years median follow-up, 28.5 Gy in 5 fractions was comparable to 50 Gy in 25 fractions, and significantly milder than 30 Gy in 5 fractions regarding the adverse effects in the breast (15).
This trial has been reported at the 2018 ASTRO annual meeting with 10 years follow-up outcomes and confirmed the initial results. No changes or only minor changes in normal tissue were observed in 88% and 86% of women at the 5- and 10-year marks, respectively. Late normal tissue effects were not statistically different between the conventional therapy group and the 5-fraction 28.5-Gy group at 5 or 10 years following treatment. Late effects to normal breast tissue were higher, however, for patients who received the 5-fraction 30-Gy regimen. On the conventional, daily-fraction arm, physicians observed normal tissue effects in 7.5% at 5 years and 9.1% at 10 years. By comparison, rates for the 5-fraction 30-Gy arm were 18.0% at 5 years (P<0.001) and 18.4% at 10 years (P=0.04) (16). It is also very interesting to note that the 10-year local relapse rate for all patients in the trial was very low at 1.3% (95% confidence interval: 0.7–2.3%), with only 10 events reported in total, balanced between the treatment groups.
The UK investigators went one step ahead and have completed a randomized trial (FAST FORWARD trial) comparing the actual standard of care for whole breast radiotherapy, 40 Gy in 15 fractions versus a 5 fractions regimen delivering a daily dose and total treatment over 5 days. In this 3-arm study the two investigational arms delivered a total dose was 27 Gy in 5 fractions (5.4 Gy/fractions) and 26 Gy in 5 fractions (5.2 Gy/fractions). Four thousand and ninety-six patients have been randomised (17). With more than 90% of patients having completed a 3-year follow-up, late effects have been modest and similar between the 3 weeks and the 1-week regimen. These interesting early outcomes need confirmation with longer follow-up assessment but are already looking quite promising with potentially some significant changes of radiotherapy management of breast cancer (18).
Partial breast radiation therapy for early breast cancer in the elderly
Partial breast irradiation (PBI) for early stage in elderly breast cancer patient treated by lumpectomy could be a very good radiotherapy alternative. The UK LOW IMPORT Study demonstrated non-inferiority of partial-breast and reduced-dose radiotherapy compared with the standard whole-breast radiotherapy, both using similar hypofractionation over 3 weeks, in terms of local relapse in a cohort of patients with early stage breast cancer, and showed equivalent or fewer late normal-tissue effects (19). There were no patients more than 70 years of age in this study. Despite this, one can assume that partial breast radiation would be equally effective and will bring some benefits in the elderly age group, as we have lower volume of breast and surrounding normal tissue irradiate. However, this PBI still delivered a dose over 3 weeks that could be challenging for some elderly women.
More abbreviated regimens have been studied and are named Accelerated PBI (APBI). For external beam irradiation, we will mainly cite the randomised phase 3 trial from the Florence University. that delivered APBI by intensity modulated radiation technique with a dose of 30 Gy in 5 fractions of 6 Gy, delivered every second day over a maximum of 2 weeks. A ratio of 22.6% of patients in the APBI arm was above 70 years of age. Despite having a biological dose (EQD2) excess of 50 Gy, the APBI arm had less acute, late toxicity and better cosmetic outcome. The ipsilateral breast recurrence and overall survival were similar (20). Other external beam APBI trials have been done, using 2 fractions a day for total of 10 fractions over 5 days. This regimen proposing 2 fractions a day could be more inconvenient for elderly women and, at least in Canada, is far to be regarded as the regimen of choice after the publication of the RAPID trial showing more adverse cosmetic outcomes following APBI (21).
