
A promising road in colorectal cancer treatment: personalized immunotherapy based on molecular and immune classification system
Immunotherapy has increasingly proven to be a key treatment modality that can make a significant impact on the lives of many cancer patients. In particular, immune checkpoint inhibitors targeting the programmed cell death protein 1 (PD-1) pathway have led to remarkable clinical benefits in various cancers, including melanoma and lung cancer, and active investigations are ongoing to expand their therapeutic utility in other cancer types (1). In fact, several clinical trials have revealed a link between high somatic mutation prevalence and the clinical success in PD-1 axis blockade. Considering that colorectal cancers (CRC) are known to have very high rates of somatic mutations in comparison to other solid cancers (2), the potential of immunotherapeutic agents in treating patients with CRC is encouraging (3,4). However, in harnessing the full potential of immunotherapy, several key questions need to be addressed: which patients are to be treated in order to maximize therapeutic benefits; how would immunotherapy be combined with other treatment modalities; and how would optimal biological dosing be determined with minimal toxicity as well as cost-effectiveness (5).
Recently, Becht and colleagues conducted transcriptomic analyses of the immune, fibroblastic and angiogenic microenvironment using 1,388 CRC samples from three independent discovery and validation cohorts, and MCP-counter algorithm that can assess immune and stromal cell infiltration (6). Their objective was to further integrate the immune and inflammatory microenvironment data within the four recently proposed CRC consensus molecular subtypes (CMSs): CMS1 [microsatellite instability (MSI) immune], CMS2 (canonical), CMS3 (metabolic), and CMS4 (mesenchymal) (7). Their results revealed a high degree of correlation between CMS classifications and microenvironmental signatures, yielding both expected and unexpected results. The good-prognosis CMS1 group was found to have high expression of immune signatures. Surprisingly, the CMS4 group with the worst prognosis of the four subgroups displayed high expression of immune signatures as well. Substantial contextual differences, however, were noted between the CMS1 and CMS4 groups. While the CMS1 group was characterized by overexpression of genes specific to cytotoxic lymphocytes, the CMS4 group showed overexpression of markers of lymphocytes and cells of monocytic origin with strong angiogenic and inflammatory components. On the other hand, the CMS2 and CMS3 groups were found to display low immune and inflammatory signatures (Table 1).
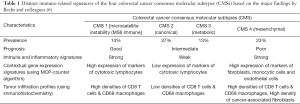
Full table
As discussed by Becht and colleagues (6), their findings may provide important insights into clinical investigations of immunotherapeutic agents in patients not only with CRC and but also other types of cancers. Relevant to this, Le and colleagues recently reported the results of a Phase II trial with pembrolizumab, an anti-PD-1 immune checkpoint inhibitor, in 41 patients randomized into three cohorts: cohort A with mismatch-repair (MMR) deficient CRC patients, cohort B with MMR proficient CRC patients, and cohort C with MMR deficient non-CRC patients (4). In this study, the immune-related objective response rates were markedly dependent upon the MMR status; 40% (4 of 10 patients) and 0% (0 of 18 patients) for cohort A (MMR-deficient CRC) and cohort B (MMR-proficient CRC), respectively. While the results from this study support the predictive value of the MMR status for the response to pembrolizumab, molecular and immune classification systems with more refined and dynamic markers may offer better predictive power in identifying responders and non-responders to anti-immune checkpoint therapies than the MMR status alone. Especially in the cases of CMS2 (canonical) and CMS3 (metabolic) groups, other strategies will be needed to optimize their treatment outcomes since the two were characterized to have low immune signatures by Becht and colleagues (6). Specifically within the immunotherapy context, other approaches such as adoptive T cell therapies may be more suitable for patients with CMS2 and CMS3 CRC. In addition, how more conventional anticancer therapies such as chemotherapy or radiation therapy interact with immune therapies or alter the immune milieu within an individual’s cancer have not been fully investigated and may also impact the treatment of these CRC subtypes.
As reflected by an almost 10-fold jump in overall median survival from what it was in the initial stages of CRC research in the 1960’s, major advances have been made in CRC therapy over the past decades. From the introduction of 5-fluorouracil (5-FU) and other chemotherapies to the gradual evolution of targeted therapies and immunotherapies, the past fifty years of CRC research have witnessed a number of pivotal moments. As suggested by Becht and colleagues (6), integrated molecular and immune classifications of CRC and their application to personalized CRC therapy may be a noteworthy advancement in guiding the selection of therapies that can maximize clinical benefits while minimizing unwanted side effects to CRC patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Zhen-Yu Lin, MD (Cancer center, Union hospital, Huazhong University of Science and Technology, Wuhan, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.06.30). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gentzler R, Hall R, Kunk PR, et al. Beyond melanoma: inhibiting the PD-1/PD-L1 pathway in solid tumors. Immunotherapy 2016;8:583-600. [Crossref] [PubMed]
- Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 2003;349:247-57. [Crossref] [PubMed]
- Brahmer JR, Drake CG, Wollner I, et al. Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol 2010;28:3167-75. [Crossref] [PubMed]
- Le DT, Uram JN, Wang H, et al. PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N Engl J Med 2015;372:2509-20. [Crossref] [PubMed]
- Jackie Oh S, Han S, Lee W, et al. Emerging immunotherapy for the treatment of esophageal cancer. Expert Opin Investig Drugs 2016;25:667-77. [Crossref] [PubMed]
- Becht E, de Reyniès A, Giraldo NA, et al. Immune and stromal classification of colorectal cancer is associated with molecular subtypes and relevant for precision immunotherapy. Clin Cancer Res 2016; [Epub ahead of print]. [Crossref] [PubMed]
- Guinney J, Dienstmann R, Wang X, et al. The consensus molecular subtypes of colorectal cancer. Nat Med 2015;21:1350-6. [Crossref] [PubMed]