Adjuvant loco-regional breast radiotherapy
A recent randomized phase 3 trial has compared a conventional versus hypofractionated radiotherapy regimen for chest wall and nodal irradiation. This study demonstrated no difference in 5 year loco-regional recurrence rates, as well in acute or late toxicity rates (22). There were no patients older than 70 years in this study. Another phase 2 study compared a different dose regimen of 36.63 Gy in 11 fractions of 3.33 Gy over 11 days to the chest wall and the draining regional lymph nodes, followed by an optional mastectomy scar boost of four fractions of 3.33 Gy was given (23).
There is lack of evidence of using hypofractionated radiotherapy for nodal irradiation in the elderly. A French retrospective studied toxicity of hypofractionated radiotherapy including nodal radiotherapy in elderly breast cancer patients (axilla, internal mammary chain and supraclavicular treated in 4%, 11% and 31% of the cases respectively) (24). The only grade 3 toxicity was 2% acute skin toxicity seen in patients who had supraclavicular nodal irradiation. A retrospective study analyzing brachial plexopathy and arm toxicity in patients treated with breast and nodal hypofractionated radiotherapy included patients up to 88 years of age in their analysis. Doses of 40 Gy in 16 fractions and 45 Gy in 20 fractions were used in this study. Compared to conventional radiation therapy arm, there was no difference in self-reported arm swelling or symptoms related to brachial plexopathy (25).
In UK, British Columbia and in Alberta, following the long-term results of UK hypofractionated trials (where a small percent of women got loco-regional radiotherapy) or following the assessment of long-term practice, hypofractionated locoregional radiotherapy over 3 weeks is standard of care. In our center and since 2018, our breast radiation group has decided to implement a locoregional breast radiotherapy care plan proposing hypofractionated dose 40 Gy in 15 fractions. This regimen is very largely use for elderly women.
For some elderly women, in particular, age more than 80 years and having a strong indication of radiation treatments, a 3 weeks regimen may still be cumbersome. Since the updates of the FAST trial and the 3 years results of the FAST forward trial previously discussed above, we have decided to implement a care plan proposing the 5 week regimen, 27 Gy in 5 fractions, 1 fraction every second day over 10 days when locoregional radiotherapy is indicated and women declined a standard 3 weeks regimen. A small number of women aged above 80 years old have been treated with very limited to nil acute side effects.
Adjuvant radiotherapy for recurrent breast cancer in elderly after previous breast conserving therapy
The rates of local recurrences within the breast cancer are becoming quite low, as shown in the 10 years update of the UK FAST trial. Occasionally such delayed recurrence may be diagnosed when the patient is in the elderly age group. The common local management for ipsilateral breast cancer recurrence is mastectomy. Despite this, published series quote ipsilateral post mastectomy recurrence rates of 3–31% (26). In addition, some elderly patients may wish to pursue the option of repeat breast conserving surgery in case of recurrence. The RTOG 1014 was a phase 2 study analyzing repeat breast conserving therapy in the form of breast conserving surgery followed by partial breast re-irradiation (26). This study included patients up to 86 years of age (median age 68 years) who were treated with “hyper” fractionation. The ipsilateral breast recurrence at 3 years was 3.7% and 6.9% late toxicity. The role of partial breast re-irradiation using hypofractionation needs to be studied in this population. I can be assumed that the local control should be similar with hypofractionation, but late toxicity could be potentially higher.
Palliative hypofractionated radiotherapy for locally advanced unresectable breast cancer
As the literature is scarce in this setting, consisting of mainly retrospective studies, various radiation regimen and also various use of medical treatments (i.e., chemotherapy), there is no clear consensus on the dose of palliative radiotherapy for unresectable breast cancer (27-29). The commonly used palliative fractionated radiotherapy regimen are similar to the ones used for other sites (i.e., bone, brain) and have proposed 20 to 30 Gy in 5 to 10 fractions but up to 40–50 Gy in 15–20 fractions, depending on the medical and performance status of the patient.
Padilha et al. have used a palliative hypofractionated RT, named “flashed scheme” with a dose of 13 Gy in 2 fractions over 3 days and 26 Gy in 4 fractions over 5 weeks, in patients with average age of 80.7+5.9 years. Surgery was held in 53% of patients and 50.6% had no evidence of progression (30).
Long term outcomes of an abbreviated hypofractionated regimen with hormone therapy and no surgery, prescribed to elderly patients (median age of 83 years) has been reported by a French group. Between 1987 and 1999, 115 patients non metastatic were treated with definitive once weekly hypofractionated radiotherapy associated with hormonal therapy. Radiation was delivered as once-a-week, 6.5 Gy for a total breast dose of 32.5 Gy in five fractions, followed with 1–3 fractions of 6.5 Gy to the tumour site. With a median follow-up of 41 months, the 5-year local progression-free rate was 78%. The corresponding cause-specific survival was 71%, the 5-year overall survival was 38%. Tumour size and performance status were the independent factors found affecting the overall survival. The breast late reactions occurred in 46 patients and were mild to moderate in 87% of these patients (31).
In our centre and in particular for women above 80 year of age having unresectable breast cancer due to comorbidities, we have used 30 Gy in 5 fractions to the whole breast and/or nodes, once a week, followed by 6 Gy boost to the primary breast tumor with acceptable local control and minimum toxicity.
It is difficult to launch and run a randomized study to evaluate different regimen of radiation for elderly breast cancer population getting this specific locally advanced non resectable primary, as its incidence is quite in low range. However, it would be possible through a multi institutions group, to define a hypofractionated abbreviated or not and prospectively evaluate the clinical outcomes.
Considering radiation toxicity in the elderly breast cancer patient
During any discussion regarding radiation therapy in the elderly patient, it is pertinent to include information on toxicity and its impact on quality of life. As elderly patient’s concept of quality of life may differ from patient to patient, based on socio-cultural and geographical differences, it may be important to take this into consideration. The planning dose volume constraints are still extrapolated from those that are published in the younger age group. Even with the use higher precision planning, including IMRT, which has partly reduced the risk of acute and subacute toxicity, these patients can still have early or moderately late skin and soft tissue toxicities including dermatitis, subcutaneous fibrosis and mastalgia. There is very little published on late toxicity in the elderly breast cancer. A Danish study with 35,000 breast cancer patients who were treated with radiotherapy demonstrated no difference in late cardiac toxicity in the left sided breast cancer patients compared to right sided breast patients in the age group 60–79 years (32).
Conclusions
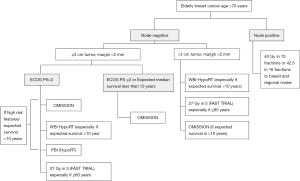
Larger consensus on validated and user-friendly tools to assess geriatric patients are indicated to determine the optimal radiotherapy treatments for elderly breast cancer patients. When breast radiation therapy is indicated in women with elderly breast cancer, a 3 weeks regimen (40–42.6 Gy in 15–16 fractions) seems very appropriate and is usually well tolerated. There is a group of elderly patients (i.e., above 80 years but still fit), where a 3 weeks regimen could be cumbersome and that would benefit for 5 fractions treatment. In Figure 1 we have proposed an algorithm for the use of radiotherapy in elderly patients with breast cancer. In general, for the elderly breast cancer population, there is a need for prospective clinical data and more evidence-based management guidelines that could be achieved through a collaborative working group.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Vincent Vinh-Hung and Nam P Nguyen) for the series “Radiotherapy for Breast Cancer in Advanced Age” published in Translational Cancer Research. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2019.09.20). The series “Radiotherapy for Breast Cancer in Advanced Age” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pallis AG, Ring A, Fortpied C, et al. Eortc workshop on clinical trial methodology in older individuals with a diagnosis of solid tumors. Ann Oncol 2011;22:1922-6. [Crossref] [PubMed]
- Hutchins LF, Unger JM, Crowley JJ, et al. Underrepresentation of Patients 65 Years of Age or Older in Cancer-Treatment Trials. N Engl J Med 1999;341:2061-7. [Crossref] [PubMed]
- Biganzoli L, Wildiers H, Oakman C, et al. Management of elderly patients with breast cancer: Updated recommendations of the International Society of Geriatric Oncology (SIOG) and European Society of Breast Cancer Specialists (EUSOMA). Lancet Oncol 2012;13:e148-60. [Crossref] [PubMed]
- Blamey RW, Bates T, Chetty U, et al. Radiotherapy or tamoxifen after conserving surgery for breast cancers of excellent prognosis: British Association of Surgical Oncology (BASO) II trial. Eur J Cancer 2013;49:2294-302. [Crossref] [PubMed]
- Fyles AW, McCready DR, Manchul LA, et al. Tamoxifen with or without breast irradiation in women 50 years of age or older with early breast cancer. N Engl J Med 2004;351:963-70. [Crossref] [PubMed]
- Hughes KS, Schnaper LA, Bellon JR, et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: Long-term follow-up of CALGB 9343. J Clin Oncol 2013;31:2382-7. [Crossref] [PubMed]
- Kunkler IH, Williams LJ, Jack WJL, et al. Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): A randomised controlled trial. Lancet Oncol 2015;16:266-73. [Crossref] [PubMed]
- Amir E, Seruga B, Niraula S, et al. Toxicity of adjuvant endocrine therapy in postmenopausal breast cancer patients: A systematic review and meta-analysis. J Natl Cancer Inst 2011;103:1299-309. [Crossref] [PubMed]
- Hickey BE, James ML, Lehman M, et al. Hypofractionated radiation therapy for early breast cancer. Cochrane Database Syst Rev 2016;CD003860. [PubMed]
- Hahn C, Kavanagh B, Bhatnagar A, et al. Choosing Wisely: The American Society for Radiation Oncology’s Top 5 list. Pract Radiat Oncol 2014;4:349-55. [Crossref] [PubMed]
- Yadav BS, Sharma SC. A Phase 2 Study of 2 Weeks of Adjuvant Whole Breast/Chest Wall and/or Regional Nodal Radiation Therapy for Patients With Breast Cancer. Int J Radiat Oncol Biol Phys 2018;100:874-81. [Crossref] [PubMed]
- Vinante L, Avanzo M, Furlan C, et al. Ten daily fractions for partial breast irradiation. Long-term results of a prospective phase II trial. Breast J 2019;25:243-9. [Crossref] [PubMed]
- Trovo M, Avanzo M, Vinante L, et al. Seven fractions to deliver partial breast irradiation: The toxicity is Low. Radiat Oncol 2017;12:86. [Crossref] [PubMed]
- Kirova YM, Campana F, Savignoni A, et al. Breast-Conserving Treatment in the Elderly: Long-Term Results of Adjuvant Hypofractionated and Normofractionated Radiotherapy. Int J Radiat Oncol Biol Phys 2009;75:76-81. [Crossref] [PubMed]
- FAST Trialists group. First results of the randomised UK FAST Trial of radiotherapy hypofractionation for treatment of early breast cancer (CRUKE/04/015). Radiother Oncol 2011;100:93-100. [Crossref] [PubMed]
- Brunt AM, Haviland J, Sydenham M, et al. FAST Phase III RCT of Radiotherapy Hypofractionation for Treatment of Early Breast Cancer: 10-Year Results (CRUKE/04/015). Int J Radiat Oncol 2018;102:1603-4. [Crossref]
- Brunt AM, Wheatley D, Yarnold J, et al. Acute skin toxicity associated with a 1-week schedule of whole breast radiotherapy compared with a standard 3-week regimen delivered in the UK FAST-Forward Trial. Radiother Oncol 2016;120:114-8. [Crossref] [PubMed]
- Brunt AM, Haviland J, Sydenham M, et al. OC-0595: FAST-Forward phase 3 RCT of 1-week hypofractionated breast radiotherapy:3-year normal tissue effects. Radiother Oncol 2018;127:S311-2. [Crossref]
- Coles CE, Griffin CL, Kirby AM, et al. Partial-breast radiotherapy after breast conservation surgery for patients with early breast cancer (UK IMPORT LOW trial): 5-year results from a multicentre, randomised, controlled, phase 3, non-inferiority trial. Lancet 2017;390:1048-60. [Crossref] [PubMed]
- Livi L, Meattini I, Marrazzo L, et al. Accelerated partial breast irradiation using intensity-modulated radiotherapy versus whole breast irradiation: 5-year survival analysis of a phase 3 randomised controlled trial. Eur J Cancer 2015;51:451-63. [Crossref] [PubMed]
- Whelan T, Julian J, Levine M, et al. Abstract GS4-03: RAPID: A randomized trial of accelerated partial breast irradiation using 3-dimensional conformal radiotherapy (3D-CRT). Cancer Res 2019;79:Abstract GS4-03.
- Wang SL, Fang H, Song YW, et al. Hypofractionated versus conventional fractionated postmastectomy radiotherapy for patients with high-risk breast cancer: a randomised, non-inferiority, open-label, phase 3 trial. Lancet Oncol 2019;20:352-60. [Crossref] [PubMed]
- Khan AJ, Poppe MM, Goyal S, et al. Hypofractionated postmastectomy radiation therapy is safe and effective: First Results from a prospective phase II trial. J Clin Oncol 2017;35:2037-43. [Crossref] [PubMed]
- Doré M, Cutuli B, Cellier P, et al. Hypofractionated irradiation in elderly patients with breast cancer after breast conserving surgery and mastectomy: Analysis of 205 cases. Radiat Oncol 2015;10:161. [Crossref] [PubMed]
- Leong N, Truong PT, Tankel K, et al. Hypofractionated Nodal Radiation Therapy for Breast Cancer Was Not Associated With Increased Patient-Reported Arm or Brachial Plexopathy Symptoms. Int J Radiat Oncol Biol Phys 2017;99:1166-72. [Crossref] [PubMed]
- Arthur DW, Winter KA, Kuerer HM, et al. NRG Oncology–Radiation Therapy Oncology Group Study 1014: 1-Year Toxicity Report From a Phase 2 Study of Repeat Breast-Preserving Surgery and 3-Dimensional Conformal Partial-Breast Reirradiation for In-Breast Recurrence. Int J Radiat Oncol Biol Phys 2017;98:1028-35. [Crossref] [PubMed]
- Le Scodan R, Stevens D, Brain E, et al. Breast cancer with synchronous metastases: Survival Impact of exclusive locoregional radiotherapy. J Clin Oncol 2009;27:1375-81. [Crossref] [PubMed]
- Budach W, Matuschek C, Bölke E, et al. DEGRO practical guidelines for radiotherapy of breast cancerV: Therapy for locally advanced and inflammatory breast cancer, as well as local therapy in cases with synchronous distant metastases. Strahlenther Onkol 2015;191:623-33. [Crossref] [PubMed]
- Yee C, Alayed Y, Drost L, et al. Radiotherapy for patients with unresected locally advanced breast cancer. Ann Palliat Med 2018;7:373-84. [Crossref] [PubMed]
- Padilha M, Gonçalves S, Fardilha C, et al. Hypofractionation in locally advanced breast cancer: “Flash” scheme. Acta Med Port 2013;26:98-101. [PubMed]
- Courdi A, Ortholan C, Hannoun-Lévi JM, et al. Long-term results of hypofractionated radiotherapy and hormonal therapy without surgery for breast cancer in elderly patients. Radiother Oncol 2006;79:156-61. [Crossref] [PubMed]
- McGale P, Darby SC, Hall P, et al. Incidence of heart disease in 35,000 women treated with radiotherapy for breast cancer in Denmark and Sweden. Radiother Oncol 2011;100:167-75. [Crossref] [PubMed]


